
It’s vital to spot a third-degree heart block on an ECG quickly. This is because it can be very dangerous if not treated right away.
Third-degree atrioventricular (AV) block means there’s no connection between the heart’s upper and lower chambers. This leads to an irregular heartbeat 3 degree heart block ecg.
At Liv Hospital, we stress the need to know the main ECG signs of this condition. These include AV dissociation and escape rhythms. This knowledge helps us give the best care fast.
Key Takeaways
- Understanding the ECG signs of third-degree AV block is critical for diagnosis.
- AV dissociation is a hallmark of third-degree heart block.
- Escape rhythms can occur in the absence of normal AV conduction.
- Prompt recognition is essential for effective management.
- Liv Hospital provides internationally benchmarked cardiac care.
Understanding Third-Degree Heart Block: Pathophysiology and Significance
Third-degree heart block is a serious form of AV block. It means the atria and ventricles don’t work together. This happens when electrical signals from the atria can’t reach the ventricles.
Definition and Electrical Conduction Abnormalities
Third-degree AV block, or complete heart block, means no electrical signals pass from the atria to the ventricles. This leads to more P waves than QRS complexes on an electrocardiogram (ECG). There’s no set pattern between them.
This condition can come from many things. It might be due to medical procedures, genetic issues, heart attacks, or blocked arteries.
The heart’s electrical system is messed up in third-degree heart block. This causes the atria and ventricles to beat on their own. It can really hurt the heart’s function and the patient’s health.
Prevalence and Clinical Importance
Third-degree heart block is not common but is very serious. It can cause severe symptoms and affect how well a patient does.
It’s key because it often needs quick medical help. This might include pacing to fix the heart rhythm and ensure it works right. Doctors need to know about third-degree heart block to treat it well.
The Fundamental Characteristics of 3 Degree Heart Block ECG
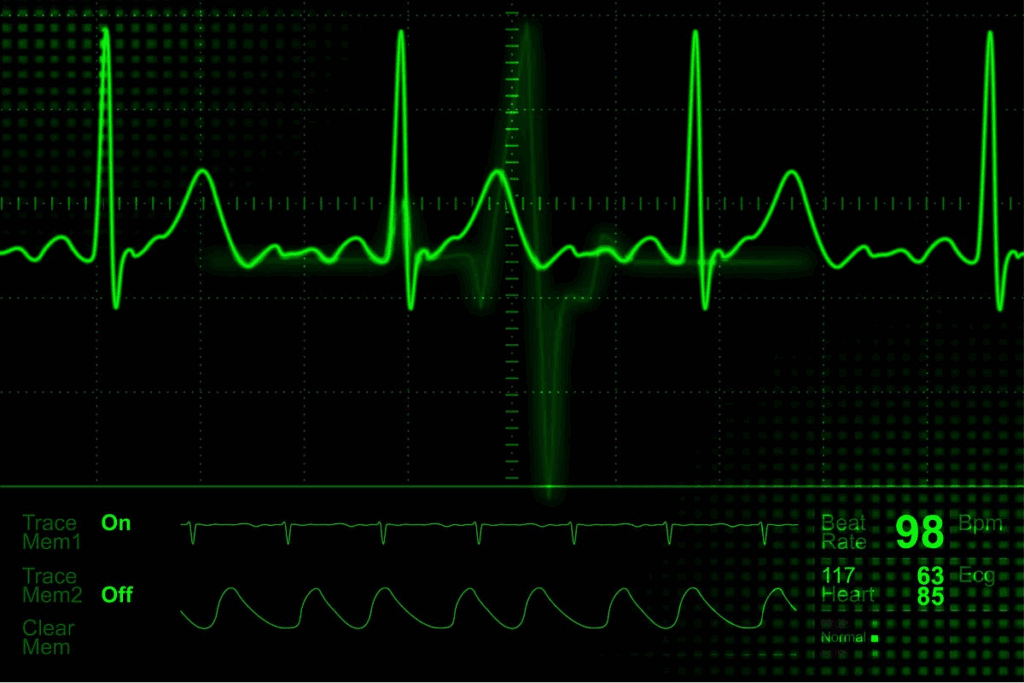
Understanding the basics of 3 degree heart block ECG is key for correct diagnosis and care. The ECG is vital for spotting third-degree atrioventricular (AV) block. This is when there’s a total stop in electrical signals from the atria to the ventricles.
Complete AV Dissociation: The Hallmark Finding
Third-degree heart block is marked by complete AV dissociation. This means the atria and ventricles beat on their own. On an ECG, you see regular P-P and R-R intervals but no link between P waves and QRS complexes. This leads to the atria beating faster than the ventricles, a key sign of complete AV block ECG.
“The presence of complete AV dissociation is a key diagnostic criterion for third-degree heart block,” highlighting the importance of meticulous ECG analysis. The absence of conducted impulses between the atria and ventricles results in the atria and ventricles beating independently, a condition that can lead to significant hemodynamic consequences if not properly managed.
P Wave and QRS Complex Relationships
In third-degree AV block, the P waves and QRS complexes don’t follow each other. The P waves, showing atrial depolarization, beat faster than the ventricular rate shown by the QRS complexes. The ECG shows P waves “marching through” the QRS complexes without a consistent PR interval, a key sign of 3rd degree AV block ECG. This is a critical finding that doctors must spot to diagnose and treat this condition well.
The ventricular rate in third-degree heart block is usually slower than the atrial rate. The QRS complexes can be narrow or wide, depending on the block’s location and the escape pacemaker. Knowing these details is vital for diagnosing and managing patients with 3rd degree heart block.
Key Finding #1: AV Dissociation with Independent Atrial and Ventricular Rhythms
In third-degree heart block, a key ECG finding is AV dissociation. This shows that the atria and ventricles beat independently. It means there’s no electrical connection between them.
Identifying Complete Electrical Dissociation
To spot complete electrical dissociation, we look for signs on the ECG. The ECG shows that the atria and ventricles beat on their own. This can happen in different parts of the heart, leading to various rhythms.
On the ECG, we see P waves without QRS complexes. This shows that the atria and ventricles don’t work together.
Differentiating from Other Forms of AV Block
It’s important to tell third-degree heart block apart from other AV block types. Unlike second-degree AV block, third-degree doesn’t have P waves followed by QRS complexes. This difference helps doctors diagnose complete heart block correctly.
Knowing how to spot AV dissociation on an ECG is key for treating 3rd degree heart block. By recognizing the independent rhythms, doctors can give the right care to patients.
Key Finding #2: P Waves and QRS Complexes – The Diagnostic Pattern
In third-degree heart block, the ECG shows a key pattern. This pattern is vital for diagnosing the condition. It helps us understand the block’s impact on patient care.
P Wave Frequency Exceeding QRS Complexes
Third-degree heart block is marked by a specific ECG pattern. The atrial rate, shown by P waves, is usually higher than the ventricular rate, shown by QRS complexes. This leads to more P waves than QRS complexes on the ECG. This is a key sign of complete third-degree heart block.
When we examine the ECG, we look for this rate difference. It shows that the atria and ventricles are beating on their own.
Absence of P-R Relationship
Another important feature of third-degree heart block is the lack of a consistent P-R relationship. In normal heart function, the P-R interval shows the time from atrial to ventricular depolarization. But in third-degree heart block, this interval is not fixed. It varies and is unpredictable.
A leading cardiologist notes,
“The lack of coordination between atrial and ventricular contractions is a telltale sign of complete heart block.”
This lack of a consistent P-R relationship is a key diagnostic criterion. It helps us tell third-degree heart block apart from other AV block types.
By spotting these ECG patterns, doctors can accurately diagnose third-degree heart block. They can then start the right treatment.
Key Finding #3: Escape Rhythms in Third-Degree Heart Block
In third-degree heart block, escape rhythms are key. They help keep the heart beating. These rhythms come from hidden pacemaker cells in the heart.
Junctional Escape Rhythms: Characteristics and Implications
Junctional rhythms start in the AV junction and beat 40-60 times a minute. They have a narrow QRS complex, unless there’s a block. This means the block is likely in the AV node.
Patients with these rhythms usually have better heart function. This is because the rhythm is faster and more organized.
Ventricular Escape Rhythms: Characteristics and Implications
Ventricular rhythms start in the ventricles and beat slower, 20-40 times a minute. They have a wide QRS complex, showing they start further down. These rhythms often mean a worse outlook for the heart.
Knowing about these rhythms on 3rd degree heart block rhythm strips is vital. It helps doctors diagnose and treat third-degree heart block.
It’s important to tell junctional and ventricular rhythms apart. Junctional rhythms are usually better for the heart. Ventricular rhythms might need more serious treatment to keep the heart stable.
Key Finding #4: Heart Rate Variations and Hemodynamic Consequences
The fourth key finding in diagnosing third-degree heart block is about heart rate changes. These changes affect how well the heart works. In complete heart block, the heart rate can change a lot, leading to different symptoms.
Typical Ventricular Rates in Complete Heart Block
In third-degree heart block, the heart rate is set by the escape rhythm. For ventricular escape rhythms, the rate is usually between 20-40 beats per minute. This is much slower than normal and can cause the heart to pump less effectively.
Clinical Impact of Different Escape Rhythm Rates
The effects of different heart rates vary a lot. Lower heart rates can lead to serious problems. These include poor blood flow to important organs, causing symptoms like dizziness, fatigue, and even fainting.
| Ventricular Rate (bpm) | Clinical Implications |
| 40-60 | Mild symptoms, potentially asymptomatic |
| 20-40 | Significant symptoms, risk of decreased cardiac output |
| <20 | Severe symptoms, high risk of cardiac arrest |
One study found that the heart rate in complete heart block is very important. It affects how well the heart works and the symptoms the patient has. Knowing about these changes helps doctors take better care of their patients.
Key Finding #5: QRS Complex Morphology and Its Clinical Significance
In third-degree AV block, the QRS complex shape is key. It tells us where the escape rhythm starts and its importance. The QRS complexes can be narrow or wide, showing where the escape pacemaker is.
Narrow vs. Wide QRS Complexes
The QRS complex width is very important for diagnosing third-degree AV block. Narrow QRS complexes usually mean the block is in or above the AV node. On the other hand, wide QRS complexes suggest a block in the ventricles.
- Narrow QRS complexes:
- Junctional escape rhythm
- Block likely above or within the AV node
- Wide QRS complexes:
- Ventricular escape rhythm
- More distal block within the ventricles
Locating the Site of Block Using QRS Morphology
The QRS complex shape can show where the block is. By looking at a 3rd degree AV block ECG strip, doctors can tell if the rhythm starts in the AV junction or the ventricles. This helps them understand the problem better and make the right treatment choices.
Looking closely at the QRS complex shape gives us important clues. It helps us understand the third-degree AV block better and its possible effects on health.
Key Finding #6: Rhythm Strip Analysis and Diagnostic Confirmation
Diagnosing third-degree heart block needs a close look at the ECG strip. We must check the rhythm strip for complete AV dissociation, a key sign of this condition. A top cardiologist says, “The ECG is the best way to spot third-degree heart block.”
“The ECG is the gold standard for diagnosing third-degree heart block.”
The ECG strip shows AV dissociation. This means the heart’s upper and lower chambers beat on their own.
Techniques for Accurate Identification on ECG Strips
To spot third-degree heart block on an ECG strip, look for no fixed PR interval. Also, check for P waves and QRS complexes that beat on their own. It’s key to examine different leads and a long enough ECG strip to be sure. We should use a step-by-step method to review the ECG strip. This includes looking at P wave and QRS complex shapes, measuring PR intervals, and checking the heart rate.
- Assess P wave and QRS complex morphology
- Measure PR interval and ventricular rate
- Look for AV dissociation
Common Pitfalls in Diagnosis
Even though ECG strip analysis is critical, there are traps to watch out for in diagnosing third-degree heart block. These include mistaking ECG noise for third-degree heart block or missing AV dissociation. When looking at ECG strips, we must be careful, even more so in complex cases or those with pacemakers. We should also think about the patient’s symptoms and overall health to make sure we’re right.
By carefully checking the ECG strip and avoiding common mistakes, we can accurately diagnose and treat patients with third-degree heart block.
Key Finding #7: Risk Stratification and Emergency Management
Risk stratification is key in managing third-degree heart block. It guides doctors in making decisions and helps avoid bad outcomes.
Identifying High-Risk Patients
Patients with third-degree heart block and low ventricular escape rhythms face a higher risk. They need close monitoring and aggressive management to avoid serious problems. Heart diseases like coronary artery disease or cardiomyopathy also raise the risk.
A leading cardiologist said,
“The key to managing third-degree heart block lies in early identification of high-risk patients and timely intervention to prevent complications.”
We must watch closely for these patients and take steps to lower their risk.
Indications for Emergency Pacing
Emergency pacing might be needed for high-risk patients with third-degree heart block. The decision to pace is based on symptoms, how well the heart is working, and symptoms like fainting or near-fainting.
The signs for emergency pacing include:
- Symptoms of slow heart rate
- Heart not working well
- Escape rhythms that don’t keep blood flowing well enough
We must be ready to act fast when these signs show up. Quick action can greatly improve a patient’s chances of recovery.
Conclusion: Integrating ECG Findings into Clinical Practice
It’s key to use ECG findings well in patient care. This helps in making the right diagnosis and managing patients with 3 degree heart block. Knowing the important signs in 3 degree heart block ECG is vital for good care.
We talked about how third degree AV block affects patient care. The ECG signs, like escape rhythms and QRS complex shape, help understand the block’s impact. These signs are important for patient care.
Understanding these signs helps doctors sort out patient risks and act quickly when needed. Using ECG findings well in care means better health for patients with 3 degree heart block. This leads to better results for patients.
FAQ
What is third-degree heart block, and how is it diagnosed on an ECG?
Third-degree heart block, also known as complete heart block, is a serious condition. It happens when there’s a complete break in the electrical signals between the heart’s upper and lower chambers. Doctors use an ECG to spot this by looking for P waves and QRS complexes that don’t match up.
What are the characteristic ECG findings in third-degree heart block?
The ECG shows a few key signs. These include AV dissociation, where P waves and QRS complexes don’t link up. Also, P waves beat faster than QRS complexes, and there’s no P-R relationship. Plus, you might see escape rhythms, which can start from the junction or ventricles.
How do you differentiate third-degree heart block from other forms of AV block on an ECG?
Third-degree heart block stands out because of complete AV dissociation. This means P waves and QRS complexes don’t connect, unlike in first or second-degree AV blocks where some connection is seen.
What is the significance of escape rhythms in third-degree heart block?
Escape rhythms are key because they control the heart rate. A faster rhythm usually means the rhythm starts from the junction, which is more stable. A slower rhythm might start from the ventricles and could be less stable.
How does the QRS complex morphology help in diagnosing third-degree heart block?
The shape of the QRS complex can tell where the block is and where the rhythm starts. A narrow QRS complex usually means the rhythm starts from the junction. A wide QRS complex suggests it starts from the ventricles.
What are the typical ventricular rates in complete heart block, and what are their clinical implications?
Ventricular rates usually range from 40 to 60 bpm for junctional rhythms. Ventricular rhythms are slower. The rate affects how well the heart works, with higher rates being better.
How do you analyze a rhythm strip for diagnosing third-degree heart block?
To analyze a rhythm strip, look for complete AV dissociation. Identify P waves and QRS complexes. Check if there are escape rhythms and where they start. Knowing common mistakes is also important.
What are the indications for emergency pacing in third-degree heart block?
You need emergency pacing if the patient is unstable, has severe symptoms, or a very slow heart rate. This is to keep the heart pumping well enough.
How do you identify high-risk patients with third-degree heart block?
High-risk patients show symptoms like fainting, dizziness, or heart failure signs. Their ECG might show a slow heart rate or wide QRS complexes.
What is the clinical importance of understanding third-degree heart block?
Knowing about third-degree heart block is vital for correct diagnosis and treatment. It helps spot high-risk patients and decide on emergency pacing when needed.
References:
- Martinez-Lemus, L. A. (2012). The dynamic structure of arterioles. Basic & Clinical Pharmacology & Toxicology, 110(1), 5-11.https://pubmed.ncbi.nlm.nih.gov/21989114/




































