Recovering from surgery is more than just resting. The “5 P’s after surgery” offer a detailed plan for better recovery. This plan covers key areas to help with healing and avoid problems.
The NHS says a top-notch care plan starts with the “5 P assessment”. It includes Pain management, Position, Personal Hygiene, Periphery, and Pump. This ensures full care for patients. For more on neurovascular observations,
Key Takeaways
- The “5 P’s after surgery” framework optimizes post-operative recovery.
- The 5 P’s include Pain management, Position, Personal Hygiene, Periphery, and Pump.
- Implementing the 5 P’s enhances patient care and reduces complications.
- A complete approach to post-operative care leads to better results.
- The NHS highlights the “5 Ps” as key to quality care.
The 5 P’s Framework: A Holistic Approach to Post-Surgical Recovery

The 5 P’s framework is changing how we care for patients after surgery. It covers all important parts of recovery, making sure patients get the best care.
The 5 P’s P assessment helps evaluate a patient’s physical condition, guiding accurate diagnosis and treatment planning for better medical outcomes and patient care. – Pain, Position, Personal Hygiene, Periphery, and Pump – work together to help patients. They make sure patients get the care they need, improving their recovery.
Evidence-Based Benefits of Structured Post-Operative Care
Studies support the 5 P’s framework for post-surgery care. They show it can lower complications and improve results. The main benefits are:
- Reduced risk of post-operative complications
- Lower readmission rates
- Improved patient satisfaction
How the 5 P’s Reduce Complications and Readmission Rates
The 5 P’s framework tackles important post-surgery care areas. For instance, managing pain and checking neurovascular health early can spot issues. The 6 Ps of compartment syndrome are also key for checking neurovascular status.
Using the 5 P’s, doctors can cut readmission rates by up to 15% and boost patient happiness. This all-encompassing approach to recovery is key to top-notch patient care.
Pain: Effective Management for Enhanced Mobility and Comfort

Managing pain well is key to a smooth recovery after surgery. It helps patients move better and feel more comfortable. Adequate pain control is vital for quick recovery, less risk of problems, and better results.
Standardized Assessment Tools for Post-Surgical Pain
Using standardized assessment tools is important for checking post-surgical pain. Tools like the Numeric Rating Scale (NRS) and the Faces Pain Scale (FPS) help doctors measure pain. This way, they can adjust pain treatments for better results.
Multimodal Analgesia Approaches
A multimodal analgesia approach mixes different ways to manage pain. It might include opioids, other pain medicines, and local anesthesia. This method offers better pain relief and cuts down on opioid side effects.
Connection Between Pain Control and Early Mobilization
Good pain control is linked to early movement after surgery. When pain is managed, patients can start moving sooner. This early activity helps avoid problems and speeds up healing.
Position: Strategic Positioning to Prevent Complications
Getting patients in the right position after surgery is key. It can greatly affect how well they recover. Healthcare teams must focus on the best positions to avoid problems. This includes preventing pressure injuries and breathing issues.
Optimal Positioning Schedules for Different Surgical Procedures
Every surgery needs its own positioning plan to lower risks. For instance, those who have had spinal surgery should avoid putting pressure on their spine. Healthcare teams should create specific plans for each patient based on their surgery.
Changing positions often can stop bed sores and improve blood flow. How often to move someone depends on their health and the type of surgery.
Preventing Pressure Injuries and Respiratory Complications
Improper positioning can lead to bed sores and breathing problems. Regularly changing positions can prevent bed sores by avoiding too much pressure. Also, keeping the head of the bed up can help breathing and lower respiratory risks.
By focusing on the right positions, healthcare teams can make patients’ recoveries better and safer.
Personal Hygiene: Critical Protocols for Infection Prevention
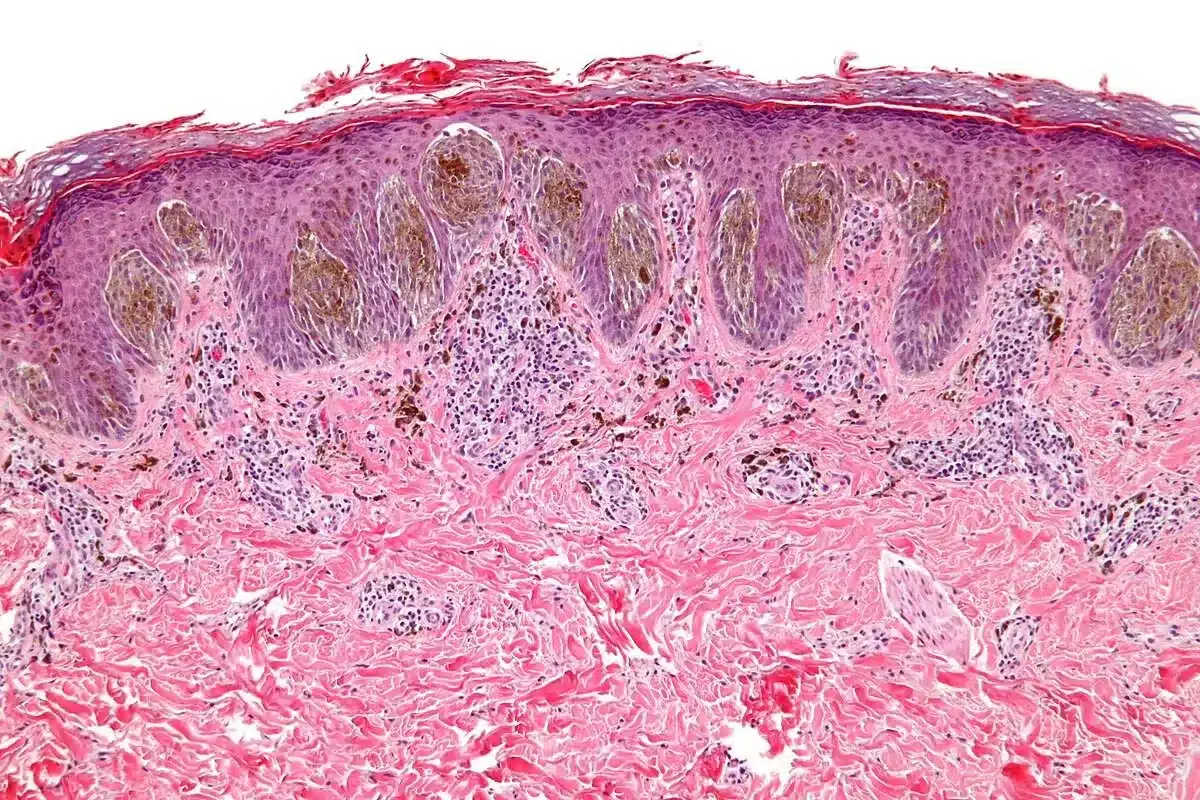
Personal hygiene is key in post-operative care, cutting down infection risks. Good hygiene practices are vital to stop surgical site infections (SSIs) and help patients recover well.
It’s important to follow strict hygiene rules in post-surgery care. Healthcare workers must stick to these rules to lower infection chances.
Surgical Site Care Guidelines and Best Practices
Proper care of the surgical site is a big part of post-operative care. Guidelines suggest:
- Keeping the surgical site clean and dry
- Using sterile dressings and changing them as needed
- Watching for signs of infection, like redness, swelling, or discharge
Understanding the 5% Global Surgical Site Infection Rate
About 5% of surgeries worldwide result in surgical site infections. This shows we need to keep working on stopping infections. Knowing what causes SSIs helps us make better prevention plans.
Patient Education for Post-Discharge Hygiene Maintenance
Teaching patients about hygiene after they leave the hospital is very important. They should learn:
- How to shower or bathe to keep the surgical site clean
- How to wash hands properly
- What signs of infection mean they need to see a doctor
By focusing on personal hygiene and teaching patients, healthcare workers can lower the chance of infections after surgery. This helps patients get better faster.
Periphery: Complete P Check of Neurovascular Status
Checking the periphery is key to spotting neurovascular issues after surgery. It looks at the limb’s neurovascular health to avoid problems like compartment syndrome and blood clots.
Checking the limb’s neurovascular status is vital for good recovery after surgery. It helps find signs of compartment syndrome, a serious condition where pressure builds up in a body space, harming muscles and nerves.
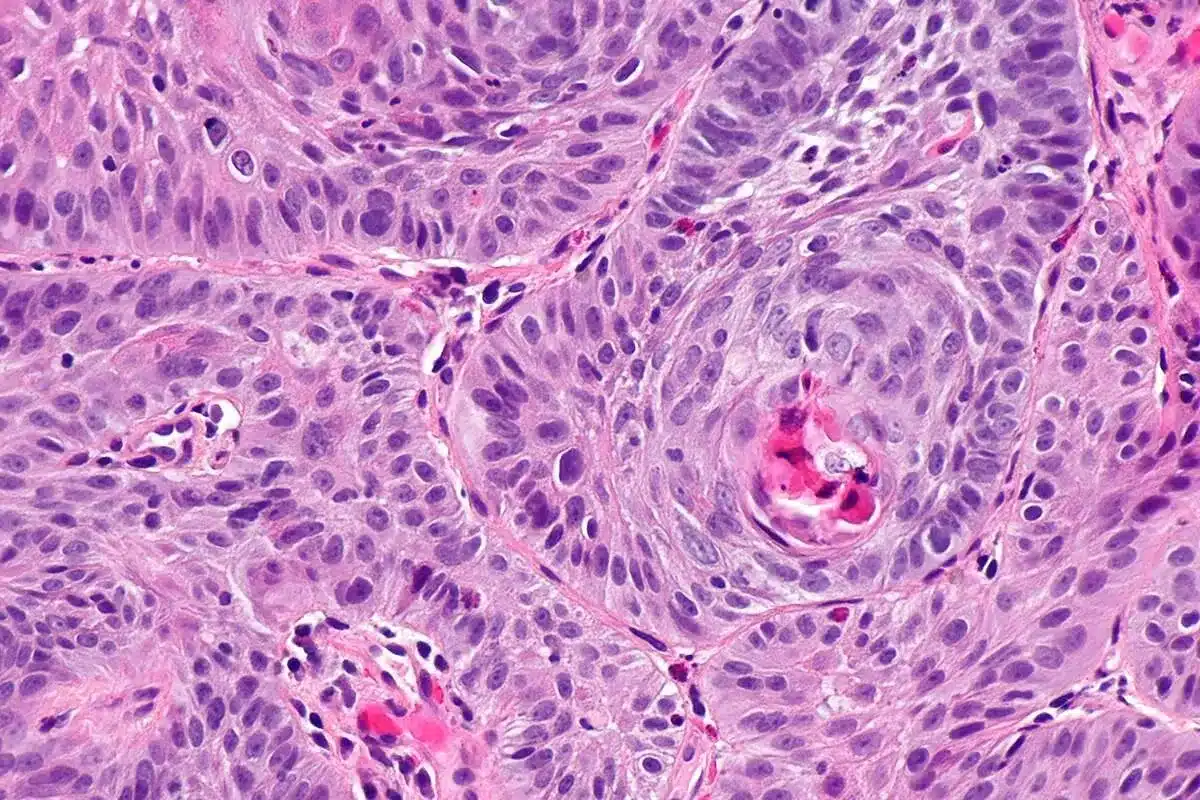
The 6 P’s of Compartment Syndrome Assessment
Checking for compartment syndrome uses the 6 P’s: pain, pulselessness, pallor, poikilothermia (cold to the touch), paresthesia, and paralysis. Pain is often the first sign, and it doesn’t match the situation. Doctors must watch for these signs to act quickly.
Preventing Venous Thromboembolism in Post-Surgical Patients
Venous thromboembolism (VTE) is a big risk for patients after surgery, happening in 1“2% of general surgery patients. Preventive steps include moving early, wearing compression stockings, and using blood thinners. Keeping the limb moving and blood flowing helps prevent blood clots, showing why checking the periphery is so important.
Frequency and Documentation of Neurovascular Checks
Regular checks of the neurovascular system are key to catching problems early. How often these checks happen depends on the surgery and the patient’s risk. Keeping accurate records of these checks is vital for the best care and clear communication among healthcare teams.
Pump: Managing Medical Devices for Optimal Function
The “Pump” part of post-surgical care is about managing medical devices correctly. It’s key to avoid problems and help with healing.
Types and Purposes of Post-Surgical Drainage Systems
Drainage systems are vital after surgery to remove fluids or gas. They come in types like closed, open, and sump systems. Knowing the type and purpose helps healthcare teams manage them well.
Good management of these systems cuts down infection risks and helps healing.
Preventing Device-Associated Infections and Complications
Infections linked to devices are a big worry after surgery. To stop these, healthcare teams must clean and change dressings often. They also need to watch for infection signs like redness or swelling.
“The prevention of device-associated infections requires a multifaceted approach that includes proper device management, surveillance, and education.”
CDC Guidelines
Troubleshooting Common Device Issues
Even with good care, devices can fail or get blocked. It’s important to fix problems like kinked or blocked tubes fast. Healthcare teams should know how to solve these issues quickly.
- Check for kinking or twisting of the device
- Verify the device is properly connected
- Monitor for signs of device malfunction
Understanding drainage systems, preventing infections, and fixing device problems helps. This ensures medical devices work properly and aids in a smooth recovery after surgery.
Conclusion: Implementing the 5 P’s to Improve Patient Outcomes
Using the 5 P’s framework is key to giving top-notch care and better patient results. It helps healthcare teams by focusing on Pain, Position, Personal Hygiene, Periphery, and Pump. This approach cuts down on complications and helps patients heal faster.
The 5 P’s offer a full plan for after-surgery care. Studies show that following these steps can lower hospital readmission rates and make patients happier. By using the 5 P’s, healthcare teams can keep up with the latest research and care standards. This leads to better care and results for patients.
Experts stress the need for organized care after surgery. The 5 P’s are a great way to make this happen. By adding the 5 P’s to their work, healthcare teams can greatly improve patient care and outcomes. This is a big step towards providing the best care possible.
FAQ
What are the 5 P’s after surgery?
The 5 P’s after surgery are a key framework for care. They focus on Pain, Position, Personal Hygiene, Periphery, and Pump.
How do the 5 P’s improve patient outcomes?
The 5 P’s help lower the risk of complications and readmission rates. They also boost patient satisfaction.
What is the significance of pain management after surgery?
Managing pain well is key to comfort and mobility after surgery. It also reduces complications and aids in recovery.
How can healthcare providers prevent compartment syndrome?
Healthcare providers can prevent compartment syndrome by checking for Pain, Pallor, Pulselessness, Paresthesia, Paralysis, and Poikilothermia. This helps identify and prevent complications.
What is the role of personal hygiene in post-operative care?
Personal hygiene is vital to prevent infections after surgery. Healthcare providers must follow guidelines and best practices to reduce infection risk.
How often should neurovascular checks be performed after surgery?
The frequency of neurovascular checks depends on the surgery and the patient’s condition. Regular checks and documentation are key to optimal care.
What are the different types of post-surgical drainage systems?
Post-surgical drainage systems include closed, open, and sump systems. Each serves a specific purpose and function.
How can healthcare providers prevent device-associated infections?
Healthcare providers can prevent infections by using sterile equipment and monitoring devices. Proper insertion and maintenance are also important.
What is the connection between pain control and early mobilization?
Effective pain control is essential for early mobilization. This reduces complications, improves circulation, and aids in recovery.
How can healthcare providers optimize positioning schedules for different surgical procedures?
Healthcare providers can tailor positioning schedules based on patient and surgical needs. This prevents pressure injuries and respiratory complications.
References
- Centers for Disease Control and Prevention. (2017). Guidelines for the Prevention of Surgical Site Infection. https://www.cdc.gov/hai/ssi/index.html
- Medical News Today. (2020). What Is a Surgical Procedure?. https://www.medicalnewstoday.com/articles/316706
- World Health Organization. (2018). Surgical Site Infection Prevention: Evidence-Based Guidelines. World Health Organization.