Last Updated on November 27, 2025 by Bilal Hasdemir
Did you know that nearly 600,000 women in the United States undergo hysterectomy every year? This surgery removes the uterus and is a common treatment for several gynecological issues. Understanding the 5 types of hysterectomy is key to making the right decision about your health.
Choosing the right procedure can feel overwhelming, but knowing the 5 types of hysterectomy helps you make an informed choice. We’re here to guide you through each type, offering support at every step to ensure you receive the best care possible.
Key Takeaways
- Understanding the different approaches to hysterectomy is vital for patient care.
- There are multiple factors to consider when choosing a hysterectomy procedure.
- Our team is committed to providing personalized support for international patients.
- Hysterectomy is a common treatment for various gynecological conditions.
- Patients should be aware of the various options available to them.
Understanding Hysterectomy: A Brief Overview

Hysterectomy is a common surgery in the U.S. It involves removing the uterus. This surgery is used to treat many gynecological issues that other treatments can’t fix.
Definition and Basic Concepts
A hysterectomy removes a woman’s uterus. It’s done for many reasons, like uterine fibroids or endometriosis. Doctors usually try other treatments first before suggesting a hysterectomy.
The type of hysterectomy depends on the surgery’s extent and approach. Knowing these details helps patients make better choices about their health.
Statistics and Prevalence in the United States
In the U.S., hysterectomies are among the most common surgeries. The CDC reports hundreds of thousands each year. Most women have this surgery between 40 and 50 years old.
The number of hysterectomies varies by region and population. This is due to different gynecological conditions, healthcare access, and patient choices.
The 5 Types of Hysterectomy: Comparing Your Options
When you think about a hysterectomy, knowing the different types is key. A hysterectomy is a big surgery that removes the uterus, and sometimes other parts too. The type of surgery you choose can affect how you recover and how you feel afterward.
Total Hysterectomy
A total hysterectomy takes out the whole uterus, including the cervix. It’s the most common type. Doctors often do it for things like uterine fibroids, endometriosis, and heavy bleeding.
Key aspects of total hysterectomy include:
- Removal of the uterus and cervix
- Often recommended for conditions like fibroids and endometriosis
- Can be performed abdominally, vaginally, or laparoscopically
Partial (Subtotal/Supracervical) Hysterectomy
In a partial hysterectomy, only the top part of the uterus is taken out. The cervix stays. This is less common but might be an option for some.
Benefits and considerations:
- Less invasive in terms of cervical removal
- May have a shorter recovery time
- Not suitable for all conditions, such as cervical dysplasia
Radical Hysterectomy
A radical hysterectomy is a bigger surgery. It removes the uterus, cervix, part of the vagina, and sometimes lymph nodes in the pelvis. It’s usually for cancer.
Key features:
- Removal of the uterus, cervix, and surrounding tissues
- Often performed in cases of cervical or uterine cancer
- May involve lymph node dissection
Hysterectomy with Bilateral Salpingo-Oophorectomy
This surgery takes out the uterus, both ovaries, and fallopian tubes. It’s a big surgery that can affect hormone levels and health.
Considerations:
- Impacts hormone production, potentially leading to early menopause
- May be recommended for certain conditions like ovarian cancer or severe endometriosis
- Requires careful consideration regarding hormone replacement therapy
Each type of hysterectomy has its own reasons, benefits, and downsides. Knowing these differences helps patients make better choices for their health.
Abdominal Hysterectomy: The Traditional Approach
The abdominal hysterectomy is a common surgery to remove the uterus through the belly. It has been used for many years. It’s often chosen for different gynecological issues.
Procedure Details and Surgical Technique
During this surgery, a cut is made in the belly to reach the uterus. The steps can change based on the patient and the doctor. Generally, the process includes:
- Making an incision in the abdomen, either vertically or horizontally, depending on the specific case.
- Carefully dissecting the surrounding tissues to access the uterus.
- Removing the uterus, and sometimes other reproductive organs, based on the patient’s needs.
- Closing the incision with sutures or staples.
Recovery Timeline and Hospital Stay
Recovery from this surgery usually means a few days in the hospital. It can take 6-8 weeks to get back to normal. Recovery depends on:
- The patient’s overall health and age.
- The presence of any complications during or after surgery.
- The effectiveness of pain management strategies.
Specific Advantages of Abdominal Approach
The abdominal hysterectomy has several benefits:
- Direct Access: The surgeon can easily reach the uterus and nearby organs, making complex cases easier.
- Flexibility: This method allows for quick adjustments if unexpected issues come up during surgery.
- Effectiveness for Complex Conditions: It’s often the best choice for treating serious gynecological problems, like big fibroids or endometriosis.
Potential Disadvantages and Limitations
Despite its benefits, there are downsides to abdominal hysterectomy:
- Longer Recovery Time: It usually takes longer to recover than less invasive surgeries.
- More Visible Scarring: The belly incision can leave a more noticeable scar.
- Higher Risk of Complications: Like any big surgery, there’s a chance of problems, such as infection or adhesions.
In summary, abdominal hysterectomy is a key surgery for many women. It’s a tried and true method for treating various gynecological issues. Knowing its details, benefits, and possible drawbacks helps patients make better choices about their health.
Vaginal Hysterectomy: A Less Invasive Option
Vaginal hysterectomy is a surgery that removes the uterus through the vagina. It’s less invasive and has become popular. Women with certain gynecological conditions might choose this option. It can lead to a quicker recovery than other methods.
Procedure Details and Surgical Technique
The vaginal hysterectomy procedure starts with an incision in the vagina. This way, no abdominal cut is needed. This can reduce pain and scarring after surgery.
Key steps in the procedure include:
- Preparation for surgery, which may include cleaning and sterilizing the vaginal area.
- Administration of appropriate anesthesia to ensure patient comfort.
- Making a careful incision in the vagina to access the uterus.
- Dissection and removal of the uterus, taking care to ligate blood vessels and other supporting structures.
- Closure of the vaginal incision, typically with dissolvable sutures.
Recovery Timeline and Hospital Stay
Vaginal hysterectomy often means a shorter recovery time. Women usually spend less time in the hospital, sometimes just a day or two.
The recovery process typically involves:
- Immediate post-operative care in the hospital, focusing on pain management and monitoring for any complications.
- A period of rest at home, avoiding heavy lifting, bending, or strenuous activities.
- Follow-up appointments with the healthcare provider to monitor healing and remove any non-dissolvable sutures.
Specific Advantages of Vaginal Approach
The vaginal approach to hysterectomy has many benefits. These include:
- Less post-operative pain due to the absence of an abdominal incision.
- Shorter hospital stays and quicker return to normal activities.
- Reduced risk of infection and other complications associated with abdominal surgery.
- No visible scar, as the incision is made inside the vagina.
One patient said, “I was back to my normal routine within a few weeks, and the lack of a visible scar was a big plus for me.”
“The vaginal hysterectomy was a game-changer for me. The recovery was faster than I expected, and I appreciated not having a scar.”A patient sharing her experience
Potential Disadvantages and Limitations
While vaginal hysterectomy has many benefits, it’s not for everyone. Some limitations include:
- The need for a certain level of vaginal accessibility and uterine mobility.
- Potential limitations in cases where the uterus is very large or there are significant adhesions.
- The requirement for a skilled surgeon experienced in vaginal hysterectomy techniques.
It’s important for patients to talk to their healthcare provider. They should decide if vaginal hysterectomy is right for them.
Laparoscopic Hysterectomy: Minimally Invasive Technique
The laparoscopic approach to hysterectomy has changed gynecology a lot. It makes scars smaller and helps healing happen faster. This method uses small cuts in the belly to put in a laparoscope and tools for surgery.
Procedure Details and Surgical Technique
Laparoscopic hysterectomy is done under general anesthesia. The surgeon makes small cuts, about 0.5 to 1 cm, for the laparoscope and tools. The laparoscope shows images on a screen, helping the surgeon see inside the body.
The steps include finding and tying the uterine arteries, separating the uterus, and taking it out through the vagina or belly.
Recovery Timeline and Hospital Stay
Laparoscopic hysterectomy has a shorter recovery time than open surgery. Women usually go home in 24 to 48 hours. It takes a few weeks to fully recover, during which they should avoid heavy lifting and hard activities.
Specific Advantages of Laparoscopic Approach
The laparoscopic method has many benefits:
- Smaller cuts mean less scarring
- Less pain after surgery
- Shorter hospital stay
- Quicker return to normal life
- Lower risk of infection than open surgery
Potential Disadvantages and Limitations
Even with its benefits, laparoscopic hysterectomy isn’t right for everyone. Some issues include:
- It needs special training for surgeons
- It might take longer than open surgery
- It can’t reach all parts of the pelvis
- It costs more because of special equipment
Patients should talk to their doctor to see if this surgery is best for them.
Laparoscopic-Assisted Vaginal Hysterectomy (LAVH)
LAVH is a new way to do hysterectomies. It combines laparoscopic and vaginal methods. This mix is becoming popular because it might help patients recover faster.
How LAVH Differs from Standard Approaches
LAVH is different because it uses laparoscopy and vaginal surgery together. This way, surgeons can do complex surgeries with less invasion. It’s less invasive than traditional methods, leading to quicker healing.
The laparoscopic part helps see the pelvic area clearly. This is great for surgeries with adhesions. The vaginal part removes the uterus without a big cut.
Ideal Candidates for LAVH
Choosing LAVH depends on several things. These include the reason for the surgery, the patient’s health, and past surgeries. It’s best for women with fibroids, endometriosis, or bleeding issues.
| Condition | Ideal for LAVH | Considerations |
| Uterine Fibroids | Yes | Size and location may affect feasibility |
| Endometriosis | Yes | Laparoscopic visualization helps in assessing extent |
| Abnormal Uterine Bleeding | Yes | Previous pelvic surgeries may be a factor |
Recovery Expectations and Outcomes
Recovery from LAVH is often easier. Patients might feel less pain and stay in the hospital less. They can get back to normal faster. But, recovery can differ based on health and following doctor’s orders.
Research shows LAVH has fewer complications and less pain than other methods. But, it’s important to follow the doctor’s advice for the best recovery.
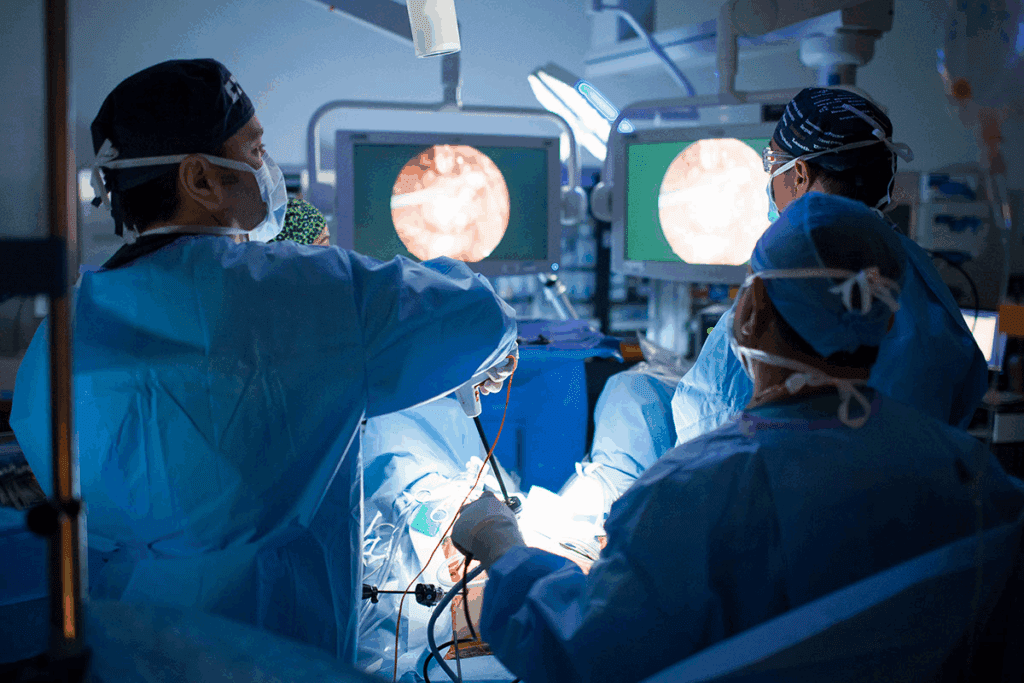
Robotic-Assisted Hysterectomy: Cutting-Edge Technology
Robotic-assisted hysterectomy is a big step forward in surgery. It gives patients a precise and less invasive choice. This method combines the surgeon’s skill with the robotic tools’ flexibility and precision.
How Robotic Surgery Works
Robotic surgery uses a high-tech system. It lets surgeons do complex tasks with better precision and control. The setup includes a console for the surgeon, robotic arms, and a 3D vision system.
The surgeon’s actions are turned into exact movements by the robotic arms. This makes it easier to do delicate work and stitch without harming nearby tissues. It can mean less blood loss, fewer complications, and quicker healing.
Recovery Timeline and Hospital Stay
Recovery from robotic-assisted hysterectomy might be faster than traditional surgery. Many patients go home the same day or within 24 hours. It usually takes a few weeks to fully recover, during which they should avoid heavy lifting and hard activities.
Advantages of Robotic Precision
The robotic system has many benefits, including:
- Enhanced precision and dexterity
- Improved visualization through 3D imaging
- Less tissue trauma and blood loss
- Smaller incisions, resulting in less scarring
- Potential for shorter hospital stays and faster recovery
Cost and Accessibility Considerations
Robotic-assisted hysterectomy has many advantages, but cost and access are important. It’s more expensive than traditional methods because of the advanced tech. Insurance coverage varies, so patients should check with their providers.
| Procedure | Average Cost | Hospital Stay | Recovery Time |
| Robotic-Assisted Hysterectomy | $15,000 – $25,000 | 1-2 days | 2-4 weeks |
| Laparoscopic Hysterectomy | $10,000 – $20,000 | 1-3 days | 2-6 weeks |
| Open Hysterectomy | $8,000 – $18,000 | 3-5 days | 6-8 weeks |
Knowing these details helps patients make better choices about their surgery.
Which Hysterectomy is Considered the “Easiest”?
Patients looking into a hysterectomy want to know which one is the easiest. They look for the one with the least recovery time and few complications. What’s considered “easiest” can change based on the patient’s health, why they need the surgery, and their personal choices.
Defining “Easiest” in Terms of Patient Experience
The “easiest” hysterectomy is one that balances well-being, safety, and comfort during recovery. The length of hospital stay, post-operative pain, and complication risks are key factors.
Comparing Recovery Times Across Procedures
Recovery times differ among hysterectomy types. Minimally invasive procedures like laparoscopic or robotic-assisted ones usually have shorter recovery times. They often let patients get back to normal in 1-2 weeks.
On the other hand, traditional abdominal hysterectomies can take 2-4 days in the hospital and weeks at home to recover.
Pain Management Differences Between Approaches
Pain management is vital in choosing the “easiest” hysterectomy. Robotic-assisted hysterectomies are precise and less invasive, leading to less pain for patients. Abdominal hysterectomies, being more invasive, might need stronger pain management.
Complication Rates and Safety Profiles
The safety of a hysterectomy is key. Minimally invasive procedures tend to have fewer complications than more invasive surgeries. Knowing these risks helps patients and doctors choose the best option.
In summary, while the “easiest” hysterectomy depends on many factors, minimally invasive procedures like laparoscopic and robotic-assisted ones are often seen as better for recovery.
Factors That Determine the Best Hysterectomy Approach for You
Choosing the right hysterectomy procedure is important. It’s not the same for everyone. The decision depends on medical, anatomical, and personal factors.
Medical Conditions and Specific Indications
The reason for needing a hysterectomy matters a lot. For example:
- Fibroids or abnormal uterine bleeding: May need a different method than endometriosis or cancer.
- Uterine prolapse: Often treated with a vaginal hysterectomy.
- Cancer diagnosis: May require a more radical procedure.
Anatomical Considerations and Previous Surgeries
Your body’s shape and past surgeries also matter. They can affect the best way to do the surgery.
- Previous pelvic surgeries: May make some methods harder, so others are better.
- Anatomical abnormalities: Can make some surgeries not work well.
Surgeon Experience and Specialization
The surgeon’s skills and focus are key to a good outcome.
- Surgeon experience with different techniques: More skilled surgeons can offer more options.
- Specialization in gynecologic surgery: Means the surgeon stays current with the latest methods.
Hospital Resources and Available Technology
The hospital’s resources and technology also play a part. They can affect the choice of surgery.
- Availability of advanced surgical equipment: Like robotic systems, can lead to more precise and less invasive surgeries.
- Post-operative care facilities: Can impact how well you recover.
Healthcare providers can choose the best hysterectomy for each patient. This makes the surgery more effective and recovery better.
Common Indications for Hysterectomy
Many health issues can make a woman think about getting a hysterectomy. This surgery removes the uterus. It’s a big decision, usually made when other treatments don’t work or aren’t right.
Fibroids and Abnormal Bleeding
Fibroids are non-cancerous growths in the uterus. They can cause heavy bleeding, long periods, and pain. Large or many fibroids can really affect a woman’s life, making her think about a hysterectomy.
Endometriosis and Chronic Pelvic Pain
Endometriosis is a painful disorder where uterine tissue grows outside the uterus. It can cause a lot of pain, heavy or irregular bleeding, and trouble getting pregnant. Sometimes, a hysterectomy is considered for endometriosis when other treatments don’t work.
Endometriosis can really hurt and make life hard. A hysterectomy can help women with severe endometriosis by easing pain and other symptoms.
Adenomyosis and Uterine Enlargement
Adenomyosis is when uterine lining grows into the muscular walls. It can lead to heavy bleeding, painful periods, and a big uterus. In some cases, a hysterectomy might be considered if other treatments don’t help.
Uterine Prolapse and Pelvic Floor Disorders
Uterine prolapse is when the uterus falls into the vagina. It’s often linked to pelvic floor disorders, causing symptoms like incontinence and pressure. A hysterectomy might be an option for severe uterine prolapse.
The American College of Obstetricians and Gynecologists says, “Hysterectomy is a common treatment for uterine prolapse, when other treatments fail.” This shows how important a hysterectomy can be for women with uterine prolapse and related issues.
Alternatives to Consider Before Hysterectomy
Exploring alternatives to hysterectomy can guide patients in making informed choices. Hysterectomy is a big surgery that changes many women’s lives. Yet, it’s not the only fix for gynecological issues.
Medication Options for Various Conditions
For conditions like fibroids, endometriosis, and adenomyosis, meds can be a good choice. Hormonal treatments, like birth control pills and GnRH agonists, can ease symptoms like heavy bleeding and pain.
NSAIDs can also help with pain from these conditions. In some cases, meds can even shrink fibroids or cut down on bleeding, possibly avoiding surgery.
Minimally Invasive Alternatives
There are many non-surgical options for gynecological problems. For instance, uterine artery embolization can shrink fibroids by cutting off their blood supply. Endometrial ablation can also reduce or stop heavy menstrual bleeding.
Women with endometriosis might benefit from laparoscopic surgery. This can remove endometrial lesions, easing pain and symptoms.
Watchful Waiting Approach
For mild symptoms or non-life-threatening conditions, watchful waiting might be the best choice. Regular check-ups with a healthcare provider can track the condition’s progress. This helps decide if symptoms get worse or stay the same.
When Alternatives Are Not Sufficient
Not all alternatives work for everyone. If other treatments fail or the condition is severe, a hysterectomy might be considered. The patient’s health, symptom severity, and future fertility plans are key factors in this decision.
It’s vital for patients to talk to their healthcare provider about all options. This helps find the best treatment for their specific situation.
Preparing for Your Hysterectomy: What to Expect
Getting ready for a hysterectomy can feel less scary if you know what’s coming. Understanding the different parts of the process can make you feel less anxious. It also helps you recover better.
Pre-Surgery Consultations and Evaluations
You’ll have many talks and tests before your surgery. These are key to checking your health and picking the best surgery plan. Your doctor will look over your health history, talk about why you need the surgery, and explain how it will be done.
Key parts of these talks include:
- Going over your health history
- Talking about the surgery and its possible risks
- Doing tests like blood work and imaging
- Checking any medicines you’re taking
Required Tests and Preparations
There are many tests and steps to get you ready for surgery. These might include:
- Blood tests to check your blood and body chemistry
- Imaging tests like ultrasound or MRI to see your uterus
- An ECG if you’re older or have heart issues
- Guidance on managing your medicines before surgery
It’s very important to follow your doctor’s advice closely. This helps lower risks and makes surgery more likely to succeed.
Mental and Emotional Preparation Strategies
Getting ready for a hysterectomy is not just about your body. Your mind and feelings are also key. Ways to help include:
- Getting support from loved ones or a support group
- Trying relaxation methods like deep breathing or meditation
- Learning as much as you can about your surgery and recovery
- Being realistic about how long it will take to get better
Setting Up Your Home for Recovery
Having a cozy recovery spot at home can really help your healing. Here are some tips:
- Make a recovery area with everything you need close by
- Get help with chores and errands
- Buy supplies like comfy clothes and heating pads
- Plan fun things to do while you’re recovering
By doing these things, you can make your recovery easier. It makes the whole experience less stressful and more manageable.
Recovery After Hysterectomy: Timeline and Tips
Recovering from a hysterectomy is different for everyone. It depends on your health, the surgery type, and care after surgery. Knowing what to expect helps manage your recovery and make smart choices about your care.
Immediate Post-Operative Period (First 72 Hours)
The first 72 hours are key for getting better. You might feel pain, tiredness, and discomfort. It’s vital to manage your pain well. Your doctor will give you medicine for this.
Also, watch for any signs of trouble like too much bleeding, fever, or trouble peeing.
- Rest and avoid strenuous activities
- Follow the prescribed pain management regimen
- Monitor for signs of complications
First Few Weeks of Recovery
In the first few weeks, you’ll start to feel stronger. Try to avoid heavy lifting, bending, or hard exercise. You can start with light activities in a few weeks, but it may take longer to fully recover.
Tips for a Smooth Recovery:
- Follow post-operative instructions carefully
- Attend follow-up appointments
- Maintain a healthy diet to support healing
Return to Normal Activities Timeline
When you can go back to normal activities depends on your surgery and health. Usually, it takes 6-8 weeks.
Listen to your body and don’t rush the recovery.
Physical Therapy and Rehabilitation Options
Physical therapy is very helpful, even more so if you have pelvic floor issues. A physical therapist can help with exercises to boost strength and flexibility.
By understanding your recovery and following these tips, you can better manage your journey. Stay informed, follow your doctor’s advice, and take care of yourself during this time.
Life After Hysterectomy: Long-Term Considerations
Many women wonder about their health after a hysterectomy. This surgery can change their life in many ways. Hormonal changes and emotional adjustments are common long-term effects.
Hormonal Changes and Management
One big change is hormonal. If the ovaries are removed, women may go into menopause right away. This can cause hot flashes, mood swings, and vaginal dryness.
Management strategies for these changes include:
- Hormone Replacement Therapy (HRT) to ease menopausal symptoms
- Lifestyle changes, like diet and exercise, to manage symptoms and stay healthy
- Alternative therapies, such as acupuncture and herbal supplements, to help with menopause symptoms
Sexual Function and Intimacy
Sexual health is important after a hysterectomy. Hormonal changes can lower libido, but some women find their sex life improves. This is because they no longer have pain or heavy bleeding.
Key considerations for sexual health include:
- Talking openly with your partner about any changes or concerns
- Using lubricants to address vaginal dryness
- Exploring different types of intimacy and sexual activity
Emotional and Psychological Adjustments
Emotional and psychological adjustments are big after a hysterectomy. Women may feel a sense of loss or grief. This is because they’ve lost their uterus and can no longer have children.
Support strategies for these adjustments include:
- Counseling or therapy to address emotional concerns
- Support groups to connect with other women who have had a hysterectomy
- Self-care practices, like meditation and journaling, to improve emotional well-being
Long-Term Health Monitoring Needs
Women need to monitor their health long-term after a hysterectomy. Regular check-ups with their healthcare provider are important. This helps catch any long-term complications early.
Important aspects of long-term health monitoring include:
- Regular pelvic exams and Pap smears (if the cervix is present)
- Monitoring for signs of osteoporosis, if ovaries were removed
- Maintaining a healthy lifestyle, including a balanced diet and regular exercise
Cost Considerations for Different Hysterectomy Procedures
When thinking about a hysterectomy, it’s key to look at the costs and insurance. The price can change a lot based on the type of surgery, the doctor’s fees, hospital costs, and your insurance.
Insurance Coverage in the United States
In the U.S., most health plans cover hysterectomies when they’re needed. But, how much they cover can differ a lot. It’s important to check your insurance before the surgery.
Usually, insurance pays for a big part of the surgery costs. This includes the doctor’s fee, hospital stay, and follow-up care. But, you might have to pay some money yourself, like deductibles, copays, and coinsurance.
Out-of-Pocket Expenses to Anticipate
Here are some costs you might face for a hysterectomy:
- Deductibles: The amount you pay before insurance starts.
- Copays: Fixed costs for each doctor visit or service.
- Coinsurance: A share of the total cost you pay.
- Prescription medication costs: Costs for pain meds and other meds after surgery.
Cost Comparison Between Procedure Types
The cost of a hysterectomy can change a lot based on the type. Here’s a quick look:
| Procedure Type | Average Cost Range |
| Abdominal Hysterectomy | $15,000 – $30,000 |
| Vaginal Hysterectomy | $10,000 – $25,000 |
| Laparoscopic Hysterectomy | $12,000 – $28,000 |
| Robotic-Assisted Hysterectomy | $15,000 – $35,000 |
Financial Assistance Programs and Options
If you’re worried about money, there are help programs. Some hospitals and doctors offer financial aid or lower fees based on income. Also, non-profit groups might give grants or help with medical bills.
It’s a good idea to ask about these options when talking with your doctor.
Conclusion: Making an Informed Decision About Your Hysterectomy
As we wrap up our look at hysterectomy options, it’s clear that making a smart choice is key. We’ve talked about the different types of hysterectomies, like total, partial, radical, and laparoscopic. Each has its own benefits and things to think about.
When you’re thinking about a hysterectomy, it’s important to weigh your options carefully. Consider your medical needs, your doctor’s expertise, and the resources you have. Knowing the details of each procedure helps you choose what’s best for you.
At our institution, we’re dedicated to helping international patients. We want to make sure you get top-notch care and support. We urge you to talk to your doctor to find the right path for you. This way, you can make a choice that fits your health and personal needs.
FAQ
What is a hysterectomy?
A hysterectomy is a major surgery to remove the uterus. It’s usually considered when other treatments fail.
What are the different types of hysterectomy?
There are several types. These include total, partial, radical, and hysterectomy with removal of ovaries and fallopian tubes.
What is the difference between a total and partial hysterectomy?
A total hysterectomy removes the whole uterus and cervix. A partial one removes the top part of the uterus, leaving the cervix.
How is a laparoscopic hysterectomy performed?
This surgery uses small incisions and a laparoscope. The uterus is removed through these small openings.
What is the recovery time for a vaginal hysterectomy?
Recovery time is usually 6 to 8 weeks. It can vary based on the surgery and individual factors.
What are the advantages of a robotic-assisted hysterectomy?
It offers precision, smaller cuts, less blood loss, and quicker recovery. This is compared to traditional surgery.
When is a hysterectomy necessary?
It’s needed for severe fibroids, endometriosis, adenomyosis, uterine prolapse, and some cancers.
Are there alternatives to hysterectomy?
Yes, options include medication, minimally invasive procedures, and watchful waiting. It depends on the condition and its severity.
How much does a hysterectomy cost without insurance?
Costs without insurance vary. They depend on the procedure, location, and hospital fees. Prices range from thousands to tens of thousands of dollars.
What are the signs of needing a hysterectomy?
Signs include severe menstrual bleeding, chronic pelvic pain, large fibroids, uterine prolapse, and some cancers.
What is the average age for a hysterectomy?
It’s most common in women aged 40 to 50.
How invasive is a hysterectomy?
Its invasiveness varies. Options range from minimally invasive to more invasive surgeries.
What is the success rate of hysterectomy?
Success rates are high. Most women see relief from symptoms like pain and heavy bleeding.
Reference:
NCBI – Hysterectomy—A Comparison of Approaches (2010)