Last Updated on November 25, 2025 by Ugurkan Demir

At Liv Hospital, we know how vital it is to quickly spot and treat third-degree AV block. This serious heart issue means the atria and ventricles don’t work together. Discover 3rd degree AV block ECG findings and how to diagnose complete heart block quickly.
Third-degree AV block is a serious problem that needs quick action. Our team is dedicated to top-notch care for all patients, including those from abroad.
This condition is marked by the ICD-10 code I44.2, showing a complete block between the heart’s chambers. Spotting third-degree AV block early on an ECG is key to good care and treatment.
Third-degree AV block, also known as complete heart block, is a serious heart condition. It happens when electrical signals from the atria can’t reach the ventricles. This leads to the atria and ventricles beating on their own, without coordinating.
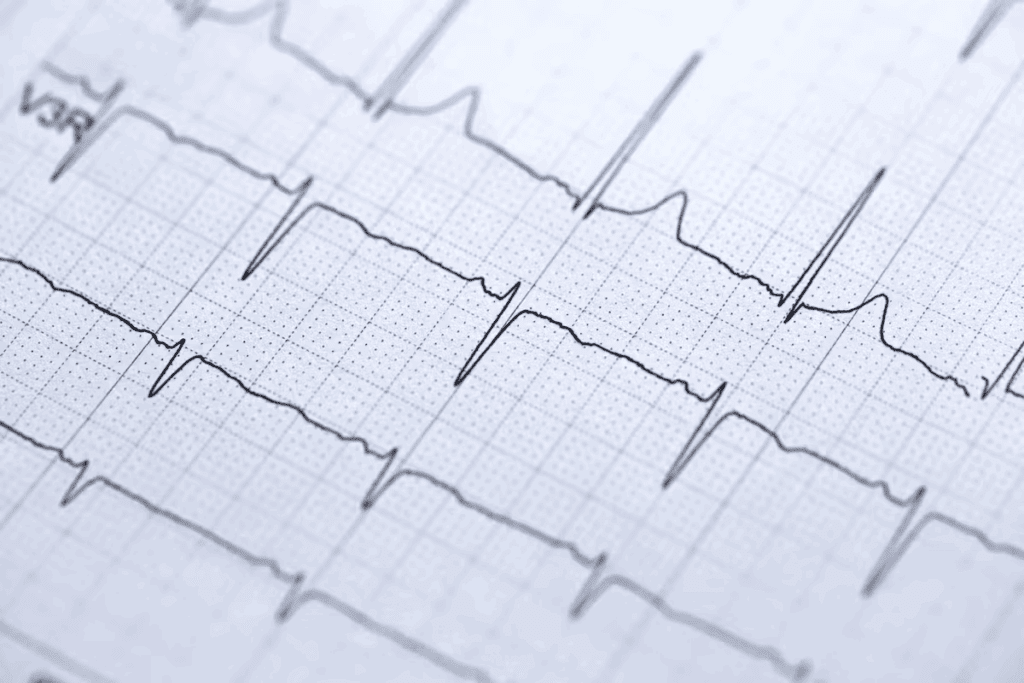
This condition means there’s no electrical connection from the atria to the ventricles. On an ECG, it shows regular P waves and QRS complexes with no consistent relationship. This is called AV dissociation.
Third-degree AV block is not common but is very serious. It can happen due to heart disease, heart attacks, or some medicines. It needs quick diagnosis and treatment to avoid serious problems.
| Clinical Setting | Prevalence | Clinical Implication |
| Degenerative Heart Disease | Common in elderly | High risk of heart failure |
| Ischemic Heart Disease | Associated with MI | Increased mortality risk |
| Medication-Induced | Variable | Reversible with medication adjustment |
Knowing about third-degree AV block is key for doctors to care for their patients well.
To understand third-degree AV block, we must look at its pathophysiology and how it affects the heart. The heart’s normal conduction system is key to a synchronized heartbeat.
The heart’s conduction system includes the SA node, AV node, Bundle of His, and the ventricular system. The SA node is the heart’s natural pacemaker. It sends electrical impulses to the AV node and then to the ventricles, making them contract.
In third-degree AV block, there’s a complete break in electrical signals between the atria and ventricles. This leads to AV dissociation. Atrial and ventricular beats happen on their own. Atrial rates are usually faster, controlled by a ‘junctional escape rhythm’ or ‘ventricular escape rhythm.’
The main sign is that there’s
Knowing how AV dissociation works is key to diagnosing and treating complete heart block. It helps doctors spot the condition on an ECG and treat it right.
It’s important to know why 3rd degree heart block happens. This knowledge helps doctors find the right treatment. Many things can cause this condition, and finding the main cause is key.
In older people, the heart’s electrical system can wear out. This can cause third-degree AV block. The heart’s tissues can become stiff and hard, making it hard for signals to move.
Heart disease caused by blocked blood flow is a big reason for 3rd degree heart block. A heart attack can harm the AV node or bundle branches. This can stop the heart’s electrical signals.
Some medicines can cause third-degree AV block. They might affect the AV node or slow the heart rate. Beta-blockers, calcium channel blockers, and anti-arrhythmic drugs are examples.
Other reasons for 3rd degree heart block include heart muscle diseases and diseases like sarcoidosis. It can also happen in people with heart problems from birth. Sometimes, it’s a side effect of heart surgery or Lyme disease.
A doctor said, “Finding out why someone has 3rd degree heart block is critical. It helps doctors choose the best treatment, like medicine or a pacemaker.”
To diagnose third-degree AV block on an ECG, we look for seven key signs. These signs show how serious this heart problem is. They help doctors tell it apart from other heart block issues and decide the best treatment.
Complete AV dissociation is a key sign of third-degree AV block. It means there’s no link between P waves and QRS complexes. This happens because the block is at the AV node or below, stopping normal conduction.
In third-degree AV block, P waves are usually regular. This shows the atrial rhythm is not affected by the block. This regularity is important for diagnosing the condition.
QRS complexes in third-degree AV block happen on their own, not with P waves. They come from a ventricular or junctional escape rhythm. The shape and width of these complexes can tell us more about their source.
A key feature of third-degree AV block is that P waves and QRS complexes don’t follow each other. This is because there’s a complete block in the electrical pathway between the atria and ventricles.
The last three important ECG signs are a slow ventricular rate, a steady P wave rate, and an escape rhythm. The ventricular rate is usually between 20-40 bpm if it’s ventricular, or 40-60 bpm if it’s junctional.
| ECG Finding | Description |
| Complete AV Dissociation | No association between P waves and QRS complexes |
| Regular P Waves | Atrial rhythm is regular and unaffected |
| Independent QRS Complexes | QRS complexes occur independently of P waves |
| No Relationship Between P Waves and QRS Complexes | Absence of consistent PR interval |
It’s vital to spot these seven ECG signs to accurately diagnose and manage third-degree AV block. Knowing these signs helps doctors quickly find patients who need pacing or other treatments.
In third-degree AV block, the heart’s natural pacemaker is disrupted. This often leads to a junctional escape rhythm. This rhythm is a key response that helps keep the heart beating when the usual pathway is blocked.
A junctional escape rhythm starts in the AV junction. This includes the AV node and the surrounding tissue. On an electrocardiogram (ECG), it shows narrow QRS complexes. These complexes are usually without preceding P waves or with retrograde P waves.
The heart rate of a junctional escape rhythm is between 35 to 50 beats per minute (bpm). This rate is slower than normal but enough to keep blood flowing well when there’s no normal rhythm.
One key feature of a junctional escape rhythm is narrow QRS complexes. This shows that the heart’s ventricles are activated through the normal His-Purkinje system. This is different from ventricular escape rhythms, which have wide QRS complexes.
Knowing about junctional escape rhythm is key for diagnosing and treating third-degree AV block. Doctors need to recognize the ECG signs, like heart rate and QRS complex width, to give the right care.
In third-degree AV block, the heart’s electrical system is badly damaged. This often leads to a ventricular escape rhythm. This rhythm helps the heart keep beating, but at a slower pace.
A ventricular escape rhythm has a unique ECG look. The QRS complexes are wide and odd, showing they come from the ventricles. This is different from the narrower complexes seen in other rhythms.
The heart rate in a ventricular escape rhythm is usually 20-40 beats per minute. This slow rate can cause symptoms like tiredness, dizziness, and shortness of breath.
The wide QRS complexes are a key sign of ventricular escape rhythms. These complexes come from ventricular pacemaker cells when the AV node is blocked. On an ECG, they look like broad, odd deflections.
Key features of ventricular escape rhythm include:
It’s key for healthcare pros to spot third-degree AV block on ECG strips. We’ll show you how to do it step by step.
To spot third-degree AV block, we need to look closely at the ECG strip. First, we search for complete AV dissociation. This means P waves and QRS complexes don’t match up. Next, we check for regular P waves and independent QRS complexes. Lastly, we make sure there’s no connection between P waves and QRS complexes.
By following these steps, we can be sure we’ve found third-degree AV block on ECG strips.
Third-degree AV block shows up in a special way on rhythm strips. We see a regular atrial rhythm and a
To quickly spot third-degree AV block, here’s what to do:
By using these tips, we can quickly and accurately find third-degree AV block on ECG strips. This helps us treat patients fast.
Third-degree AV block is a serious condition that needs quick action. It can cause big problems with blood flow. We’ll look at how it affects patients and the dangers it brings.
Bradycardia is a big worry with third-degree AV block. It means the heart beats too slow. This can make people feel dizzy and have trouble breathing.
People with third-degree AV block often feel very tired. They might also faint or feel like they’re going to faint. These problems happen because the heart can’t beat right.
| Symptom | Description |
| Fatigue | A general feeling of tiredness or weakness |
| Syncope | Fainting or loss of consciousness |
| Presyncope | Near-fainting episodes |
Third-degree AV block is a big risk for sudden cardiac death. If not treated fast, it can cause dangerous heart rhythms.
Some people might have Stokes-Adams attacks. These are sudden times when they lose consciousness because their heart stops working. These attacks are very serious.
Doctors say, “Third-degree AV block needs quick heart monitoring and might need a pacemaker to avoid serious problems.”
Complete 3rd degree heart block is a serious medical issue that needs quick action. We start by closely watching the heart and might put in a pacemaker to help.
The first thing we do is make sure the patient is stable. We check their blood pressure and make sure their organs are getting enough blood. This is key to keeping them safe.
Putting in a temporary pacemaker is often needed. This is true if the patient is feeling bad or if their heart is not beating right. We can do this through the skin or through a vein.
| Temporary Pacing Method | Indications | Advantages | Disadvantages |
| Transcutaneous Pacing | Emergency situations, symptomatic bradycardia | Quick to establish, non-invasive | Painful, limited duration |
| Transvenous Pacing | Prolonged pacing need, unstable patients | More stable, can be used for longer periods | Invasive, requires expertise |
Medicine might be used to help the patient feel better while we get ready for pacing. Atropine is often given, but it doesn’t always work well.
“Atropine is often administered in cases of symptomatic bradycardia, though its effectiveness in complete heart block is not guaranteed.”
— Clinical Guidelines for Bradyarrhythmias
It’s very important to keep a close eye on the heart. We watch the heart rate and rhythm closely. This helps us decide what to do next.
Pacemaker implantation is the best treatment for third-degree AV block. It helps patients by regulating their heartbeat. This ensures the heart beats at the right rate and rhythm.
Patients with third-degree AV block need a permanent pacemaker. Those with symptoms like syncope, fatigue, or heart failure definitely need pacing.
There are different pacemakers available. These include single-chamber, dual-chamber, and biventricular pacemakers. The right one depends on the patient’s heart condition.
The pacemaker implantation is done under local anesthesia. Leads are inserted into the heart through a vein. They connect to the pacemaker generator under the skin.
After the procedure, patients are watched for any issues. They learn how to take care of their pacemaker. This includes checking its function and avoiding device interactions.
A leading cardiologist says, “Pacemaker implantation has changed how we treat third-degree AV block. It greatly improves patient outcomes and quality of life.“
Different groups, like kids and pregnant women, face unique challenges with third-degree AV block. It’s key to know these special needs to give the best care.
In kids, third-degree AV block can be born with them or happen later. Congenital third-degree AV block might link to mom’s autoimmune issues. Acquired cases could come from heart surgery or myocarditis. For kids, the goal is to keep their heart rate up and watch for heart failure signs.
Pregnant women with third-degree AV block need close watch. Monitoring is key to avoid heart failure and ensure a safe birth.
Older adults often have other health problems that make third-degree AV block harder to manage. Pacemaker implantation is common. But, other health issues can change how well it works and need careful thought.
Athletes with third-degree AV block face a special challenge. It can affect their sports career. Guidelines suggest a detailed check and risk assessment to see if they can keep playing sports safely.
Handling third-degree AV block in various groups needs a custom plan. It’s important to understand each group’s unique needs. This way, doctors can give more effective and tailored care.
Managing third-degree AV block starts with quick diagnosis and treatment. With the right care, like pacemaker implants, patients see big improvements in their life quality.
At Liv Hospital, we focus on full care for third-degree AV block patients. We do more than just pacemaker implants. We also keep a close eye on patients and offer ongoing support for the best results.
Thanks to new medical tech and treatment plans, the outlook for third-degree AV block patients is much better. Knowing about the condition and how to manage it helps patients live full and active lives.
Long-term care means regular check-ups and monitoring. Our team is dedicated to giving each patient the care they need. We tailor our care to meet each patient’s unique needs.
Third-degree AV block, also known as complete AV block, is a serious heart condition. It happens when there’s no connection between the heart’s electrical signals from the atria and the ventricles.
To diagnose third-degree AV block, look for seven key ECG signs. These include complete AV dissociation and regular P waves. You’ll also see independent QRS complexes and no link between P waves and QRS complexes.
Other signs include junctional and ventricular escape rhythms. Also, look for specific patterns on rhythm strips.
Junctional escape rhythm has a heart rate of 35-50 bpm and narrow QRS complexes. Ventricular escape rhythm has a heart rate of 20-40 bpm and wide QRS complexes.
The best treatment for third-degree AV block is getting a pacemaker. This can greatly improve a patient’s health. Emergency steps include stabilizing the patient and starting temporary pacing.Medication management and monitoring are also key.
Third-degree AV block can lead to bradycardia and symptoms like fatigue and dizziness. It also increases the risk of sudden cardiac death. Stokes-Adams attacks can happen too.
Yes, different groups need special care. This includes children, pregnant women, the elderly, and athletes. Knowing these needs is vital for the best care.
Yes, with quick diagnosis and effective treatment, like pacemaker implantation, patients can live active lives.
ECG is key in diagnosing third-degree AV block. It shows the important signs, like complete AV dissociation and regular P waves. It also shows independent QRS complexes.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!