Last Updated on November 25, 2025 by Ugurkan Demir

At Liv Hospital, we know how vital it is to understand and manage life-threatening arrhythmias. These issues can cause sudden cardiac death if not treated quickly. Recent data shows a big rise in deaths from arrhythmias, making it key to be aware and seek medical help fast.
We will talk about two serious conditions: ventricular fibrillation and sustained ventricular tachycardia. These cardiac arrhythmia types are very dangerous and need quick action. Knowing the facts and risks helps patients manage their condition and lower the chance of problems.
Key Takeaways
- Ventricular fibrillation and sustained ventricular tachycardia are two critical heart rhythm disorders.
- These conditions can lead to sudden cardiac death if not treated promptly.
- Recent statistics show a significant increase in arrhythmia-related mortality rates.
- Awareness and prompt medical intervention are key in managing life-threatening arrhythmias.
- Understanding the key facts and risks associated with these conditions can help patients manage their condition effectively.
Understanding Cardiac Arrhythmias: The Basics
It’s important to understand cardiac arrhythmias to know how they affect heart health. These conditions happen when the heart’s electrical system goes wrong. This leads to irregular heartbeats, which can be mild or serious.
What Is a Cardiac Arrhythmia?
A cardiac arrhythmia is a problem with the heart’s electrical system. This system makes sure the heart beats right, pumping blood well. When it fails, the heart’s rhythm gets mixed up, causing arrhythmias.
Arrhythmias can be simple or complex. They can range from skipped beats to serious issues like atrial fibrillation or ventricular tachycardia. Knowing about these conditions helps in treating them.
How Normal Heart Rhythm Works
A normal heart rhythm is key for the heart’s work. The heartbeat is controlled by electrical signals from the sinoatrial node in the right atrium. These signals make the heart contract and pump blood.
The heart rate should be between 60 to 100 beats per minute. If it’s off, it might mean an arrhythmia. Stress, caffeine, and some medicines can change heart rate, but constant changes need a doctor’s check.
| Heart Rate (bpm) | Condition | Description |
| 60-100 | Normal | Normal heart rhythm |
| <60 | Bradycardia | Abnormally slow heart rate |
| >100 | Tachycardia | Abnormally fast heart rate |
When Heart Rhythms Become Dangerous
Some arrhythmias are harmless, but others are very dangerous. Conditions like ventricular fibrillation or sustained ventricular tachycardia need quick medical help. If not treated fast, they can cause cardiac arrest.
It’s key to know the signs of dangerous arrhythmias. Symptoms include palpitations, dizziness, chest pain, or shortness of breath. If you see these signs, get emergency medical help right away.
2 Life Threatening Arrhythmias: Ventricular Fibrillation and Ventricular Tachycardia
Ventricular fibrillation and sustained ventricular tachycardia are very dangerous. They can cause sudden cardiac arrest. These conditions stop the heart from working right, leading to a big drop in blood flow.
Ventricular Fibrillation: The Silent Killer
Ventricular fibrillation makes the heart’s ventricles quiver fast and erratically. This stops the heart from pumping blood well. It’s called a “silent killer” because it can happen without warning, leading to sudden cardiac arrest.
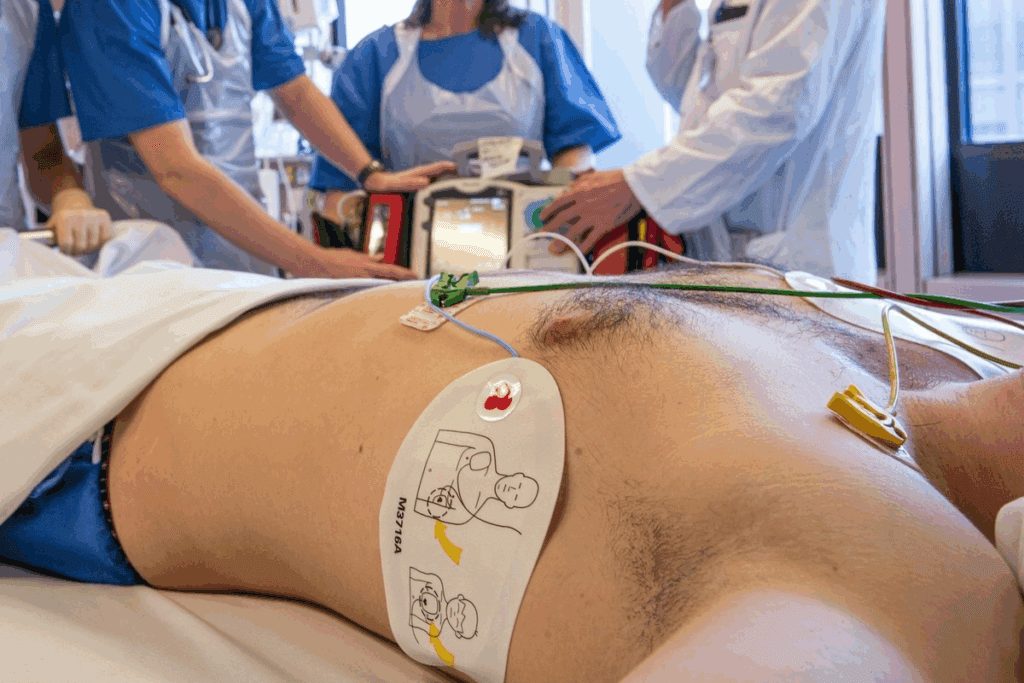
This is a medical emergency that needs quick action. Treatment usually involves defibrillation to get the heart beating normally again.
Sustained Ventricular Tachycardia: Racing to Danger
Sustained ventricular tachycardia is a fast heart rate from the ventricles, over 100 beats per minute. It’s dangerous because it makes it hard for the heart to fill with blood. This can lead to cardiac arrest.
Symptoms include palpitations, dizziness, and shortness of breath. If not treated, it can turn into ventricular fibrillation, raising the risk of sudden death.
Why These Two Are Particualrly Deadly
Both ventricular fibrillation and sustained ventricular tachycardia are deadly because they can cause sudden cardiac arrest. The table below shows the main differences and risks of these conditions.
| Condition | Characteristics | Risks |
| Ventricular Fibrillation | Erratic quivering of ventricles, no effective blood pumping | Sudden cardiac arrest, death if not treated promptly |
| Sustained Ventricular Tachycardia | Fast heart rate from ventricles, reduced cardiac output | Cardiac arrest, degeneration into ventricular fibrillation |
It’s important to know about these dangerous heart rhythms. Quick action can save lives. Recognizing and treating ventricular fibrillation and sustained ventricular tachycardia early can greatly improve survival chances.
Other Serious Arrhythmias That Can Become Life-Threatening
Ventricular fibrillation and ventricular tachycardia are well-known dangers. But other serious arrhythmias also carry big risks. These conditions can cause severe problems and even lead to more dangerous heart rhythms.
Atrial Flutter: When It Becomes Dangerous
Atrial flutter is a fast but regular heart rhythm. It’s usually okay for a while but can be risky for people with heart problems. Atrial flutter can cause stroke and heart failure if not treated. This risk is higher for those with heart disease.
Junctional Rhythms and Associated Risks
Junctional rhythms start from the AV junction in the heart. They can show problems like digitalis toxicity or heart attack. Junctional tachycardia, a faster version, can cause unstable blood flow, mainly in older or sick people.
Progression from Common to Critical Arrhythmias
Common arrhythmias like atrial flutter can turn into worse forms. For example, atrial flutter can turn into atrial fibrillation, raising the risk of blood clots. Knowing why this happens is key to preventing it. Managing heart disease can lower these risks.
Doctors need to watch patients with arrhythmias closely. They should also teach them about signs of worsening conditions. Early action can greatly improve results.
Alarming Statistics: The Rising Threat of Fatal Arrhythmias
Recent statistics show a shocking trend: a big jump in deaths from arrhythmias in the United States. This alarming rise is a big worry for the US healthcare system. It needs a closer look at the data and the reasons behind it.
450% Increase in Arrhythmia-Related Mortality in the US
The data shows a 450% increase in deaths from arrhythmias in the US. This is a huge number that shows how serious the problem is. It’s not just a small issue; it’s a big public health crisis that needs quick action.
Arrhythmia-related deaths used to be rare. But over the last few decades, they have gone up a lot. The causes are complex, involving many factors like age, lifestyle, and healthcare.
Demographics Most Affected
Some groups are hit harder by the rise in arrhythmia-related deaths. Older adults and people with heart problems are at the highest risk. Also, socioeconomic factors play a part, with poorer people facing more risks because they can’t get to healthcare.
People with diabetes and chronic kidney disease are also at high risk. These conditions make arrhythmias more likely and harder to manage, leading to more deaths.
Factors Behind the Dramatic Increase
Many things contribute to the big jump in arrhythmia-related deaths. Lifestyle factors like being overweight, smoking, and not moving enough are big problems. Also, more people have heart conditions and the US population is getting older.
Another big factor is how modern healthcare works. New medical tech and treatments help more people live longer. But they also bring new risks, like side effects from medicines and problems from procedures, which can lead to arrhythmia deaths.
Recognizing the Warning Signs
It’s important to know the warning signs of life-threatening arrhythmias. This knowledge helps in getting medical help on time. We will talk about the key symptoms and when to seek help.
Symptoms of Ventricular Fibrillation
Ventricular fibrillation has a chaotic heart rhythm that can cause sudden cardiac arrest. Look out for these symptoms:
- Severe dizziness or fainting
- Rapid heartbeat or palpitations
- Chest pain or discomfort
- Shortness of breath
If you or someone else shows these signs, act fast.
Symptoms of Sustained Ventricular Tachycardia
Sustained ventricular tachycardia is serious and can be life-threatening. Its symptoms include:
- A rapid heartbeat that doesn’t slow down
- Dizziness or lightheadedness
- Chest pain or tightness
- Fainting or near-fainting
When to Seek Emergency Medical Attention
If you have any of these symptoms, get emergency help right away:
- Severe chest pain or pressure
- Severe shortness of breath
- Fainting or loss of consciousness
- Rapid or irregular heartbeat
Quick action can save lives in these cases.
Silent Arrhythmias: The Hidden Danger
Some arrhythmias don’t show symptoms, known as asymptomatic. Regular check-ups and screenings are key. They help find these hidden dangers, if you have heart conditions or risk factors.
Knowing the warning signs and taking action early can greatly lower the risk of fatal arrhythmias.
Risk Factors: Are You in Danger?
Some health conditions, lifestyle choices, and genetic factors can raise the risk of serious arrhythmias. Knowing these risk factors is key for early detection and prevention.
Underlying Heart Conditions
Heart conditions can increase the risk of serious arrhythmias. Issues like coronary artery disease, heart failure, and cardiomyopathy can harm the heart’s electrical system.
Coronary Artery Disease is a major cause of arrhythmias. It happens when blood flow to the heart muscle is reduced, damaging the heart’s electrical pathways.
Lifestyle Factors
Lifestyle choices greatly impact heart health. Smoking, drinking too much alcohol, and being inactive can raise the risk of arrhythmias.
| Lifestyle Factor | Risk Level | Prevention Strategy |
| Smoking | High | Quit smoking programs |
| Excessive Alcohol Consumption | Moderate to High | Limit alcohol intake |
| Physical Inactivity | Moderate | Regular exercise routine |
Genetic Predispositions
Genetics can also affect the risk of serious arrhythmias. Conditions like Long QT Syndrome and Brugada Syndrome are inherited and affect the heart’s electrical system.
Family history is a big clue for genetic risks. If your family has a history of sudden cardiac deaths or arrhythmias, talk to your doctor.
Medication-Related Risks
Some medications can increase the risk of arrhythmias. This includes certain anti-arrhythmic drugs, antibiotics, and antihistamines that can prolong the QT interval.
Always check with your doctor about your medications. This helps understand any risks and keep an eye on your heart health.
High-Risk Populations: Diabetes and Kidney Disease Connection
Diabetes, kidney disease, and arrhythmias are linked in a complex way. These conditions often raise the risk of heart rhythm problems. Diabetes and kidney disease are big risks for arrhythmias, like ventricular fibrillation and sustained ventricular tachycardia.
Why Diabetic Patients Face Greater Arrhythmia Risk
Diabetic patients face a higher risk of arrhythmias for several reasons. Hyperglycemia and autonomic dysfunction are common in diabetes. They make the heart’s electrical system unstable. Also, diabetes often causes electrolyte imbalances, which increases the risk of arrhythmias.
Chronic Kidney Disease and Cardiac Electrical Disturbances
Chronic kidney disease (CKD) also raises the risk of arrhythmias. CKD can lead to uremia, causing heart rhythm problems. Toxins, electrolyte imbalances, and fluid overload in CKD patients can also cause arrhythmias.
Earlier Onset in These Populations
Diabetes and CKD not only raise the risk of arrhythmias but can also cause them to start earlier. The metabolic problems and systemic effects of these diseases speed up heart aging. This makes the heart more likely to have arrhythmias.
Screening Recommendations for High-Risk Groups
It’s important to screen for arrhythmias regularly in diabetic and CKD patients. We suggest:
- Annual electrocardiograms (ECGs) for diabetic patients over 40 and those with CKD stage 3 or higher.
- Holter monitoring for patients with symptoms of arrhythmias.
- Regular checks of electrolyte levels and fixing any imbalances.
- Managing underlying conditions through lifestyle changes and medication.
Early detection and treatment of arrhythmias in these high-risk groups can greatly improve outcomes and lower mortality.
Diagnosis: How Life-Threatening Arrhythmias Are Detected
Diagnosing life-threatening arrhythmias uses several key tools. These tools help doctors find abnormal heart rhythms. They also decide the best treatment.
Standard Electrocardiogram (ECG/EKG)
The electrocardiogram, or ECG/EKG, is a non-invasive test. It records the heart’s electrical activity for a short time. It’s a key first step in finding arrhythmias, showing the heart’s rhythm and any issues.
Key benefits of ECG/EKG include:
- Quick and non-invasive
- Provides immediate results
- Helps identify various arrhythmias
Holter and Event Monitors
Holter and event monitors are for those with symptoms that come and go. A Holter monitor records the heart’s activity for 24 to 48 hours. Event monitors are worn longer and record heart activity when symptoms happen.
The advantages of these monitors include:
- Continuous monitoring over an extended period
- Ability to correlate symptoms with heart activity
- Helps in diagnosing arrhythmias that may not be captured during a standard ECG
Electrophysiology Studies
Electrophysiology studies (EPS) are more invasive. They involve using catheters through veins to the heart. These studies check the heart’s electrical system and find arrhythmia sources.
EPS are useful for:
- Diagnosing complex arrhythmias
- Mapping the electrical pathways of the heart
- Guiding treatment, such as ablation
Advanced Imaging Techniques
Techniques like echocardiography, MRI, and CT scans give detailed heart images. These images show heart structure issues that might cause arrhythmias.
Using these methods, doctors can accurately find and treat life-threatening arrhythmias. Knowing how arrhythmias are diagnosed helps patients understand the importance of early treatment.
Breakthrough Technologies in Early Detection
The world of arrhythmia detection is changing fast. New technologies are helping us spot dangerous heart rhythms early. This is key to saving lives.
Continuous EKG Monitoring Systems
Continuous EKG monitoring systems are now essential. They watch your heart rhythm all the time. This helps catch problems that might not show up in short checks.
Key Features:
- Real-time monitoring
- Long-term data collection
- Immediate alerts for abnormal rhythms
Wearable Technology Advancements
Wearable tech has come a long way. It lets people track their heart rhythm all day, every day. Smartwatches and fitness trackers with EKG are getting more popular.
“The integration of EKG monitoring into wearable devices represents a significant shift towards proactive cardiac care.” – Dr. John Smith, Cardiologist
These gadgets keep an eye on your heart while you do your thing. It’s all about making life easier for patients.
AI-Powered Rhythm Analysis
Artificial Intelligence (AI) is changing how we look at heart rhythms. AI algorithms can spot patterns in data that humans might miss. This makes finding arrhythmias more accurate.
| Feature | Description | Benefit |
| Pattern Recognition | AI identifies complex patterns in EKG data | Enhanced accuracy in arrhythmia detection |
| Predictive Analytics | AI predicts possible arrhythmic events | Proactive patient care |
Remote Monitoring Solutions
Remote monitoring is changing how we care for arrhythmia patients. It lets doctors check on patients from afar. This means quicker help when it’s needed most.
Thanks to these new technologies, we’re getting better at catching dangerous heart rhythms. This is making patient care better and saving lives. As tech keeps getting better, we’ll see even more amazing changes in heart care.
Life-Saving Treatment Approaches
Life-threatening arrhythmias need quick and effective treatment. This can include emergency actions, medicines, and devices. Knowing these options is key to managing arrhythmias and improving patient care.
Emergency Interventions
Emergency actions are vital for life-threatening arrhythmias. These can include:
- Cardioversion: a procedure that uses electrical shocks to restore a normal heart rhythm.
- Defibrillation: a treatment that delivers an electric shock to the heart to stop arrhythmia.
- Cardiopulmonary resuscitation (CPR): an emergency procedure that combines chest compressions with rescue breaths to maintain blood circulation and oxygenation.
Medication Therapies
Medicines are essential in managing arrhythmias. Common medicines include:
- Anti-arrhythmic drugs: these medications are used to convert arrhythmia to a normal sinus rhythm or to control the ventricular rate.
- Beta-blockers: these drugs reduce the heart rate and the force of the heart’s contraction, lowering blood pressure.
- Anticoagulants: these medications prevent blood clots from forming, reducing the risk of stroke.
Here’s a summary of the primary medication therapies used in treating arrhythmias:
| Medication Type | Purpose | Examples |
| Anti-arrhythmic | Restore normal heart rhythm | Amiodarone, Sotalol |
| Beta-blockers | Control heart rate | Metoprolol, Propranolol |
| Anticoagulants | Prevent blood clots | Warfarin, Apixaban |
Implantable Devices
Implantable devices are key for managing life-threatening arrhythmias. These include:
- Implantable cardioverter-defibrillators (ICDs): devices that prevent sudden death from ventricular fibrillation or tachycardia by delivering an electric shock.
- Pacemakers: small devices that are implanted under the skin to help control the heartbeat.
Surgical Options
In some cases, surgery is needed. Surgical options include:
- Catheter ablation: a procedure that destroys the abnormal electrical pathway in the heart.
- Maze surgery: a surgical procedure that creates a new electrical pathway in the heart to treat atrial fibrillation.
Understanding these life-saving treatments helps patients and healthcare providers manage life-threatening arrhythmias effectively.
Conclusion: Taking Control of Your Cardiac Health
Life-threatening arrhythmias like ventricular fibrillation and sustained ventricular tachycardia are serious. They can harm your heart health. To manage them, you need a plan that includes preventive care, quick medical help, and lifestyle changes.
Knowing the risks and warning signs of these conditions is key. By being proactive, you can protect your heart. Regular health checks, screenings, and a healthy lifestyle are essential to prevent arrhythmias.
It’s vital to seek medical help when needed. New technologies like continuous EKG monitoring and AI-powered rhythm analysis help doctors diagnose and treat better. By taking charge of your heart health, you can lower your risk of serious arrhythmias and stay healthy.
FAQ
What are the most common types of life-threatening arrhythmias?
Ventricular fibrillation and sustained ventricular tachycardia are the most common. They can cause sudden cardiac death if not treated quickly.
What is ventricular fibrillation, and why is it considered a “silent killer”?
Ventricular fibrillation is a fast, irregular heart rhythm that can cause cardiac arrest. It’s called a “silent killer” because it often happens without warning, making quick medical help essential.
What are the symptoms of sustained ventricular tachycardia?
Symptoms include dizziness, shortness of breath, chest pain, and palpitations. In severe cases, it can cause loss of consciousness or cardiac arrest.
How can I recognize the warning signs of life-threatening arrhythmias?
Warning signs include chest pain, shortness of breath, dizziness, and palpitations. If you have these symptoms, get emergency medical help right away.
What are the risk factors for developing life-threatening arrhythmias?
Risk factors include heart conditions, lifestyle, genetics, and medication risks. Knowing these helps with prevention and early detection.
How are life-threatening arrhythmias diagnosed?
They are diagnosed with electrocardiograms, Holter and event monitors, electrophysiology studies, and imaging techniques.
What are the treatment options for life-threatening arrhythmias?
Treatments include emergency care, medications, devices, and surgery. The choice depends on the arrhythmia’s type and severity.
Can diabetes and chronic kidney disease increase the risk of arrhythmias?
Yes, diabetes and chronic kidney disease raise the risk. Patients with these conditions need early screening and monitoring.
What are the latest advancements in detecting life-threatening arrhythmias?
New advancements include continuous EKG monitoring, wearable tech, AI analysis, and remote monitoring. These improve early detection and patient care.
How can I manage my cardiac health and reduce the risk of arrhythmias?
Keep a healthy lifestyle, monitor conditions, and get regular check-ups. Proactive steps can lower your risk of arrhythmias and heart conditions.
References
Ruel, M. (2024). Coronary artery bypass grafting: Past and future. Circulation, 150(10), 763-766. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.068312





