Knowing about a 6BA embryo is key for those looking into advanced fertility treatments. A 6BA embryo is fully hatched with high-quality inner cell mass and trophectoderm. This makes it a strong candidate for successful implantation.
The quality of embryos greatly affects pregnancy success and live birth rates. Studies show that high-quality embryos, like the 6BA, have a live birth rate of about 46.8%. They also have a success rate of around 60%. The Gardner blastocyst grading system checks embryos on expansion, inner cell mass, and trophectoderm quality.
Grasping the importance of a 6BA embryo helps us make better treatment choices. This can lead to better fertility results.
Key Takeaways
- The 6BA embryo is a fully hatched blastocyst with good inner cell mass and trophectoderm quality.
- The Gardner blastocyst grading system evaluates embryos based on expansion, inner cell mass, and trophectoderm quality.
- Good-quality embryos have a live birth rate of approximately 46.8% and a success rate around 60%.
- Understanding embryo grading is essential for making informed fertility treatment decisions.
- The quality of embryos transferred directly impacts pregnancy outcomes and live birth rates.
The Basics of Embryo Grading in Fertility Treatment

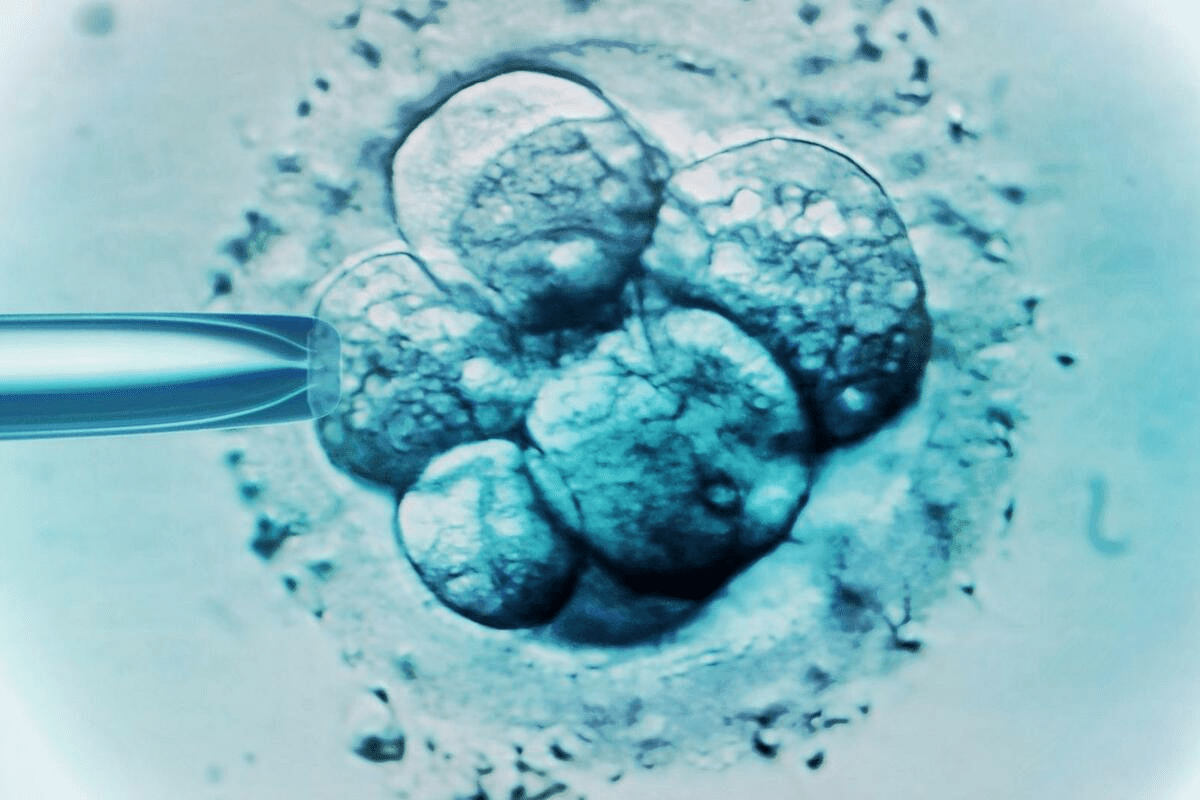
Embryo grading is key in fertility treatments. It helps experts pick the best embryo for IVF. This choice can greatly affect treatment success.
“Embryo grading is not an exact science, but it provides valuable insights into the viability of embryos,” says Medical Expert, a renowned fertility specialist. “By evaluating the morphology of embryos, we can identify those with the highest potentials for implantation and successful pregnancy.”
Why Embryologists Grade Embryos
Embryologists grade embryos to check their viability and implantation chances. They look at expansion, inner cell mass, and trophectoderm quality. This helps pick the best embryos for transfer.
Grading is key for making smart decisions on which embryos to transfer, freeze, or discard. It lets us see an embryo’s implantation and pregnancy success chances.
How Grading Influences Treatment Decisions
Grading affects IVF clinic decisions a lot. It helps choose the best embryo for transfer. This can greatly improve pregnancy chances.
Grading also guides how many embryos to transfer. Sometimes, one high-quality embryo is best. Other times, more might be needed.
Common Grading Systems Used in IVF Clinics
IVF clinics use different grading systems. But most look at similar things. The Gardner blastocyst grading system is very common. It checks expansion, inner cell mass, and trophectoderm quality.
Other systems might be used too, based on the clinic and patient needs. But the main goal is always the same: find the best embryos for transfer to increase pregnancy chances.
The Gardner Blastocyst Grading System Explained

The Gardner blastocyst grading system is key in IVF treatment. It offers a way to check embryo quality in a standard way. It looks at three main things: how much the embryo has grown, the quality of the inner cell mass, and the quality of the outer layer.
Expansion Grades: Understanding the 1-6 Scale
The expansion grade is a score from 1 to 6. It shows how much the embryo has grown. A score of 1 means the embryo is just starting to grow, while 6 means it’s almost ready to hatch.
Expansion grades are key because they show how far along the embryo is. A higher score means the embryo is more developed. This is often linked to a better chance of success.
Inner Cell Mass Quality: A, B, and C Ratings
The inner cell mass (ICM) is a group of cells in the embryo that will become the fetus. The ICM is rated A, B, or C. An A rating means the cells are tightly packed and many. A C rating means the cells are spread out and fewer.
The ICM quality is very important for the embryo’s chance to implant and grow. A high ICM rating (A) is linked to better chances of pregnancy.
Trophectoderm Quality: A, B, and C Ratings
The trophectoderm is the outer layer of the embryo. It will become the placenta and other tissues. Like the ICM, it’s rated A, B, or C based on how well it’s formed. A high-quality trophectoderm is vital for implantation and growth.
A well-formed trophectoderm is essential for the embryo to implant and grow well. The trophectoderm rating gives important clues about the embryo’s implantation chances.
What Is a 6BA Embryo? Complete Breakdown
Understanding a 6BA embryo is key for those going through fertility treatments. It’s graded using the Gardner system. This system checks the embryo’s quality and if it can implant well.
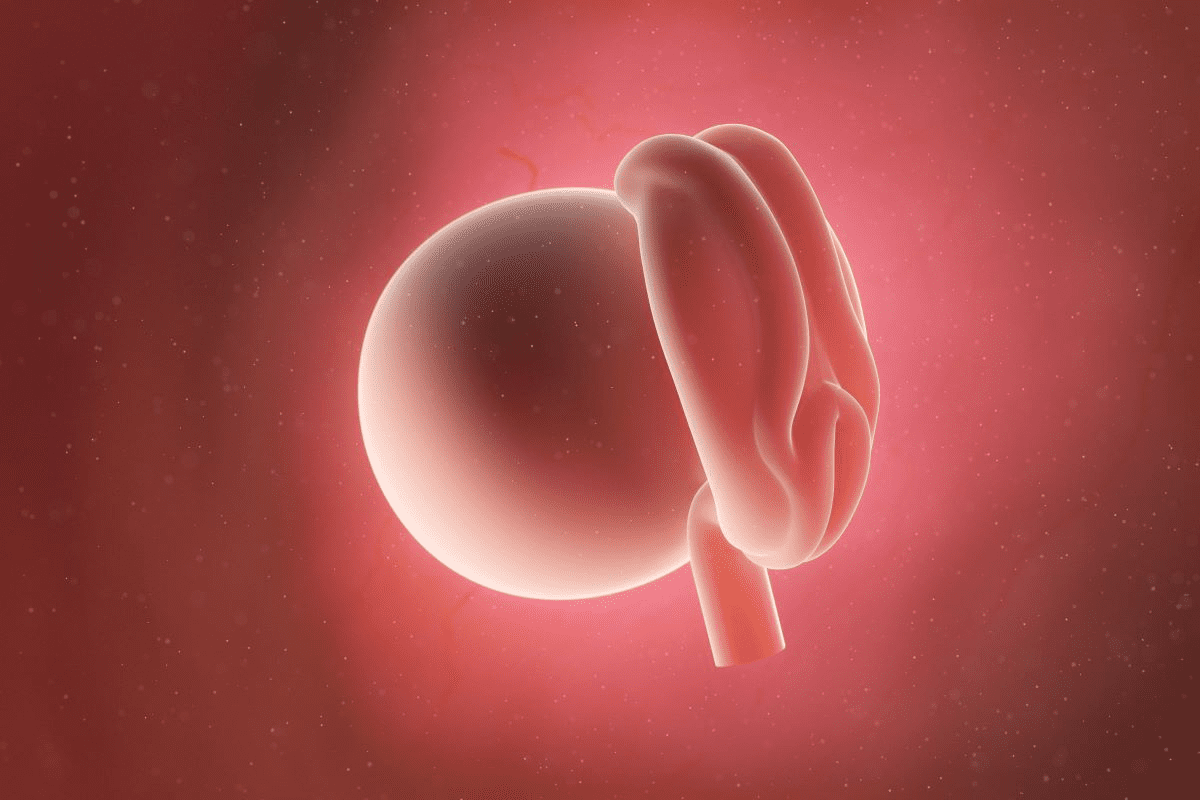
Grade 6: The Fully Hatched Blastocyst Stage
The ‘6’ in 6BA means the embryo has fully hatched. This is a big deal because it shows the embryo is ready to implant in the uterus. This usually happens 5-6 days after fertilization.
The fully hatched blastocyst stage is a big step in embryo growth. It shows the embryo has a good chance of implanting well.
Grade B: Good Inner Cell Mass Quality Explained
The ‘B’ in 6BA shows the inner cell mass (ICM) quality. The ICM is where the fetus will form. A ‘B’ grade means the ICM is healthy and can grow into a fetus.
The quality of the inner cell mass is key for implantation and growth.
Grade A: Excellent Trophectoderm Quality Explained
The second ‘A’ in 6BA talks about the trophectoderm quality. This outer layer forms the placenta and other needed tissues. An ‘A’ grade means the trophectoderm is strong and healthy, supporting implantation and growth.
Good trophectoderm quality is essential for implantation. It helps the embryo attach to the uterine lining for a successful pregnancy.
To sum up, a 6BA embryo is fully hatched, with good inner cell mass and excellent trophectoderm. This makes it a top choice for successful implantation and pregnancy.
How 6BA Embryos Compare to Other Grades
In the world of fertility treatments, embryo quality is very important. 6BA embryos are often seen as good choices for transfer. It’s key to know how they stack up against others in terms of quality and success.
The Hierarchy of Embryo Quality Categories
Embryo quality depends on several things. These include the stage of development, the inner cell mass, and the trophectoderm. The Gardner blastocyst grading system is used in IVF clinics to categorize embryos.
6BA embryos are considered high quality. They are at an advanced stage (grade 6), have good inner cell mass (grade B), and excellent trophectoderm (grade A).
Comparing 6BA to Top-Tier Grades (5AA, 4AA)
Grades like 5AA and 4AA are among the best. They have excellent inner cell mass and trophectoderm. 6BA embryos are not top-tier because their inner cell mass is grade B, not A.
But, research shows that 6BA embryos have a live birth rate of about 46.8%. This means they are a very good choice for patients, even if they’re not the absolute best.
Comparing 6BA to Other Good-Quality Embryos (5BA, 6BB)
6BA embryos are compared to other good-quality embryos like 5BA and 6BB. They are all viable options for transfer. 5BA embryos are at an earlier stage but have excellent trophectoderm.
6BB embryos have good inner cell mass but lower trophectoderm grade. But, the success rate for these embryos is high. This shows patients have many good options, depending on their situation.
In conclusion, 6BA embryos are very competitive in success rates. They are not the absolute best but are close. Knowing this helps patients and doctors make better decisions about embryo transfer.
Understanding 6BA Embryo Success Rates
When thinking about fertility treatments, knowing the success rates of 6BA embryos is key. The success of an embryo depends on its quality, the age of the person, and the fertility treatment used.
Implantation Rates: What Research Shows
Research shows that 6BA embryos have high implantation success rates. This is good news for those going through fertility treatments.
Key findings on implantation rates include:
- High-quality embryos have better implantation rates
- The uterine environment plays a key role in successful implantation
- Matching embryo development with uterine preparation is vital
Clinical Pregnancy Rates: Around 60%
The clinical pregnancy rate for 6BA embryos is about 60%. This is a strong sign of a successful pregnancy.
The rate is influenced by:
- The embryo’s quality
- The uterus’s readiness
- The health of the person undergoing treatment
Live Birth Rates: Approximately 46.8%
The goal of fertility treatment is a live birth. 6BA embryos have a live birth rate of about 46.8%. This rate is lower than the clinical pregnancy rate but shows the challenges of fertility treatments.
Factors affecting live birth rates include:
- The age of the individual
- Any health conditions
- The quality of prenatal care
Knowing these success rates helps people make better choices about their fertility journey. By looking at implantation, clinical pregnancy, and live birth rates for 6BA embryos, we can better understand fertility treatments.
Day 6 Blastocysts: Development Timeline and Clinical Significance
Day 6 blastocysts grow slower than day 5 ones but have a good chance of leading to pregnancy. Knowing how they develop is very important.
The Standard Embryo Development Timeline
Embryos usually grow at a set pace during IVF. Most reach the blastocyst stage by day 5. But, some might need an extra day, becoming blastocysts on day 6. This extra time doesn’t always mean there’s a problem with the embryo.
The timeline for growth is as follows: fertilization happens on day 0. Then, the embryo goes through cell divisions before becoming a blastocyst around day 5 or 6. The blastocyst stage is key because it’s when the embryo is ready to implant in the uterus.
Why Some Embryos Develop More Slowly
Many things can affect how fast an embryo grows. These include the egg and sperm quality, lab conditions, and the embryo’s genetics. Research shows that slower-growing embryos might have unique traits that could impact their chances of implanting and growing.
It’s important to remember that an embryo’s growth rate is just one thing that matters for a successful pregnancy. The quality of the inner cell mass and trophectoderm also play big roles.
Genetic Implications of Slower Development
Research has looked into the genetic aspects of slower-growing embryos, like day 6 blastocysts. Some studies suggest these embryos might face a higher risk of genetic problems. But, the findings are not clear-cut, and more research is needed to understand this link.
The introduction of preimplantation genetic testing (PGT) has helped assess embryos more closely, including slower-growing ones. PGT can spot genetic issues, giving valuable insights for choosing which embryos to transfer.
Fresh vs. Frozen Transfer Strategies for Day 6 Blastocysts
It’s key to know the differences between fresh and frozen transfers for day 6 blastocysts. This choice can greatly affect IVF success. Transferring a blastocyst fresh or after freezing can make a big difference.
Limitations of Fresh Transfers
Studies show fresh transfers of day 6 blastocysts have lower success rates, about 15%. This is due to several reasons. The uterine environment might not be ready for the embryo’s stage.
Fresh transfers might not prepare the uterine lining well for implantation. Ovarian stimulation in IVF can make the uterus less ready for the embryo.
Advantages of Frozen Transfers
On the other hand, frozen transfers of day 6 blastocysts have higher success rates, around 50%. Frozen transfers have many benefits. They allow for better timing of the embryo transfer with the uterine environment.
Frozen embryo transfers (FET) help prepare the uterine lining better. This is because the uterine lining can grow naturally without the effects of IVF drugs. This timing is key for successful implantation.
The Critical Role of Endometrial Synchronization
Endometrial synchronization is very important for embryo transfer success. The uterine lining must be ready to support the embryo. Frozen transfers help control when the embryo is transferred, ensuring it’s at the best time.
This precise timing in frozen cycles boosts the chances of successful implantation and pregnancy. It’s a popular choice in IVF because of its better results.
Beyond Grading: Other Factors Affecting 6BA Embryo Success
The success of a 6BA embryo transfer is not just about its grade. Other important factors also play a big role in IVF treatment outcomes.
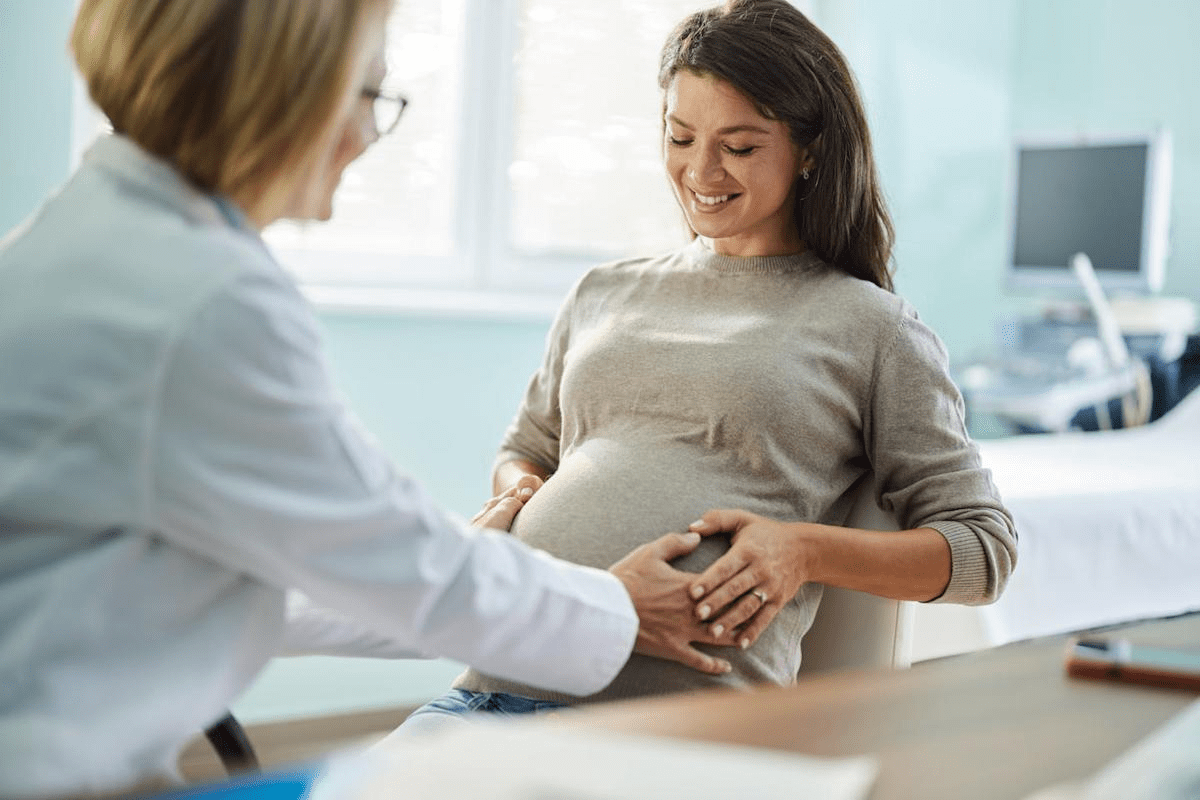
Maternal Age and Its Impact
Maternal age is a key factor in IVF success, including with 6BA embryos. As women get older, their eggs’ quality and number drop, affecting embryo health.
- Women under 35: Usually have better IVF success rates due to egg quality.
- Women between 35-40: May see lower success rates as egg quality starts to decline.
- Women over 40: Face much lower success rates due to egg quality drop and chromosomal issues.
The Role of Preimplantation Genetic Testing
Preimplantation genetic testing (PGT) is also vital for 6BA embryo transfers. PGT helps pick embryos without genetic problems, boosting pregnancy chances.
Benefits of PGT:
- It lowers miscarriage risk by spotting abnormal embryos.
- It boosts pregnancy success by choosing healthy embryos.
- It reduces genetic disorder risk in offspring.
Uterine Receptivity Factors
Uterine receptivity is key for 6BA embryo implantation. Factors like endometrial thickness, uterine lining quality, and hormonal balance are very important.
- Endometrial thickness: Right thickness is essential for implantation.
- Uterine lining quality: A healthy lining is vital for embryo implantation.
- Hormonal balance: Proper hormonal levels, like progesterone, keep the uterus ready.
Clinic-Specific Success Variations
Success rates with 6BA embryos can differ between clinics. This is due to protocol, experience, and technology differences.
Clinic Factor | Impact on Success Rate |
Experience with IVF | More experienced clinics tend to have higher success rates. |
Technology and Equipment | Advanced technology can improve embryo handling and transfer success. |
Protocols and Personalization | Tailored treatment plans can enhance individual success rates. |
Conclusion: Making Informed Decisions About Your Fertility Journey
Knowing about 6BA embryos is key for those on a fertility path. We’ve looked at how IVF clinics grade embryos and the importance of 6BA ones. We’ve also talked about what affects their success.
Learning about 6BA embryos helps people make better choices for their fertility care. The data on implantation and pregnancy rates gives patients a clear view. It helps them talk better with their doctors.
In the end, a 6BA embryo is a top-notch blastocyst with a strong chance of success. But, getting pregnant is more than just the embryo’s quality. Things like the mother’s age, genetic testing, and how well the uterus receives the embryo matter too. By understanding these points, people can improve their fertility treatment plans. This way, they can make smart choices on their fertility journey.
FAQ
What is a 6BA embryo?
A 6BA embryo is fully developed and ready to implant. It has a strong inner cell mass and top-notch trophectoderm. This makes it a strong candidate for successful implantation.
How is embryo grading done?
Grading is based on the Gardner blastocyst system. It looks at expansion, inner cell mass quality, and trophectoderm quality.
What is the success rate of a 6BA embryo?
A 6BA embryo has a live birth success rate of about 46.8%. Clinical pregnancy rates are around 60%. Implantation rates vary based on several factors.
How does a 6BA embryo compare to other grades?
A 6BA embryo is of high quality, similar to 5AA or 4AA. It has a higher success rate than lower-grade embryos.
What is the difference between a day 5 and day 6 blastocyst?
Day 5 and day 6 blastocysts develop at different speeds. Day 6 develops more slowly, which might have genetic implications.
Is fresh or frozen transfer better for day 6 blastocysts?
Frozen transfer is better for day 6 blastocysts. Success rates are around 50%. Fresh transfer success rates are about 15%.
How does maternal age affect 6BA embryo success?
Maternal age greatly affects 6BA embryo success. Older age can lower success rates due to declining egg quality.
What is the role of preimplantation genetic testing in 6BA embryo success?
Preimplantation genetic testing can identify normal embryos. This can improve success rates for 6BA embryos.
How does uterine receptivity affect 6BA embryo success?
Uterine receptivity is key for 6BA embryo success. A receptive uterus is essential for successful implantation.
Can clinic-specific success variations affect 6BA embryo success rates?
Yes, clinic-specific success variations can impact 6BA embryo success rates. Different clinics have varying success rates due to treatment protocols and expertise.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34486510/