Last Updated on November 26, 2025 by Bilal Hasdemir

Chemotherapy is a lifesaving treatment for many cancer patients. But, it comes with its own set of challenges. At Liv Hospital, we know how important it is for patients and their families to know what to expect after treatment. Chemotherapy can affect many parts of the body, impacting organs and systems in lasting ways.
Understanding these risks is key to managing life after cancer. Studies have shown that chemotherapy’s effects can last long. These can include ongoing fatigue, changes in thinking, and even serious damage to the heart and lungs.
We believe in the importance of being aware and prepared for those undergoing cancer treatment. Our aim is to give a clear overview of the risks linked to chemotherapy. We want to help patients understand these risks in simple terms.
Key Takeaways
- Chemotherapy can have lasting impacts on the body.
- Understanding these risks is key to managing life after cancer.
- Patients should be aware of possible long-term complications.
- Liv Hospital is committed to supporting patients through complete care.
- Knowledge is key to navigating life after chemotherapy.
The Lasting Impact of Cancer Treatment
As cancer treatment gets better, it’s more important to understand its lasting effects. Many cancer survivors talk about how treatment changes their lives forever. They need care that goes beyond just the treatment time.
Chemotherapy is a big part of cancer treatment. It targets fast-growing cancer cells but also harms healthy cells. This can cause lasting side effects that don’t go away after treatment ends.
How Chemotherapy Affects Healthy Cells
Chemotherapy drugs kill fast-growing cells, which is good for cancer but bad for healthy cells too. These include cells in the bone marrow, hair follicles, and the digestive tract lining. This can lead to many side effects, both short-term and long-term.
Why Some Side Effects Persist After Treatment
Some chemotherapy side effects can last long after treatment. This can happen for many reasons, like the type and dose of drugs, how long treatment lasts, and the patient’s health. For example, some drugs can damage the heart, lungs, or nerves for a long time.
The reasons for lasting side effects are complex. Things like the patient’s health, genes, and other medical conditions can affect how long and how bad side effects are.
| Factors Influencing Persistent Side Effects | Description |
|---|---|
| Type and Dose of Chemotherapy | The specific chemotherapy drugs and the dosage used can significantly impact the severity of long-term side effects. |
| Duration of Treatment | Longer treatment durations can increase the risk of persistent side effects. |
| Individual Patient Factors | Patient-specific factors, including age, overall health, and genetic predispositions, play a critical role in determining the risk and severity of long-term side effects. |
The Importance of Awareness and Preparation
Knowing about long-term chemotherapy side effects is key to managing them. Patients who understand the risks can prepare better. This means making lifestyle changes, staying healthy, and getting support when needed.
Doctors also have a big role in helping patients. By educating them about chemotherapy’s long-term effects, doctors can support them through treatment and beyond.
Persistent Fatigue: A Common Long-Term Struggle
Persistent fatigue is a big problem for many after chemotherapy. It’s not just feeling tired. It’s a deep exhaustion that makes everyday tasks hard and lowers quality of life.
Why Fatigue Continues After Treatment Ends
Fatigue after cancer treatment comes from many sources. The disease and treatment can harm healthy cells and disrupt body functions. This can lead to long-lasting fatigue. The emotional stress of cancer also plays a role.
Distinguishing Cancer-Related Fatigue from Normal Tiredness
It’s key to tell normal tiredness from cancer-related fatigue. Normal tiredness goes away with rest. But cancer-related fatigue keeps coming back, even after plenty of sleep. People with this fatigue feel very tired and need more rest.
The signs of cancer-related fatigue are:
- Persistent and unrelenting exhaustion
- Not proportional to recent activity or exertion
- Interferes with daily functioning and activities
- Not relieved by rest or sleep
Evidence-Based Management Strategies
Managing cancer-related fatigue needs a full plan. We suggest a mix of exercise, mental health help, and learning how to save energy.
| Management Strategy | Description | Benefits |
|---|---|---|
| Physical Activity | Regular, moderate exercise like walking or yoga | Boosts energy, cuts down fatigue, improves well-being |
| Psychological Interventions | Cognitive-behavioral therapy, stress management, and counseling | Deals with mental health, helps cope better |
| Energy Conservation | Pacing activities, taking regular breaks, prioritizing tasks | Reduces energy use, makes daily tasks easier |
Understanding and tackling persistent fatigue with proven methods can help patients deal with this tough side effect of chemotherapy.
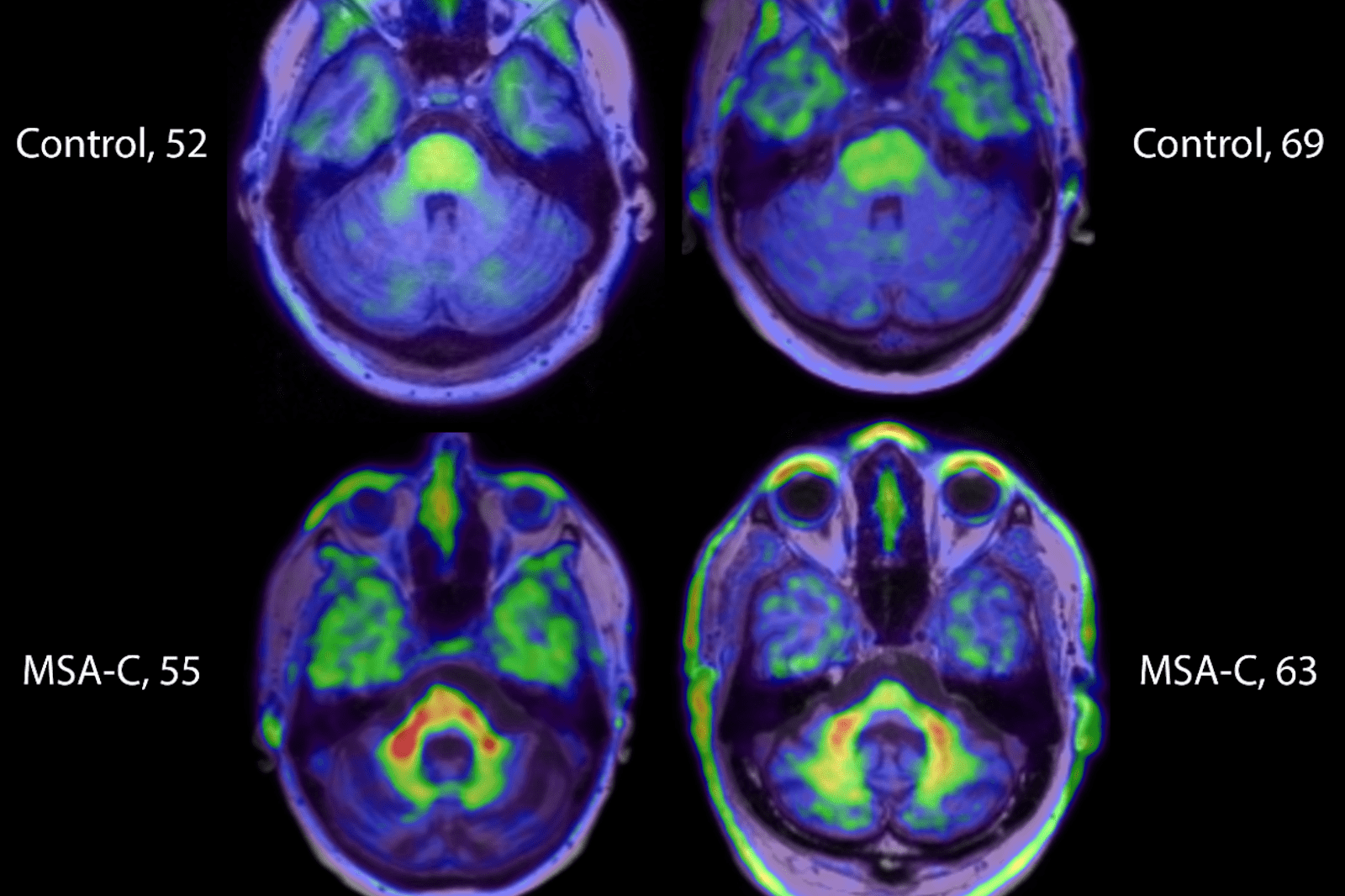
Cognitive Impairment: Understanding “Chemo Brain”
Chemotherapy is a lifesaver but can affect our brains. This is known as ‘chemo brain’. Many people struggle with memory, focus, and other brain tasks after chemo.
Symptoms and Cognitive Domains Affected
‘Chemo brain’ symptoms differ for everyone. But common issues are memory loss, trouble focusing, and poor executive function. Research shows chemo can harm areas like attention, speed, and memory.
Some chemo drugs are worse for the brain than others. Drugs that get into the brain easily are more likely to cause problems.
Neurological Mechanisms Behind Cognitive Changes
The reasons for ‘chemo brain’ are complex. Damage to brain cells, inflammation, and changes in brain structure are possible causes. Knowing these helps us find ways to help.
New studies suggest changes in brain white matter and hormonal shifts can affect thinking.
Rehabilitation Approaches and Compensatory Strategies
Managing ‘chemo brain’ is possible. Cognitive rehab programs, like memory training, can help. These programs aim to improve brain function.
Changing your lifestyle can also help. Regular exercise, staying mentally active, and managing stress are good for your brain. Using tools like calendars and reminders can also be helpful.
| Cognitive Domain | Common Symptoms | Rehabilitation Strategies |
|---|---|---|
| Memory | Forgetting appointments, difficulty recalling familiar words | Memory training, use of memory aids |
| Attention and Concentration | Difficulty focusing, easily distracted | Cognitive training programs, mindfulness exercises |
| Executive Function | Trouble with planning, decision-making | Executive function exercises, strategy training |
Understanding ‘chemo brain’ helps doctors support patients better. This way, patients can manage brain issues and live better lives.
Cardiovascular Complications: Protecting Your Heart
Chemotherapy saves lives but can harm the heart. It’s vital to know the risks and protect heart health during treatment.
Cardiotoxic Chemotherapy Agents
Some chemotherapy drugs are bad for the heart. Anthracyclines, like doxorubicin, are known to cause heart damage. This can lead to heart failure.
“Anthracyclines are effective against cancer but can harm the heart,” a study found. This shows the importance of careful use and monitoring.
Early Detection of Heart Damage
Spotting heart damage early is key. We suggest regular heart function checks for those on cardiotoxic drugs. Echocardiography and cardiac MRI can catch problems early.
- Regular echocardiograms to assess heart function
- Biomarker testing, such as troponin levels, to detect cardiac injury
- Cardiac MRI for detailed imaging of the heart
Cardioprotective Measures During and After Treatment
To lower heart risk, we use cardioprotective agents like dexrazoxane. They help lessen chemotherapy’s heart harm.
Healthy living is also important. Eating well, exercising, and managing stress help the heart. “A healthy lifestyle is essential for cancer survivors,” experts say.
By understanding chemotherapy’s heart risks and taking steps to protect the heart, we can reduce complications. This helps during and after treatment.
Pulmonary Toxicity: Long-Term Respiratory Issues
Chemotherapy can harm the lungs, leading to long-term breathing problems. It’s important for patients and doctors to know about this risk. This way, they can manage it better.
Some chemotherapy drugs are more likely to damage the lungs. Drugs like Bleomycin, Methotrexate, and Cyclophosphamide are among them. They carry a higher risk of lung damage.
Chemotherapy Drugs Associated with Lung Damage
These drugs are used to fight cancer but can harm the lungs. The list includes:
- Bleomycin, commonly used in treating testicular cancer and Hodgkin’s lymphoma
- Methotrexate, used in treating various cancers and autoimmune diseases
- Cyclophosphamide, used in treating several types of cancer and some autoimmune disorders
Progressive and Delayed-Onset Pulmonary Complications
Pulmonary problems can start during or after treatment. They can get worse over time or show up months or years later. It’s important to watch for any breathing issues.
Some patients may get pneumonitis, an inflammation of the lung tissue. This can happen because of chemotherapy. Finding and treating it early is key to avoiding long-term damage.
Monitoring Lung Function After Treatment
It’s vital to check lung function after treatment. This can involve pulmonary function tests (PFTs) and other tests. Regular check-ups with doctors are important to manage these risks.
Understanding the risks and taking action can help patients deal with chemotherapy better. It helps them keep their quality of life.
Peripheral Neuropathy: Lasting Nerve Damage
Chemotherapy can lead to peripheral neuropathy, a condition causing nerve damage. This damage results in pain, numbness, and tingling in certain areas.
Risk Factors for Developing Chronic Neuropathy
Several factors increase the risk of chronic neuropathy in chemotherapy patients. These include:
- The type and dose of chemotherapy administered
- Pre-existing medical conditions, such as diabetes
- Previous exposure to neurotoxic agents
Knowing these risk factors helps in early detection and management of peripheral neuropathy.
Impact on Quality of Life and Daily Functioning
Peripheral neuropathy can greatly affect a patient’s life and daily activities. Symptoms like chronic pain and numbness can make it hard to move and do everyday tasks.
We understand the need to tackle these challenges to better patient outcomes. Ways to manage symptoms and improve quality of life include:
- Physical therapy to improve mobility and strength
- Pain management through medication and alternative therapies
- Lifestyle adjustments to lessen symptoms
Current Treatments and Emerging Therapies
Today’s treatments for peripheral neuropathy aim to manage symptoms and slow disease progression. These include:
- Medications to ease pain and other symptoms
- Therapies to improve nerve function
New therapies hold promise in treating the root causes of peripheral neuropathy. Research into gene therapy and stem cell therapy offers hope for better patient outcomes.
We keep an eye on new developments to offer the best care for those with peripheral neuropathy.
Fertility and Reproductive Health Concerns
Many cancer patients worry about how chemotherapy will affect their ability to have children in the future. We address these concerns with compassion and medical expertise.
Chemotherapy’s Impact on Fertility
Chemotherapy can damage reproductive cells, leading to infertility. The damage’s extent depends on several factors. These include the type and dose of chemotherapy, the patient’s age, and overall health.
Mechanisms of Chemotherapy-Induced Infertility
Chemotherapy drugs can harm ovaries in women and testes in men. This affects their ability to produce eggs and sperm. Women may experience premature ovarian failure, while men may see a decrease in sperm count and quality.
Options for Fertility Preservation
Fortunately, there are several options for fertility preservation before chemotherapy. These include:
- Egg and Embryo Freezing: Women can freeze their eggs or embryos for future use.
- Sperm Banking: Men can bank their sperm for future use.
- Ovarian Tissue Freezing: This is a more experimental technique that involves freezing ovarian tissue.
| Fertility Preservation Method | Description | Applicability |
|---|---|---|
| Egg Freezing | Freezing eggs for future fertilization | Women of reproductive age |
| Sperm Banking | Freezing sperm for future use | Men of reproductive age |
| Ovarian Tissue Freezing | Freezing ovarian tissue for possible future transplantation | Women, including prepubertal girls |
Family Planning After Cancer Treatment
Family planning after chemotherapy can be complex. It’s vital to discuss risks and possibilities with a healthcare provider. Some may conceive naturally after treatment, while others may need assisted reproductive technologies.
We understand the challenges of cancer treatment and beyond. Our goal is to provide care that addresses cancer and overall well-being, including reproductive health.
Bone Health Deterioration and Fracture Risk
Chemotherapy can harm bone health, leading to osteoporosis and fractures. This can greatly affect the life quality of cancer survivors.
Accelerated Bone Loss From Chemotherapy
Chemotherapy can cause bone loss through several ways. It can harm bone cells, change hormones, and reduce mobility. Certain drugs, like glucocorticoids, speed up bone loss. This can lead to osteoporosis, making bones weak and raising fracture risk.
Screening Recommendations for Survivors
Screening for osteoporosis is key for cancer survivors who had chemotherapy. They should get bone density tests, like DXA scans. How often depends on age, sex, and chemotherapy type.
| Risk Factor | Screening Recommendation |
|---|---|
| Age >65 | DXA scan every 2 years |
| History of fractures | DXA scan annually |
| Prolonged glucocorticoid use | DXA scan every 1-2 years |
Nutritional and Pharmacological Interventions
To fight bone loss from chemotherapy, diet and medicine are important. Enough calcium and vitamin D are key for bone health. Survivors should eat well and might need supplements.
Medicines like bisphosphonates and denosumab can help. They slow bone loss, keeping bones strong.
Survivors should talk to their doctors about their risks and how to stay healthy. This ensures they keep their bones strong.
Long Term Side Effects of Chemotherapy Drugs on the Endocrine System
Chemotherapy can have lasting effects on the endocrine system, affecting overall health. The endocrine system is a network of glands that produce hormones. These hormones regulate growth, metabolism, and reproductive processes. When chemotherapy impacts this system, it can lead to a range of long-term side effects.
Thyroid Dysfunction and Management
One common long-term side effect of chemotherapy is thyroid dysfunction. Certain chemotherapy agents can damage the thyroid gland. This can lead to hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid). Symptoms include fatigue, weight changes, and mood swings.
We recommend regular thyroid function tests for patients who have undergone chemotherapy. Management strategies for thyroid dysfunction typically involve medication to normalize thyroid hormone levels. In some cases, lifestyle adjustments, such as dietary changes, can also help manage symptoms.
| Chemotherapy Agent | Risk of Thyroid Dysfunction | Management Strategy |
|---|---|---|
| Tyrosine Kinase Inhibitors | High | Regular thyroid function tests, medication |
| Alkylating Agents | Moderate | Thyroid function monitoring, lifestyle adjustments |
| Anthracyclines | Low | Observation, thyroid function tests as needed |
Premature Menopause and Hormonal Changes
Chemotherapy can induce premature menopause in women, leading to hormonal changes. This condition, also known as chemotherapy-induced ovarian failure, can result in symptoms such as hot flashes, vaginal dryness, and mood changes.
We advise women undergoing chemotherapy to discuss fertility preservation options with their healthcare provider before starting treatment. For those who experience premature menopause, hormone replacement therapy (HRT) may be recommended to alleviate symptoms.
Metabolic Syndrome and Insulin Resistance
Metabolic syndrome, a cluster of conditions including high blood pressure, high blood sugar, and abnormal lipid profiles, can be exacerbated by chemotherapy. Insulin resistance, a precursor to type 2 diabetes, is also a concern.
Lifestyle modifications, such as a healthy diet and regular exercise, are key in managing metabolic syndrome and insulin resistance. We also recommend regular monitoring of metabolic parameters and, if necessary, medication to control blood pressure, blood sugar, and lipid levels.
By understanding the long-term effects of chemotherapy on the endocrine system, patients and healthcare providers can work together. This helps improve quality of life for cancer survivors.
Secondary Cancers: The Hidden Risk
Chemotherapy is a lifesaver but comes with a hidden risk. This risk shows up long after treatment ends. It’s about secondary cancers, a known side effect of some chemotherapy. We need to know the risks and how to watch for them.
Chemotherapy Agents Associated with Secondary Malignancies
Some chemotherapy drugs raise the risk of secondary cancers. Alkylating agents, for example, can lead to leukemia. Topoisomerase inhibitors also increase the risk of secondary cancers.
Examples of chemotherapy agents associated with secondary malignancies include:
- Alkylating agents (e.g., cyclophosphamide, melphalan)
- Topoisomerase inhibitors (e.g., etoposide, doxorubicin)
Latency Periods and Risk Duration
The time it takes for secondary cancers to appear after chemotherapy varies. For some, it’s just a few years. For others, it can take decades. Knowing how long the risk lasts is key for ongoing care.
The risk duration depends on the chemotherapy type, dose, and treatment length. For example, the risk of t-MN after alkylating agents peaks at 4-6 years post-treatment.
Surveillance Guidelines for Cancer Survivors
Cancer survivors need ongoing care due to secondary cancer risks. Guidelines suggest regular checks for these cancers. The checks depend on the chemotherapy used and the survivor’s risk factors.
Surveillance may include:
- Regular physical examinations
- Laboratory tests (e.g., complete blood counts)
- Imaging studies as recommended by guidelines or based on clinical suspicion
By knowing the risks and following guidelines, we can catch secondary cancers early. This helps manage them better in cancer survivors.
Compounded Effects of Chemotherapy and Radiation
Chemotherapy and radiation therapy together can harm the body more. This is why it’s important for patients and doctors to know the risks and long-term side effects.
Synergistic Toxicity in Combined Modality Treatment
Synergistic toxicity happens when chemotherapy and radiation work together to cause more damage. This can hurt healthy tissues and organs more, leading to worse side effects. It’s key to understand this to make treatment plans that are safe yet effective.
Studies show that using both treatments can harm organs like the heart, lungs, and stomach more. For example, some chemotherapy can make heart problems worse when combined with radiation.
Organ-Specific Combined Effects
The harm from chemotherapy and radiation can differ based on the organ and treatment. For instance:
- Cardiovascular System: Mixing anthracyclines with chest radiation can greatly increase heart damage, leading to heart failure.
- Pulmonary System: Some chemotherapy and thoracic radiation can cause lung problems, like pneumonitis and fibrosis.
- Gastrointestinal System: Using chemotherapy and abdominal radiation together can harm the stomach, causing nausea, vomiting, and diarrhea.
Risk Reduction Strategies for Patients Receiving Both Treatments
To lessen the harm from chemotherapy and radiation, several strategies can be used. These include:
- Personalized Treatment Planning: Making treatment plans that fit each patient’s needs can reduce unnecessary harm.
- Advanced Radiation Techniques: Using modern radiation methods, like IMRT, can lower doses to healthy tissues.
- Cardioprotective and Pulmonoprotective Measures: Using protective agents during chemotherapy can lessen organ damage.
By knowing the harm from chemotherapy and radiation and using these strategies, doctors can help patients better. This improves the chances of a good outcome.
Conclusion: Navigating Life After Chemotherapy
The journey through cancer treatment is complex. Understanding the long term side effects of chemotherapy drugs is key for both patients and healthcare providers. Managing these effects is vital for a good quality of life after chemotherapy.
We’ve looked at many long-term challenges, like persistent fatigue and cognitive issues. There are also cardiovascular problems and secondary cancers to consider. It’s important for cancer survivors to get ongoing support and care to handle these side effects.
Being aware of risks and taking action can help patients navigate life after chemotherapy. This means adopting healthy habits, going to regular check-ups, and seeking help when needed. A team effort between patients, healthcare providers, and caregivers is essential to meet each survivor’s unique needs.
With the right support, people can do well after cancer treatment. They can manage their side effects and improve their overall health and well-being.
FAQ
What are the long-term side effects of chemotherapy?
Chemotherapy can lead to long-term side effects. These include persistent fatigue and cognitive impairment. It can also cause cardiovascular complications and affect the lungs.