Last Updated on November 26, 2025 by Bilal Hasdemir

For many cancer survivors, the end of chemotherapy is just the start of new challenges. Lasting effects can linger and reshape life, affecting both physical and mental health. At Liv Hospital, we help patients through every stage, guiding them on what to expect next.
Chemotherapy is a daunting experience, and the journey after is just as important. We use stories like Tylher Coleman’s fight against triple-negative breast cancer to help understand these lasting effects. It’s essential to be aware of the possible long-term side effects that can last for months or even years after treatment ends.
Key Takeaways
- Chemotherapy can have lasting effects on both physical and mental health.
- Understanding these effects is key to managing them well.
- Real-life experiences offer valuable insights into the challenges faced by cancer survivors.
- Liv Hospital offers compassionate expert care to guide patients through every stage.
- Awareness of possible long-term side effects can help patients prepare and cope.
Understanding the Persistence of Chemotherapy Effects
Chemotherapy can leave a lasting mark on the body, causing side effects that last long after treatment. This is a big worry for cancer survivors. It’s important to know why these effects can stick around.
How Chemotherapy Damages Healthy Cells
Chemotherapy aims to kill fast-growing cancer cells. But it can also harm healthy cells that grow quickly. This includes cells in the bone marrow, digestive tract, and hair follicles. Damage to these cells can cause short-term side effects like fatigue, nausea, and hair loss.
But some chemotherapy agents can also harm healthy cells for a long time. This can lead to side effects that don’t go away. It’s key to understand how different chemotherapy agents affect healthy cells to lessen their long-term effects.
Why Some Side Effects Last for Years
Several factors can make chemotherapy side effects last a long time. These include the type and dose of chemotherapy, how long treatment lasts, and the patient’s individual characteristics. Some side effects, like neuropathy and cognitive problems, can be very hard to deal with and may last for years.
| Chemotherapy Agent | Potential Long-Term Side Effects |
|---|---|
| Anthracyclines | Cardiotoxicity, heart failure |
| Platinum-based agents | Neuropathy, ototoxicity, kidney damage |
| Taxanes | Neuropathy, muscle pain, nail changes |
Chemotherapy can cause lasting side effects like persistent fatigue, neuropathy, and cognitive problems. By understanding why these effects happen, we can work to manage and reduce them. This can greatly improve the lives of cancer survivors.
The Reality of “Chemo Ruined My Life”: Patient Perspectives
Many cancer survivors say “chemo ruined my life” after dealing with long-term effects. They face severe side effects from treatment. Tylher Coleman, a survivor, shares her struggles after treatment.
Tylher’s story shows chemotherapy’s lasting impact. The side effects can greatly lower a survivor’s quality of life. We’ll look at how these effects affect survivors and their lives after treatment.
Impact on Quality of Life
Chemotherapy’s long-term effects can change a survivor’s life in many ways. Chronic fatigue, neuropathy, and cognitive dysfunction are common. These issues affect not just the body but also the mind and emotions, making it hard to get back to normal.
One survivor said, “
The hardest part is not knowing what’s going to happen next. Will I be able to work? Will I be in pain? It’s like living in limbo.
” This shows the uncertainty and fear survivors face with long-term effects.
Balancing Cancer Survival with Long-Term Effects
Survivors often struggle to balance celebrating their survival with missing their old life. The side effects of chemotherapy make simple tasks hard. They affect work, hobbies, and social life. It’s a tough balance between being thankful and grieving the changes.
We understand that every cancer journey is different. By sharing stories like Tylher Coleman’s, we hope to help others understand the challenges. We also highlight the need for strong support systems.
Persistent Fatigue and Energy Depletion
Chemotherapy can leave a lasting mark, with persistent fatigue hitting many survivors hard. This feeling of constant tiredness makes everyday tasks tough and lowers life quality.
About 50% of survivors face chronic fatigue, a fact that highlights how common it is. The reasons behind it are complex, involving body, mind, and lifestyle factors.
Causes of Chronic Fatigue in Cancer Survivors
The reasons for chronic fatigue in cancer survivors are not fully known. But, several factors are thought to play a role. These include how chemotherapy affects the body, hormonal changes, and the emotional toll of cancer and treatment.
“Fatigue is one of the most distressing symptoms reported by cancer patients, and it can persist long after treatment has ended.”
Energy Conservation Techniques
Dealing with chronic fatigue needs a mix of strategies, including energy conservation techniques. By focusing on what’s important, taking breaks, and resting regularly, survivors can manage their energy better.
| Technique | Description | Benefit |
|---|---|---|
| Prioritization | Focus on essential activities | Conserves energy for important tasks |
| Pacing | Balance activity with rest | Reduces fatigue and prevents exhaustion |
| Relaxation Techniques | Practice deep breathing, meditation, or yoga | Reduces stress and promotes restful sleep |
Living a healthy lifestyle also helps fight chronic fatigue. Eating well, exercising, and getting enough sleep are key. By using these methods, survivors can enhance their life quality and handle fatigue better.
Neuropathy: Long-Term Nerve Damage
Neuropathy is a lasting side effect of chemotherapy that causes chronic nerve pain. It affects many patients. We will look at why it happens and what can be done to manage it.
Why 58% of Patients Develop Persistent Neuropathies
Chemotherapy can damage nerve fibers, leading to pain and numbness. This damage comes from certain chemotherapy drugs. The risk depends on the type and dose of chemotherapy and the patient’s health.
Management Options for Chronic Nerve Pain
Dealing with neuropathy needs a variety of approaches. Some people get better over time, but others need ongoing care. Here are some ways to manage it:
- Medications to help with pain and symptoms
- Alternative therapies like acupuncture and physical therapy
- Changes in lifestyle, such as diet and stress management
“I’ve been dealing with neuropathy for years, and it’s been a challenge. But with the right management plan and support, I’ve learned to live with it.”
| Treatment Option | Effectiveness | Side Effects |
|---|---|---|
| Medications | High | Drowsiness, dizziness |
| Acupuncture | Moderate | Bruising, soreness |
| Physical Therapy | Moderate | Muscle soreness |
Neuropathy is a tough side effect of chemotherapy, but it can be managed. Understanding the causes and trying different treatments can help cancer survivors live better lives.
Cognitive Dysfunction: “Chemo Brain”
Chemotherapy can cause lasting effects on memory and concentration. This is known as “chemo brain” and affects many cancer survivors. We will look at how it impacts survivors and ways to manage it.
Memory and Concentration Problems in 35% of Survivors
About 35% of survivors face memory and concentration issues after chemotherapy. These problems can make it hard to learn new things, remember appointments, or stay focused.
Cognitive Rehabilitation Strategies
Fortunately, there are ways to manage “chemo brain.” These include cognitive training, lifestyle changes, and stress management.
- Cognitive training programs to improve memory and concentration.
- Lifestyle modifications such as regular exercise and a balanced diet.
- Stress management techniques like meditation and yoga.
Managing cognitive dysfunction requires a mix of these strategies. Here’s a table with some key strategies:
| Strategy | Description | Benefits |
|---|---|---|
| Cognitive Training | Programs designed to improve memory and concentration | Enhances cognitive function, improves daily task management |
| Regular Exercise | Physical activity tailored to the individual’s capacity | Improves overall health, boosts cognitive function |
| Balanced Diet | Nutrition plans focusing on brain health | Supports cognitive recovery, overall well-being |
| Stress Management | Techniques such as meditation and yoga | Reduces stress, improves cognitive function and overall quality of life |
Understanding and tackling cognitive dysfunction helps cancer survivors deal with “chemo brain.” It improves their quality of life.
Cardiovascular Complications: Heart Damage
Chemotherapy can harm the heart, leading to serious problems. As more people survive cancer, it’s key to understand and manage these long-term effects.
Types of Chemotherapy-Related Heart Problems
Some chemotherapy drugs can damage the heart. The main heart problems caused by chemotherapy are:
- Cardiomyopathy: a condition where the heart muscle weakens, making it hard to pump blood.
- Heart Failure: when the heart can’t pump enough blood for the body’s needs.
- Arrhythmias: irregular heartbeats caused by damage to the heart’s electrical system.
Research shows that drugs like anthracyclines can raise heart problem risks. For example, Corventum has been given IND clearance for CVT-130. This is a new treatment to prevent heart damage from anthracyclines (Corventum Press Release).
Cardiac Monitoring and Prevention
Regular heart checks are vital for catching and managing heart issues early. This includes:
| Monitoring Method | Description | Frequency |
|---|---|---|
| Echocardiogram | An ultrasound test that evaluates heart function. | Before, during, and after chemotherapy. |
| Electrocardiogram (ECG) | A test that measures the heart’s electrical activity. | As recommended by the healthcare provider. |
| Biomarker Tests | Tests that measure specific proteins in the blood that indicate heart damage. | During and after chemotherapy. |
To prevent heart problems, making healthy lifestyle choices is important. This includes eating well and exercising. Also, taking medicine to control risk factors like high blood pressure and cholesterol is helpful.
Long Term Chemo Side Effects on Vital Organs
Chemotherapy saves lives but can harm vital organs. This can affect the quality of life for cancer survivors. It’s important to know how it impacts organs like the liver, kidneys, and lungs.
Liver Toxicity and Function Changes
The liver detoxifies and metabolizes substances. Some chemo agents can harm the liver, changing its function. Monitoring liver health through tests and scans is key to catching damage early.
Some chemo drugs can cause hepatotoxicity, raising liver enzymes and, in bad cases, liver failure. Knowing the risks and taking steps to prevent them can help.
Kidney Damage and Renal Complications
Kidney harm is another possible long-term chemo side effect. Some chemo agents can damage kidneys, leading to chronic disease or worsening existing issues. Renal function monitoring is vital for chemo patients.
Drinking enough water and avoiding harmful meds can lower kidney damage risk. Regular kidney function tests are essential for early detection.
Pulmonary Fibrosis and Breathing Difficulties
Pulmonary fibrosis, lung scarring, can result from some chemo agents. This can cause breathing problems and lower lung function. Early detection through tests and scans is key to managing this.
If you have symptoms like shortness of breath or cough, see a doctor. Treatment may include meds to slow disease and improve life quality.
| Vital Organ | Potential Chemotherapy-Related Complications | Monitoring and Management Strategies |
|---|---|---|
| Liver | Liver toxicity, hepatotoxicity | Regular blood tests, imaging studies, preventive measures |
| Kidneys | Kidney damage, nephrotoxicity, chronic kidney disease | Renal function monitoring, hydration, avoiding nephrotoxic medications |
| Lungs | Pulmonary fibrosis, breathing difficulties | Pulmonary function tests, imaging studies, early detection and management |
It’s vital to understand chemotherapy’s long-term effects on vital organs. By closely monitoring these effects and using the right management strategies, we can enhance the lives of cancer survivors.
Bone and Musculoskeletal System Effects
Long-term chemotherapy side effects can deeply affect the musculoskeletal system. While it fights cancer, it can also harm bone density and joint health. We will look into these effects and how to manage them.
Osteoporosis and Increased Fracture Risk
Chemotherapy can raise the risk of osteoporosis, where bones weaken. Some chemotherapy agents can lower bone density, making fractures more likely. Osteoporosis management is key for cancer survivors to avoid fractures and keep moving.
Research shows chemotherapy can decrease bone mineral density, mainly in postmenopausal women. We suggest cancer survivors talk to their healthcare provider about their osteoporosis risk. Ways to manage osteoporosis include:
- Calcium and vitamin D supplements
- Weight-bearing exercises
- Medications to prevent bone loss
| Osteoporosis Management Strategies | Benefits |
|---|---|
| Calcium and Vitamin D Supplements | Enhance bone density |
| Weight-bearing Exercises | Improve bone strength |
| Medications | Prevent bone loss |
Joint Pain and Mobility Issues
Joint pain and mobility issues are common in cancer survivors who have had chemotherapy. The exact reasons are not fully known. But, it’s thought that some chemotherapy agents can damage nerves and cause inflammation, leading to pain and stiffness.
We recommend the following for managing joint pain:
- Physical therapy to improve joint mobility
- Pain management medications
- Alternative therapies such as acupuncture
By understanding how chemotherapy affects bone health and the musculoskeletal system, cancer survivors can take steps to manage these issues. We encourage survivors to work with their healthcare providers to keep their bones and joints healthy.
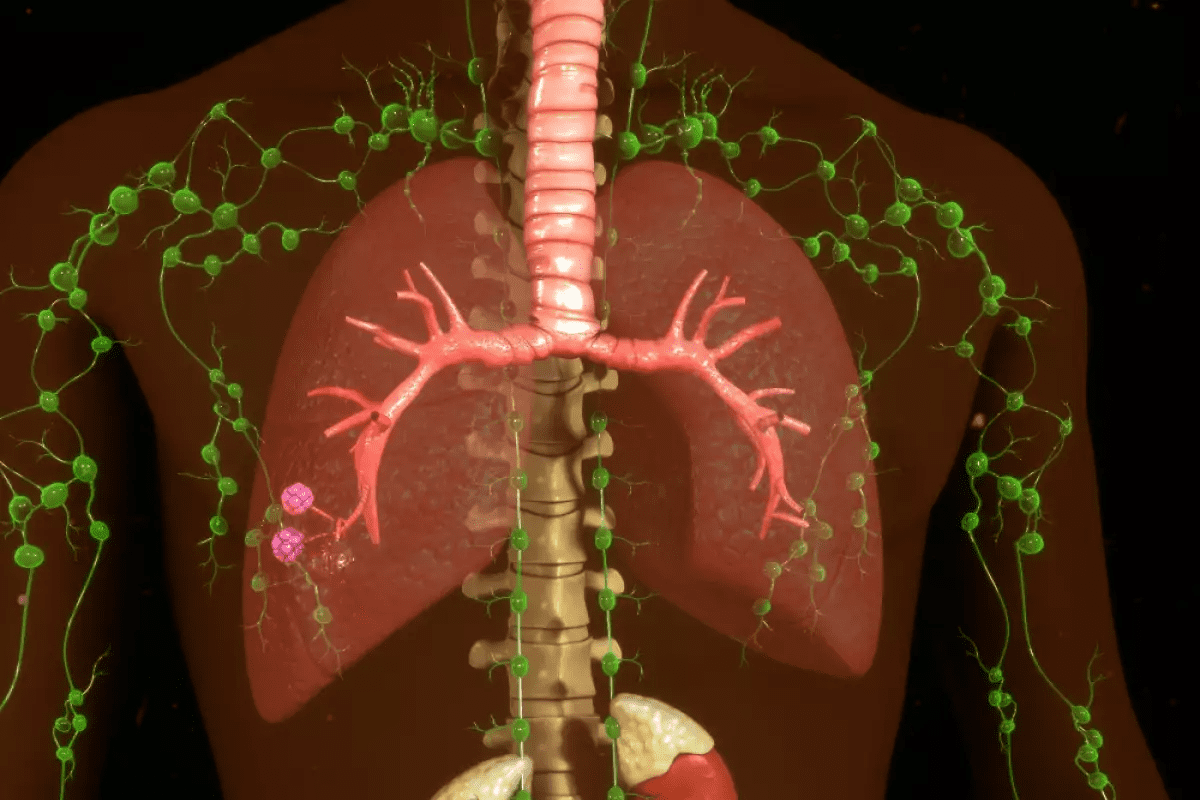
Immune System Suppression and Infection Risk
Chemotherapy can weaken the immune system, making it harder to fight off infections. The immune system protects us from harmful germs. When it’s weakened, even small infections can become serious.
Research shows that some chemotherapy drugs can lower immune function. This affects the production of white blood cells, which are key in fighting off infections. This weakening can last for months or even years after treatment ends.
Long-Term Immune Function Changes
The effects of chemotherapy on the immune system vary. They depend on the type and dose of chemotherapy and the patient’s health. Some people’s immune systems may recover slowly, while others may stay weakened.
To learn more about chemotherapy’s effects on the body, visit Liv Hospital. They provide detailed information on chemotherapy’s impacts.
Strategies to Strengthen Immunity
When the immune system is weak, it’s important to prevent infections. Simple actions like washing hands often, staying away from sick people, and getting vaccinated can help. These steps can reduce the risk of getting sick.
Living a healthy lifestyle also supports the immune system. Eating well, exercising regularly, and getting enough sleep are important. Some people might also need supplements or medications to boost their immune system.
Key strategies include:
- Practicing good hygiene
- Staying up-to-date on recommended vaccinations
- Eating a nutritious diet
- Exercising regularly
- Getting enough rest
By understanding the risks and taking proactive steps, cancer survivors can lower their infection risk. This helps promote overall health.
Secondary Cancers and Malignancies
Chemotherapy saves lives but can also raise the risk of getting secondary cancers in some cases. It’s important to know the risks and how to screen for them.
Risk Factors for Treatment-Induced Cancers
Some chemotherapy drugs can lead to secondary cancers. The risk depends on the drug type, dose, the patient’s age, and their genes.
Key Risk Factors:
- Type and dose of chemotherapy agents
- Patient’s age during treatment
- Genetic predispositions
- Combination with radiation therapy
Research shows that drugs like alkylating agents and topoisomerase inhibitors are more likely to cause secondary cancers.
| Chemotherapy Agent | Associated Secondary Cancer Risk |
|---|---|
| Alkylating agents | High risk of myelodysplastic syndromes and acute myeloid leukemia |
| Topoisomerase inhibitors | Increased risk of secondary leukemia |
Screening Recommendations for Survivors
Regular screening is key to catch secondary cancers early. The right screening depends on the primary cancer, chemotherapy, and individual risks.
General Screening Guidelines:
- Annual follow-up visits with a healthcare provider
- Regular blood tests to monitor blood cell counts
- Imaging studies as recommended by healthcare providers
Survivors should talk to their healthcare team about their specific risks and screening plans.
By knowing the risks and following screening advice, cancer survivors can lower their chance of getting secondary cancers. This helps keep them healthy overall.
Combined Effects of Chemotherapy and Radiation
Chemotherapy and radiation together can cause many long-term side effects. They work better together to fight cancer. But, this also means more risks for long-term problems.
Compounded Risks from Multiple Treatment Modalities
Research shows that using both treatments can raise compounded risks in the body. For example, heart disease risk goes up for those who get both treatments. We must plan follow-up care carefully for cancer survivors.
The interaction between chemotherapy and radiation can make some organs more toxic. For example, heart damage risk goes up with anthracycline chemotherapy and chest radiation. Knowing these interactions helps reduce long-term side effects.
Organ-Specific Concerns with Combined Therapy
Organs react differently to chemotherapy and radiation. The liver and kidneys are very sensitive to some drugs. Adding radiation makes damage risk higher. We must watch organ function closely in patients who get both treatments.
- Liver damage from methotrexate can get worse with radiation.
- Kidney damage from some drugs gets worse with radiation.
- Pulmonary fibrosis risk goes up with certain drugs and chest radiation.
Managing Complex Side Effect Profiles
Handling side effects from both treatments needs a multidisciplinary approach. Regular check-ups with doctors are key. We also need to teach patients about possible long-term effects and encourage them to report new symptoms.
Understanding the risks and concerns of combined therapy helps us target solutions. This approach can greatly improve life quality for cancer survivors.
Living Well After Chemotherapy: Moving Forward
Cancer survivors face many challenges after chemotherapy. But, with the right strategies and support, they can manage these effects and thrive. Survivorship is not just about surviving cancer; it’s about living well after treatment.
Tylher Coleman’s story shows the human spirit’s strength. After chemotherapy, Tylher helped others who faced similar challenges. Her story shows how important community and support are in the survivorship journey.
To live well after chemotherapy, survivors can take proactive steps. They can maintain a healthy lifestyle, stay connected with healthcare providers, and seek support from loved ones and support groups. By focusing on survivorship and managing long-term effects, survivors can move forward with confidence.
FAQ
What are the most common long-term side effects of chemotherapy?
Long-term side effects of chemotherapy include fatigue, neuropathy, and cognitive issues. There are also cardiovascular problems and damage to organs like the liver, kidneys, and lungs.
How does chemotherapy damage healthy cells, and why do some side effects last for years?
Chemotherapy harms healthy cells by targeting fast-growing ones. This can cause long-lasting side effects. Some effects last years because of the lasting impact on cells and the body’s recovery.
Can long-term chemo side effects be managed or mitigated?
Yes, many long-term side effects can be managed. Techniques include conserving energy, cognitive rehab, cardiac monitoring, and lifestyle changes.
What is the impact of chemotherapy on the immune system, and how can it be strengthened?
Chemotherapy weakens the immune system, making infections more likely. To boost immunity, live healthily, get vaccinated, and practice good hygiene.
Are there any risks of secondary cancers after chemotherapy, and how can they be mitigated?
Yes, chemotherapy increases the risk of secondary cancers. Factors include the type and dose of chemotherapy and patient characteristics. Screening and regular follow-up care can reduce this risk.
How do combined treatment modalities, such as chemotherapy and radiation, impact long-term health?
Combined treatments can raise the risk of long-term side effects, including organ damage. Managing these side effects requires careful monitoring and follow-up care.
What can be done to promote overall health and well-being after chemotherapy?
To promote health after chemotherapy, maintain a healthy lifestyle. Manage long-term side effects and seek support from healthcare and loved ones.
How common is persistent fatigue after chemotherapy, and how can it be managed?
Up to 50% of survivors experience persistent fatigue after chemotherapy. Manage it by pacing activities and taking regular breaks.
What are the risks of cardiovascular complications after chemotherapy, and how can they be mitigated?
Cardiovascular complications are a big concern after chemotherapy, more so for certain types. Monitor the heart and prevent complications by living healthily and managing risk factors.
Can chemotherapy cause long-term damage to vital organs, and how can it be monitored?
Yes, chemotherapy can damage vital organs like the liver, kidneys, and lungs. Regular monitoring and follow-up care can help manage these complications.