Last Updated on December 1, 2025 by Bilal Hasdemir
Epilepsy surgery is a big step for those with seizures that don’t respond to medicine. A successful surgery can greatly improve life quality. But, it’s important to know what to expect during recovery.
After epilepsy brain surgery, many patients wonder about their recovery. The journey includes not just the first few days but also long-term changes and possible side effects. Our essential list: 20 things to expect after brain surgery. Get the awful, honest truth about recovery, pain, and life-changing effects.
Knowing what to expect can greatly help in the recovery. This guide aims to give a detailed look at the recovery process. It helps patients and their families get ready for what’s ahead.
Key Takeaways
- Understanding the recovery process is key for a good outcome.
- Immediate care after surgery is critical to avoid problems.
- Long-term recovery means making adjustments and dealing with side effects.
- Being ready can make the recovery better.
- Epilepsy surgery can greatly improve life for many patients.
The immediate post-operative period
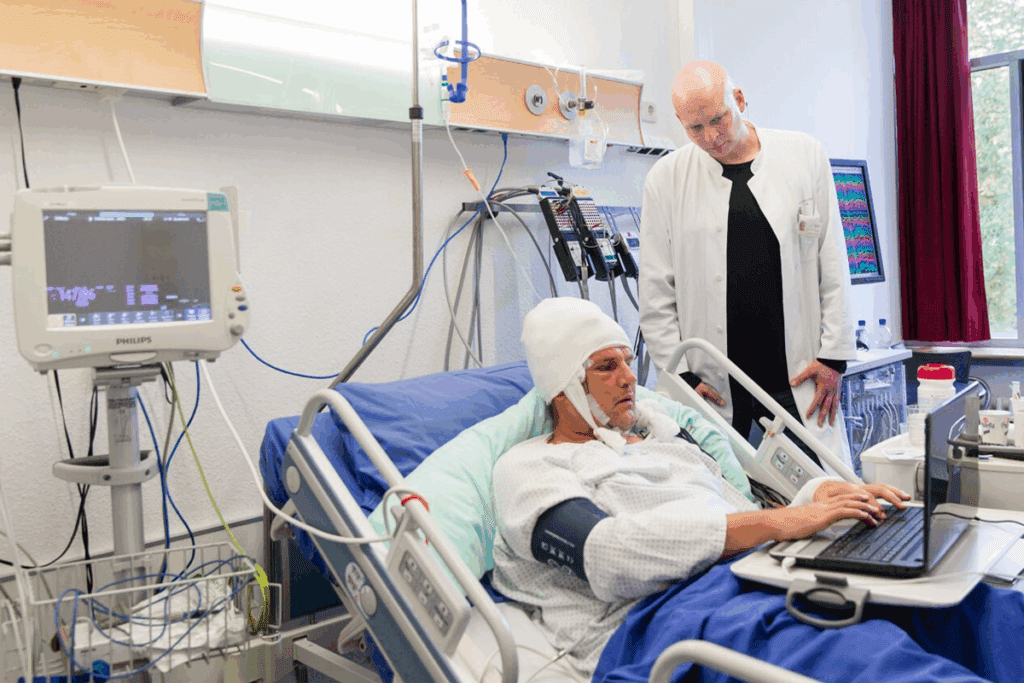
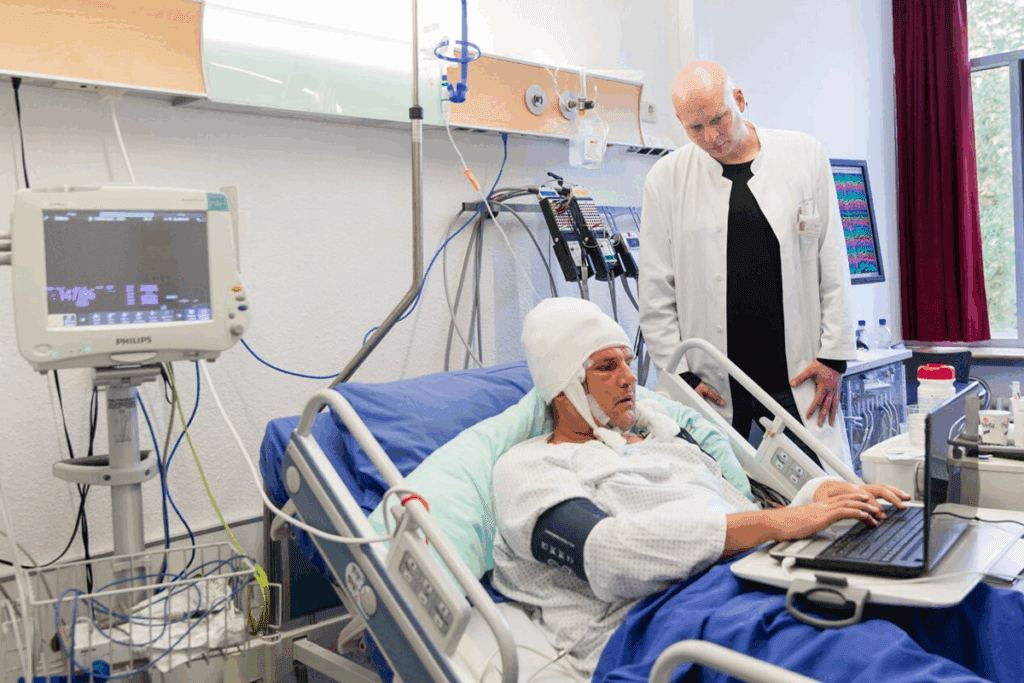
After surgery for epilepsy, the first days are key for a good recovery. Doctors and nurses watch closely to manage risks and keep patients comfortable and safe.
The First 24-48 Hours in Recovery
The first two days after surgery are very important. Patients often stay in the ICU for close monitoring. Doctors and nurses check vital signs and watch for complications.
Patients might feel confused or disoriented as they wake up. Caregivers focus on pain, comfort, and preventing problems like blood clots or pneumonia. Moving around is encouraged to help with recovery.
Managing Pain and Discomfort
Managing pain is a big part of care after surgery. Doctors use pain scales to make sure patients are comfortable. They aim to control pain without the side effects of opioids. They also treat other discomforts like nausea or headaches.
- Medications are given as needed for pain.
- Patients are asked to report their pain levels.
- Other ways to feel better, like relaxation techniques, are suggested.
Initial Medical Monitoring
Monitoring is constant in the first days after surgery. Doctors check neurological function and vital signs. They act fast if they see any problems. They watch blood pressure, heart rate, and oxygen levels closely.
Knowing what to expect in the first days helps patients and families. It prepares them for the healing journey ahead.
Hospital recovery and discharge planning
Recovering in the hospital after epilepsy surgery is key. It involves watching over the patient closely and getting ready for them to go home. This time is important for checking how the surgery is affecting them and setting up a good recovery plan at home.
Typical Length of Hospitalization
The time spent in the hospital after brain surgery varies. It can be a few days to over a week. The type of surgery, the patient’s health, and how they do after surgery all play a part.
Early Physical and Cognitive Assessments
Checking the patient’s physical and mental state early on is vital. These tests help doctors see how the surgery has affected them. They also help plan the right rehabilitation.
Medication Adjustments After Surgery
After surgery, changing medications is common to control seizures. Doctors watch how the patient reacts to their meds. They make changes to keep seizures low and side effects minimal.
Preparing for the Transition Home
Before leaving the hospital, teams help patients and their families get ready. They teach about wound care, managing meds, and follow-up visits. They also guide on slowly getting back to normal activities.
In summary, the recovery period after epilepsy surgery is complex. It involves careful monitoring, assessments, and planning for discharge. Knowing what to expect helps patients and their families through the recovery journey.
Different types of epilepsy surgeries and their specific recoveries
Epilepsy surgery is not a one-size-fits-all procedure. Various surgical techniques are used, each with its own recovery process. Knowing what to expect based on your surgery is important.
Temporal Lobectomy Recovery Considerations
Temporal lobectomy involves removing part of the temporal lobe. Recovery can take several days in the hospital. Post-operative care includes monitoring for neurological deficits and managing side effects like memory issues or mood changes. Recovery usually takes weeks to months.
Corpus Callosotomy Side Effects and Healing
Corpus callosotomy involves severing or partially severing the corpus callosum. This surgery is for severe seizure symptoms. Common side effects include cognitive and coordination issues, which can be temporary or persistent. Managing these side effects and rehabilitation are key to healing.
RNS Surgery Recovery Time and Expectations
RNS surgery involves implanting a device to detect and respond to abnormal brain activity. Recovery is generally shorter than other surgeries. Patients may experience some discomfort and swelling at the implant site, which resolves within a few weeks. Adjusting to the device can take months.
Laser Ablation Brain Surgery Recovery Process
Laser ablation is a minimally invasive technique used to treat epilepsy. The recovery process is generally quicker than traditional open surgery. Many patients can return home within a day or two. Post-operative care involves monitoring for complications and managing side effects, which are often minimal.
Understanding the recovery process for each type of epilepsy surgery helps patients and caregivers prepare. It allows for better management of expectations and optimization of the recovery experience.
Physical healing and incision care
After epilepsy surgery, taking care of the incision is key. Proper wound care and managing the surgical site are important. They help avoid complications and aid in healing.
Managing Epilepsy Surgery Scars
Dealing with scars from epilepsy surgery needs a mix of good wound care and sometimes extra treatments. At first, the scar might look red or swollen. This is normal as it heals.
It’s important to keep the wound clean and dry to avoid infection. Your doctor might suggest creams or dressings to help it heal faster and look better.
Proper Wound Care Techniques
Good wound care is key to prevent infection and ensure the incision heals right. This means gently washing the area with mild soap and water. Also, apply any dressings or creams as your doctor tells you to.
- Keep the incision site clean and dry
- Follow your healthcare provider’s instructions for dressing changes
- Monitor for signs of infection, such as redness, swelling, or discharge
When to Be Concerned About Your Incision
Some discomfort and redness around the incision are normal. But, watch out for signs of trouble. These include more pain, swelling, or discharge, and fever. If you see these, call your doctor right away.
Long-term Scar Appearance and Management
The scar will look different over time, usually becoming less noticeable. There are ways to make it less visible, like using silicone gel or sheeting, and massage.
By sticking to these tips and talking often with your healthcare provider, you can get the best results for your incision and recovery.
20 things to expect after brain surgery for epilepsy
Brain surgery for epilepsy is a big step. Knowing what to expect after can ease worries. Patients should be ready for various changes during recovery.
Physical sensations and changes
After surgery, patients might feel different physically. They could experience:
- Headaches and pain at the surgical site
- Numbness or tingling sensations
- Fatigue and weakness
- Changes in sensory perceptions
- Temporary difficulty with coordination and balance
Cognitive functions and challenges
Cognitive changes are common too. Patients might find it hard to:
- Remember familiar words or names
- Focus and concentrate
- Process information quickly
- Find the right words to say
- Feel confused or disoriented
Emotional responses and mood fluctuations
Emotions can shift a lot after surgery. Some patients might feel:
- Mood swings
- Anxiety or depression
- Irritability
- Emotional sensitivity
- Changes in personality
Sleep and energy level changes
Sleep and energy levels can change too. Patients might see:
- More sleepiness or trouble sleeping
- Energy ups and downs
- Need for more rest
- Hard time keeping a regular sleep schedule
- Fatigue that affects daily life
Knowing these changes can help patients get ready for recovery. It’s key to listen to the medical team and share any big changes or worries.
Week-by-week recovery timeline
Understanding the recovery process after epilepsy surgery is key for patients and their caregivers. The recovery time can vary a lot from person to person. Yet, most go through similar stages.
Weeks 1-2: Basic self-care and rest
The first phase focuses on rest and basic self-care. Patients should avoid hard activities and let their body heal.
Managing pain and discomfort is a top priority. Doctors often give medication to help with these symptoms.
Weeks 3-6: Gradual increase in activities
By weeks 3-6, patients can start doing more. This includes short walks, light stretching, and other easy exercises.
It’s important to listen to your doctor about how much to do. This helps avoid problems.
Months 2-3: Expanding your capabilities
By months 2-3, patients can do more. They can start doing some daily tasks again, but they should be careful.
Keep seeing your healthcare team. They will check on your progress and adjust your plan if needed.
Months 4-6: Approaching your new normal
By months 4-6, most patients are getting close to their new normal. They can do more strenuous activities, but some may have limits.
| Recovery Stage | Typical Activities | Guidelines |
| Weeks 1-2 | Rest, basic self-care | Avoid strenuous activities |
| Weeks 3-6 | Gradual increase in activities | Follow healthcare provider’s guidance |
| Months 2-3 | Expanding capabilities | Continue follow-ups with healthcare team |
| Months 4-6 | Approaching new normal | Continue rehabilitation therapies |
Managing common side effects after epilepsy surgery
Understanding and managing side effects is key to a smooth recovery after epilepsy surgery. Patients often face physical discomfort, cognitive, and speech challenges. Effective management of these side effects can significantly improve the overall recovery experience.
Headaches and Pain Management Strategies
Headaches are a common side effect following epilepsy surgery. Pain management strategies are key to alleviate this discomfort. Patients should use prescribed pain medications as directed by their healthcare provider. Techniques like deep breathing, relaxation, and adequate rest can also help manage headache severity.
- Follow the prescribed pain management regimen.
- Stay hydrated to help reduce headache severity.
- Practice relaxation techniques to minimize stress.
Swelling and Inflammation Reduction
Swelling and inflammation are typical after surgery. To reduce these effects, patients can apply cold compresses as recommended by their healthcare team. Elevating the head while resting can also help minimize swelling.
- Apply cold compresses as directed.
- Elevate your head while resting.
- Monitor swelling and report any concerns to your healthcare provider.
Memory and Cognitive Challenges
Cognitive challenges, including memory issues, can occur after epilepsy surgery. Strategies to manage these challenges include cognitive rehabilitation therapies and maintaining a routine to help structure daily activities.
- Engage in cognitive rehabilitation if recommended.
- Use memory aids like calendars and reminders.
- Establish a daily routine to minimize confusion.
Speech and Language Difficulties
Some patients may experience speech and language difficulties post-surgery. Speech therapy can be beneficial in addressing these challenges. Practicing speech exercises and working with a speech-language pathologist can help improve communication skills.
By understanding and addressing these common side effects, patients can better navigate their recovery journey after epilepsy surgery.
Post-surgical seizures: What you need to know
It’s important to know about post-surgical seizures after epilepsy surgery. Seizures after surgery can be a worry. But, knowing what to expect and how to handle them can make recovery better.
Why seizures might occur after surgery
Seizures can happen after surgery for many reasons. This includes the brain adjusting to surgery, leftover epileptic tissue, or stopping anti-seizure meds. Remember, having post-surgical seizures doesn’t mean the surgery failed.
Typical seizure patterns during recovery
During recovery, seizure patterns can vary. Some might see fewer and less severe seizures. Others might have seizures like before surgery. It’s key to watch these patterns to adjust treatment.
When to contact your medical team
Knowing when to get medical help is important. If seizures get more frequent or severe, or change in pattern, reach out to your team. They can help adjust your treatment.
Strategies to minimize seizure risk
Minimizing seizure risk involves sticking to medication, making lifestyle changes, and regular check-ups. This can include the right dosage of meds, managing stress, and getting enough sleep.
Understanding post-surgical seizures and how to manage them helps patients through their recovery.
Returning to daily activities and restrictions
Epilepsy surgery starts a new chapter in life. It’s key to know how to live daily life after surgery. Patients often wonder about going back to their usual routines.
Work and School Reintegration
Going back to work or school after surgery should be slow. Your doctor will give you advice based on your healing. Usually, you’ll need to take a few weeks off before returning.
You might need to change your schedule or workload. Students might need to take fewer classes or delay some activities.
Physical Activity Guidelines
Being active is important in recovery, but carefully. For a few weeks, avoid hard activities, heavy lifting, and bending. Start with light exercises like walking to help your health.
How Long After Brain Surgery Can You Drive?
Driving after brain surgery is a big worry for many. The time to start driving varies by person and local laws. Usually, wait at least 3 to 6 months, or until your doctor says it’s okay.
Always follow your doctor’s advice and be honest about your seizures and medication side effects.
Travel Considerations After Epilepsy Surgery
Planning travel after surgery needs careful thought. Talk to your doctor about your travel plans, including long trips or new places. It’s best to travel with someone and have access to medical care where you’re going.
Also, remember your seizure medicine schedule, even when traveling across time zones.
Long-term side effects of brain surgery for epilepsy
The journey after epilepsy surgery is about understanding and managing long-term side effects. The surgery aims to reduce or stop seizures. It’s important for patients and caregivers to know about possible long-term changes.
Cognitive changes that may persist
Cognitive changes can happen after surgery, affecting memory, attention, or speed. Some patients might see improvements, while others might see declines. For example, surgeries in the temporal lobe can affect verbal memory. It’s key to have good pre-surgical counseling and post-surgical follow-up to track these changes.
Physical side effects over time
Physical side effects can change over time. Some patients might have ongoing weakness, numbness, or sensory changes. For instance, corpus callosotomy can affect motor control or coordination. Regular physical therapy can help manage these effects.
Emotional and psychological long-term effects
The emotional and psychological impact of surgery can be big. Some patients see mood improvements and better overall well-being. But others might face depression, anxiety, or mood swings.
“The psychological adjustment after surgery can be as challenging as the physical recovery,” notes a study on post-surgical outcomes.
Support from mental health professionals is very helpful in dealing with these changes.
Managing chronic symptoms
Managing chronic symptoms after surgery needs a multi-faceted approach. This includes adjusting medications, physical therapy, cognitive rehab, and psychological support. A tailored rehabilitation plan can greatly improve a patient’s quality of life. Patients should work closely with their healthcare team to manage long-term side effects.
In conclusion, while epilepsy surgery can greatly reduce seizures, it comes with long-term side effects that need careful management. By understanding these effects and working with healthcare providers, patients can improve their outcomes and quality of life.
Rehabilitation therapies and brain recovery
After surgery for epilepsy, patients need various therapies to recover. These therapies help them regain strength, cognitive skills, and independence.
Physical Therapy Approaches
Physical therapy is key in the recovery process. It aims to restore strength, flexibility, and mobility. Physical therapists create custom exercise plans for each patient’s needs.
Cognitive Rehabilitation Techniques
Cognitive rehabilitation helps patients overcome cognitive challenges from surgery. It includes memory training, attention exercises, and strategies for better problem-solving.
Speech and Language Therapy
Speech and language therapy is vital for those struggling with communication after surgery. Therapists work to improve speech clarity, comprehension, and language skills.
Occupational Therapy for Daily Living
Occupational therapy helps patients do daily tasks on their own. Therapists assist in adapting to physical or cognitive limitations, boosting independence and confidence.
| Therapy Type | Focus | Goals |
| Physical Therapy | Restoring physical strength and mobility | Improve physical function, reduce pain |
| Cognitive Rehabilitation | Addressing cognitive difficulties | Enhance memory, attention, problem-solving |
| Speech and Language Therapy | Improving communication skills | Enhance speech clarity, comprehension |
| Occupational Therapy | Promoting independence in daily activities | Adapt to limitations, improve confidence |
By using these therapies, people can greatly improve their lives after epilepsy surgery.
Quality of life changes after epilepsy surgery
Epilepsy surgery changes a patient’s life in many ways. It’s not just about the surgery itself. The long-term effects on a patient’s life are just as important.
Seizure Freedom Statistics and Outcomes
One big change is the chance for seizure freedom. Many patients see a big drop in seizures or even stop having them. For example, a common surgery, temporal lobectomy, can lead to seizure freedom in 50% to 80% of cases.
Medication Reduction Possibilities
If seizures decrease or stop, patients might not need as much medication. This can greatly improve life by reducing side effects like tiredness and brain fog.
Key benefits of medication reduction include:
- Reduced risk of medication side effects
- Improved cognitive function
- Enhanced overall well-being
- Better control over one’s health
Social and Relationship Improvements
Epilepsy can make social life tough due to unpredictable seizures and stigma. But, with better seizure control, things can get better. Patients might feel more confident, have better family relationships, and be more independent.
- Increased confidence in social situations
- Improved family dynamics and relationships
- Greater independence
- Enhanced participation in activities previously avoided due to fear of seizures
Career and Education Opportunities
Improved seizure control can open up new doors in work and school. This means patients might be able to drive, work better, go to school, or advance in their careers.
- The ability to drive, opening up more job opportunities
- Increased productivity at work or school
- Pursuit of higher education or career advancement
- Greater participation in extracurricular activities
In conclusion, epilepsy surgery can greatly improve life. It can lead to seizure freedom, less medication, better social life, and more opportunities in work and school.
Conclusion: Embracing your new journey after epilepsy surgery
Understanding what to expect after epilepsy surgery can make your recovery easier. Epilepsy surgery results can vary, but knowing what to expect helps prepare you better.
Recovery means dealing with physical and mental changes, new medicines, and side effects. The first few weeks can be tough, but many people see big improvements in their life quality.
Starting your new journey after surgery takes patience, strength, and support from friends and family. By staying informed and working with your doctors, you can improve your surgery results. This way, you can look forward to a life with fewer seizures.
FAQ
What is the typical recovery time after epilepsy surgery?
Recovery time varies. It depends on the surgery type and individual factors. Generally, it takes several weeks to a few months.
How long will I be in the hospital after epilepsy surgery?
Hospital stay varies. It’s usually a few days to a week. This depends on surgery complexity and patient health.
What are the common side effects after epilepsy surgery?
Side effects include headaches, swelling, and cognitive challenges. Fatigue is also common. These can be managed with rest and medication.
Can I stil have seizures after epilepsy surgery?
Yes, some patients may have seizures after surgery. But, the frequency and severity often lessen over time.
How long after brain surgery can I drive?
Driving rules vary. They depend on surgery type and individual factors. Usually, patients can’t drive for weeks to months.
What are the long-term side effects of brain surgery for epilepsy?
Long-term effects include cognitive changes and physical limitations. Emotional challenges can also occur. These can be managed with therapy and lifestyle changes.
Will I need rehabilitation therapy after epilepsy surgery?
Many patients benefit from therapy. This includes physical, cognitive, speech, and occupational therapy. It helps in recovery and improves quality of life.
Can epilepsy surgery improve my quality of life?
Yes, surgery can improve life quality. It reduces seizure frequency, minimizes medication, and enhances well-being.
How will epilepsy surgery affect my cognitive abilities?
Cognitive changes can happen after surgery. The extent varies by surgery type and individual factors.
What are the benefits of Responsive Neurostimulation (RNS) surgery?
RNS surgery can reduce seizures and improve life quality. It delivers targeted electrical stimulation to the brain.
How do I manage my epilepsy surgery scar?
Proper wound care and scar management can minimize scar appearance. They promote healing.
Can I return to work or school after epilepsy surgery?
Yes, many can return to work or school after recovery. The timing and nature depend on individual factors and surgery type.
Are there any travel restrictions after epilepsy surgery?
Travel rules vary. They depend on surgery type and individual factors. Patients often avoid areas with limited medical facilities.
How can I minimize the risk of seizures after epilepsy surgery?
To reduce seizure risk, follow medication regimens, get enough rest, and manage stress.
What are the possible risks and complications of epilepsy surgery?
Risks include infection, bleeding, and cognitive or physical changes. Discuss these with a healthcare provider.
References
National Institutes of Health. Evidence-Based Medical Insight. Retrieved from https://www.ninds.nih.gov/health-information/disorders/epilepsy#toc-what-are-treatments-for-epilepsy-