Last Updated on November 27, 2025 by Bilal Hasdemir
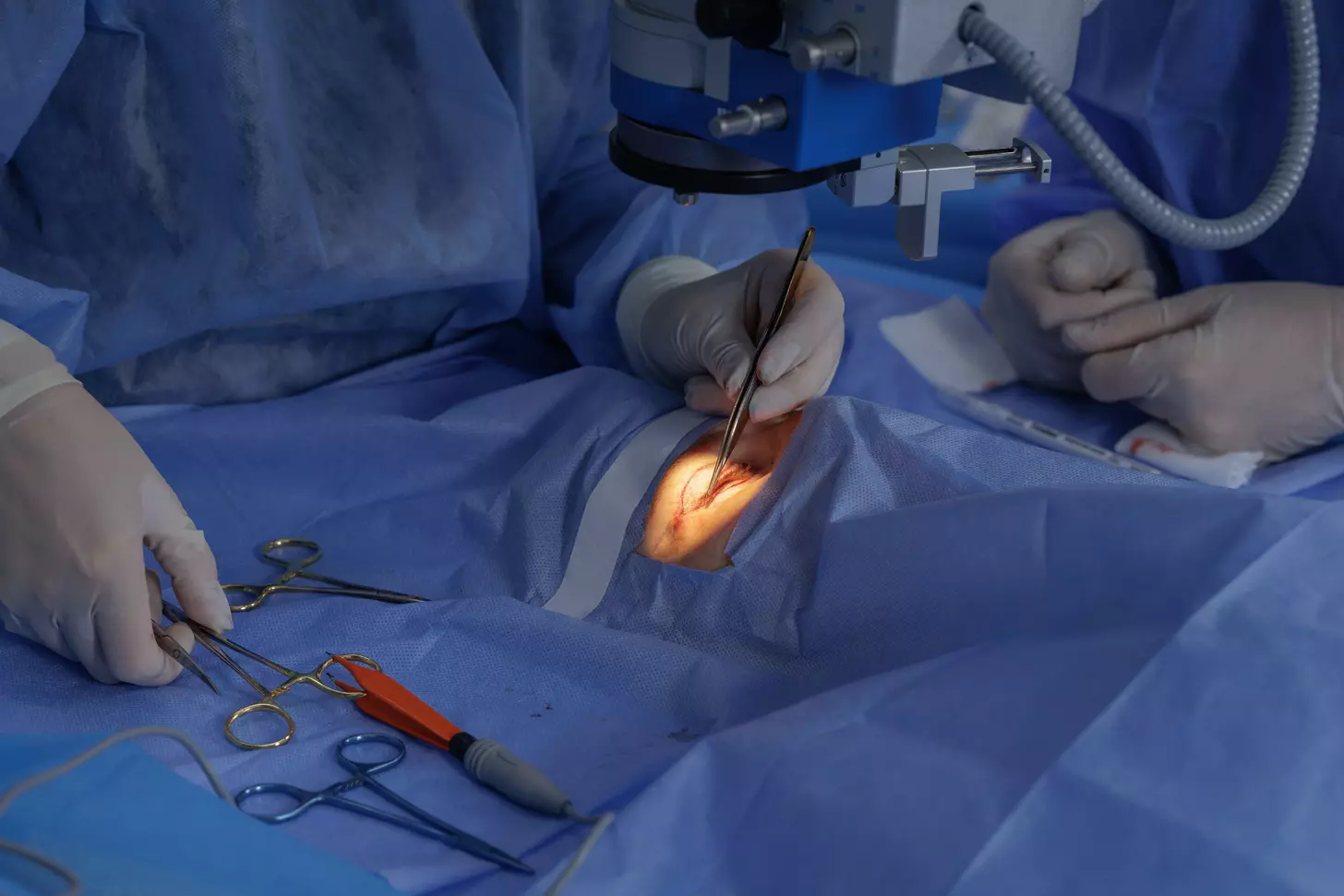
At Liv Hospital, we know how vital it is to find the right people for CABG surgery. This big surgery helps by bypassing blockages in the coronary arteries. It uses veins or arteries to get blood flowing to the heart again.
CABG is a lifesaver for those with serious heart disease. It greatly boosts survival chances and improves life quality. We’ll talk about the main indications for CABG in the next parts.
Knowing the key criteria for CABG is key for top-notch heart care. Our team is all about giving the best healthcare. We also offer full support for patients from abroad.
CABG surgery is a complex procedure to fix blocked coronary arteries. It helps restore blood flow to the heart. This is key for those with severe heart disease, easing symptoms and boosting heart health.
CABG surgery uses a healthy blood vessel to bypass blocked arteries. This vessel can come from the leg or chest. It ensures blood keeps flowing to the heart muscle, lowering heart attack risks and easing pain.
The surgery is done under general anesthesia. It can be on-pump or off-pump, depending on the patient and surgeon. Coronary bypass surgery has evolved to improve results over time.
Bypass grafting is a surgical method to bypass blocked arteries. It connects a graft vessel to the artery above and below the blockage. This restores blood flow to the heart.
The graft can be an artery or a vein. Arterial grafts, like the internal mammary artery, are preferred for their better long-term success rates.
Knowing CABG terms is vital for patients and healthcare teams. Key terms include:
| CABG Terminology | Description |
|---|---|
| On-pump CABG | Surgery using a heart-lung machine |
| Off-pump CABG | Surgery without a heart-lung machine |
| Arterial Graft | Graft taken from an artery |
| Venous Graft | Graft taken from a vein |
Evidence-based medicine is key in deciding if CABG is right for a patient. The choice to have CABG surgery looks at the patient’s health, medical history, and how bad their heart disease is.
Guidelines for CABG come from solid research, like clinical trials and studies. These guidelines help doctors find out who will most likely get better from CABG. The American Heart Association (AHA) and the American College of Cardiology (ACC) update these guidelines often to keep up with new findings.
The main reasons for CABG, as the guidelines say, are:
Choosing who gets CABG is a detailed process. It looks at how bad the heart disease is, how well the heart is working, and if there are other health issues. CABG criteria make sure the surgery is for those who will get the most help.
Doctors think about several things when deciding on CABG for a patient:
CABG is a big help for the right patients, but it’s not without risks. Risks include stroke, infection, and graft failure. The choice to have CABG must weigh these risks against the benefits, like living longer and feeling better.
The main benefits of CABG are:
In summary, CABG is recommended based on solid guidelines. Choosing the right patients and carefully considering risks and benefits are key to good results.
Significant left main coronary artery stenosis is a major reason for CABG surgery. This condition narrows the left main coronary artery. This artery is key for blood supply to a big part of the heart.
To diagnose significant left main coronary artery stenosis, we use a few steps. First, we do a clinical assessment. Then, we use coronary angiography to see how bad the stenosis is.
Other tests like stress testing and cardiac imaging help us understand the damage. They show how much the heart is affected.
Without treatment, the risk of death is high for those with left main stenosis. Research shows that untreated patients face a higher risk of heart problems and death. We stress the need for quick action to save lives.
CABG greatly improves survival chances for left main stenosis patients. It bypasses the blocked area, ensuring blood flow to the heart. This reduces heart risks and boosts long-term survival.
Guidelines strongly recommend CABG for significant left main stenosis. It’s a key treatment in medical practice.
Our talk highlights CABG’s vital role in treating left main coronary artery stenosis. Understanding diagnosis, risks, and benefits of CABG helps us give the best care to these patients.
When coronary artery disease affects three vessels, the outlook is much worse without treatment. This condition, known as three-vessel coronary artery disease, shows severe blockages in three main arteries. It’s a serious and potentially deadly situation.
Three-vessel disease is diagnosed when blockages are found in the right coronary artery, the left anterior descending artery, and the left circumflex artery. Or, blockages are found in their major branches. This means the heart’s blood supply is badly affected.
Having three-vessel coronary artery disease increases the risk of heart attacks and death. Research shows that patients with this condition face a worse prognosis than those with single or double-vessel disease.
Prognostic factors include how much the heart is affected, the heart’s function, and other health issues like diabetes. These factors help doctors understand the risk and decide on the best treatment.
Coronary artery bypass grafting (CABG) can improve survival and reduce symptoms in patients with three-vessel disease. The benefits of CABG are clear in complex cases where medicine alone is not enough.
CABG helps by improving blood flow to the heart. This can greatly enhance a patient’s quality of life. The procedure uses grafts, often from the patient’s own veins or arteries, to bypass the blocked areas.
Every patient’s situation is different. The choice to have CABG depends on a detailed review of their health, disease extent, and other factors.
Two-vessel disease with involvement of the proximal LAD is a key reason for choosing Coronary Artery Bypass Graft (CABG) surgery. This choice can lead to better long-term results. We see two-vessel disease, and more so when the LAD is involved, as a complex issue. It needs a thoughtful approach to treatment.
The LAD artery is vital for the heart. Proximal LAD involvement means the blockage is close to the start. This can cause more heart damage if not treated right.
We know that the LAD’s involvement in two-vessel disease raises the risk of heart problems. Choosing the right treatment is very important.
Getting a correct diagnosis is key to understanding the heart disease’s extent. We use tools like coronary angiography to see the blockages. Coronary angiography gives us clear images of the arteries. This helps us see how much of the LAD is affected.
Studies show that CABG can lead to better survival and fewer heart problems than just medicine for those with two-vessel disease and LAD involvement. We look at each patient’s risk, symptoms, and what they want when choosing between CABG and medicine. CABG can not only save lives but also improve quality of life by reducing symptoms and the need for more treatments.
In summary, two-vessel disease with LAD involvement is a strong reason for CABG. Evidence supports better results with CABG over medicine for the right patients. We focus on a treatment plan that fits each patient’s needs and wishes.
Left main equivalent disease is when both the LAD and circumflex arteries have a lot of blockage. This is a big risk for patients because it affects a lot of heart muscle.
Left main equivalent disease means there are big blockages in both the LAD and circumflex arteries. This is serious because it can harm a big part of the heart muscle, leading to severe problems.
Finding left main equivalent disease can be hard because symptoms vary and non-invasive tests have limits. Coronary angiography is key for accurate diagnosis. A study on NCBI shows that getting the diagnosis right is vital for treatment.
For left main equivalent disease, CABG is usually the best choice because it has shown to improve survival. The aim of CABG is to get blood flowing to the heart again, which helps survival and reduces symptoms. Choosing the right graft sites is important, and the internal thoracic artery is often the best choice.
After CABG for left main equivalent disease, patients often see big improvements in survival and quality of life. It’s important to have a team approach in treating these patients, looking at both surgery and other options.
Disabling angina that doesn’t get better with medicine is a strong reason for CABG. Angina makes it hard to live a normal life. When medicine doesn’t work, other treatments are needed.
Refractory angina means angina symptoms don’t go away with the best medicine. It makes life hard and lowers quality of life. It’s not just about symptoms but how it affects daily life.
Life is tough for those with refractory angina. Simple tasks are scary because of the risk of angina. CABG can help by making life easier and improving how well you can do things.
Research shows CABG helps a lot. It makes symptoms better and life quality higher. Being able to do more things makes you feel better physically and mentally.
CABG really helps with angina symptoms. It fixes the blocked arteries, improving blood flow to the heart. This reduces angina episodes.
| Symptom | Pre-CABG | Post-CABG |
|---|---|---|
| Angina Episodes | Frequent | Reduced |
| Quality of Life | Poor | Improved |
| Functional Capacity | Limited | Enhanced |
Our findings show CABG greatly improves symptoms and life quality for those with disabling angina. It not only makes life better but can also help you live longer.
There are more reasons to consider Coronary Artery Bypass Graft (CABG) surgery. These reasons help identify who can benefit most from CABG. It improves their chances of living longer and better.
Non-invasive tests show if a patient has significant ischemia. Those with extensive ischemia face a higher risk of heart problems. CABG can help by reducing ischemia and improving blood flow to the heart.
CABG is a good option for those who can’t or shouldn’t have PCI. These patients often have complex heart arteries or other reasons why PCI is not safe or effective.
Diabetics with heart disease in many arteries benefit from CABG. Studies show CABG can help them live longer and avoid more surgeries.
Those with heart failure due to blocked arteries and some heart muscle that can recover also benefit from CABG. This surgery can improve heart function and outcomes.
Other cases might need CABG too. This includes people with ongoing chest pain despite medication, certain heart artery shapes, or a high risk of heart problems.
| Clinical Scenario | Benefits of CABG | Key Considerations |
|---|---|---|
| Significant Ischemia | Reduces ischemia, improves myocardial perfusion | Extent of ischemia, patient risk factors |
| Failed/Unsuitable PCI | Alternative revascularization option | Coronary anatomy, patient comorbidities |
| Diabetes with Multi-Vessel Disease | Improves survival, reduces repeat revascularization | Presence of multi-vessel disease, diabetes control |
| Ischemic Cardiomyopathy | Improves cardiac function, patient outcomes | Presence of viable myocardium, cardiac function |
Looking ahead, coronary artery bypass graft (CABG) surgery is set for big changes. New surgical methods and better care before and after surgery will shape the future. These advancements promise to make CABG even better for patients.
CABG will keep playing a key role in treating complex heart disease. Knowing about different CABG procedures, like cabg x3 and cabg x4, will help doctors treat patients with multiple blockages better.
We’re excited for the future of CABG, with hopes for better survival rates and quality of life for patients. Our goal is to provide top-notch healthcare. We’ll use the newest CABG techniques to help patients get the best results.
CABG (Coronary Artery Bypass Graft) surgery is a lifesaving procedure for those with severe heart disease. It’s recommended for patients with big blockages in their heart arteries. This surgery can greatly improve their survival and quality of life.
CABG is mainly for patients with big blockages in the main heart artery or in three of the heart’s arteries. It’s also for those with two-vessel disease and a big blockage in the LAD artery. Or for those with severe chest pain that doesn’t get better with medicine.
On-pump CABG uses a heart-lung machine to keep blood flowing during surgery. Off-pump CABG is done on a beating heart without this machine.
CABG surgery can make patients live longer and feel better. It improves their quality of life by reducing symptoms of heart disease.
Risks include stroke, infection, and graft failure. Other complications can also happen during or after surgery.
Doctors use coronary angiography and other tests to find out if there’s a blockage in the main heart artery. These tests show how severe the blockage is.
The LAD artery is very important because it supplies a lot of the heart. Blockages here can cause serious problems.
Left main equivalent disease means the blockages in the heart arteries are as bad as in the main artery. It often involves more than one artery.
CABG is often suggested for diabetic patients with heart disease in multiple arteries. It can help improve their health and lower the risk of complications.
CABG can help patients with heart muscle damage and viable areas. It improves blood flow to the heart, which can lead to better outcomes.
New CABG techniques include less invasive methods and better grafting. These advancements lead to better results and faster recovery times.
The future of coronary bypass surgery looks bright. It will likely see more advanced techniques and better patient selection. This will help improve outcomes for those with heart disease.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!