Last Updated on November 4, 2025 by mcelik

Feeling pain or discomfort in the back of your legs can really get in the way of your day. At Liv Hospital, we get how much leg pain can worry you.
We’ll look into why the back of your legs might hurt and how to make it better. Leg pain is common, often because of muscle cramps. Knowing what’s causing it is key to feeling better.
Key Takeaways
- Find out what usually causes leg pain
- Learn how to stop it from happening again
- See how Liv Hospital’s team can help with hamstring discomfort
- Discover ways to feel better and move easier
Understanding the Anatomy Behind Back of Legs Pain
Knowing the anatomy of the back of our legs is key to figuring out calf soreness and thigh ache. Our legs’ backside has muscles, nerves, and other parts. They all work together to help us move and do daily tasks.
Key Muscles and Structures in the Posterior Leg
The back of our legs has important muscles and structures that can get hurt. These include:
- The gastrocnemius and soleus muscles, which form the calf and help with ankle movement.
- The hamstring muscles, which run down the back of the thigh. They help bend the knee and straighten the hip.
- The tibial nerve, which runs down the back of the leg. It can get compressed, causing pain and discomfort.
How Pain Signals Travel Through the Leg
Pain signals in the leg follow a complex network of nerves. When something hurts, special nerve endings called nociceptors detect it. These signals then go to the spinal cord and brain, where they’re seen as pain.
Many things can affect how pain signals travel. This includes inflammation, compression, and damage to nerves or tissues. Knowing this helps us find better ways to treat lower limb discomfort.
Recognizing Different Types of Back of Legs Ache
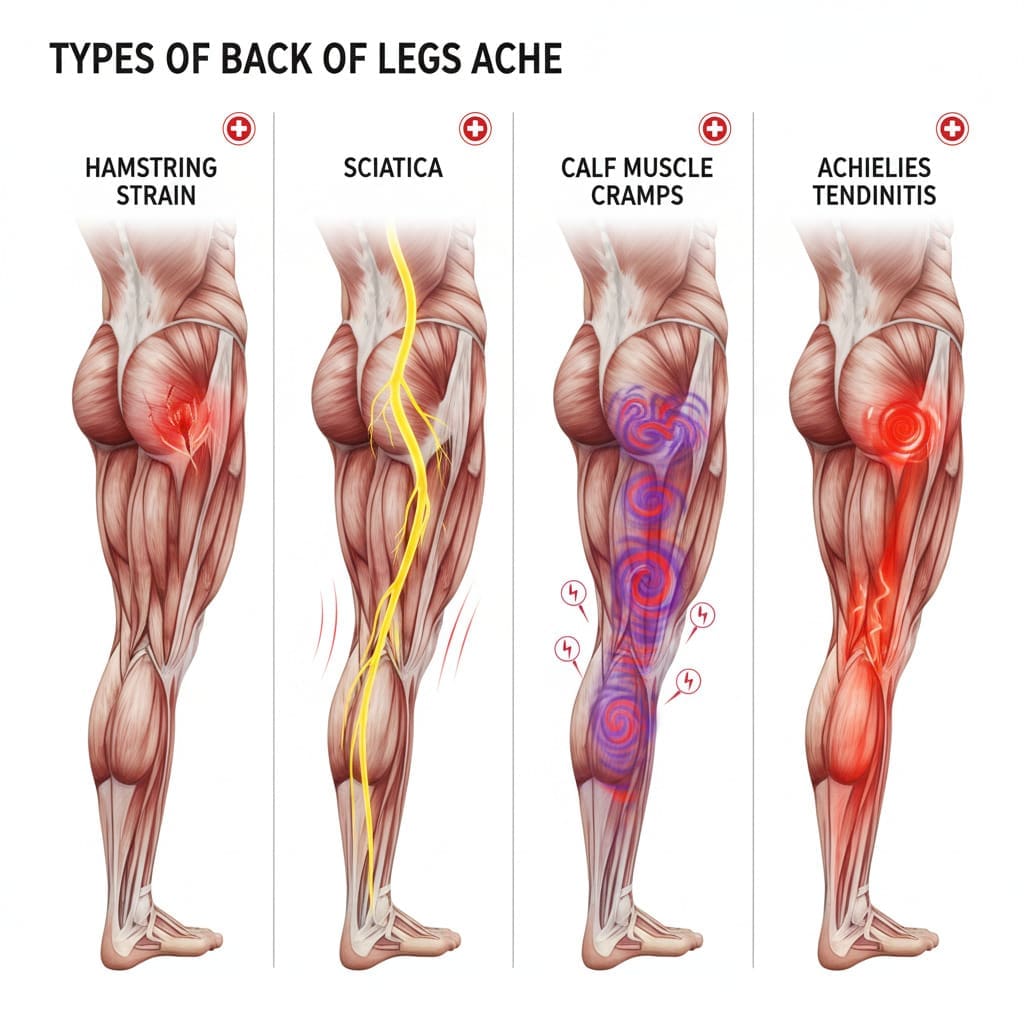
The back of our legs can ache in many ways. Each type of ache points to different causes. Knowing these differences is key for the right diagnosis and treatment.
Acute vs. Chronic Posterior Leg Pain
Posterior leg pain falls into two main types: acute and chronic. Acute pain is sharp and sudden, usually from injury or strain. Chronic pain, lasting over three months, suggests an ongoing issue.
A medical expert says, “Chronic pain is not just long-term acute pain. It’s a unique condition needing a special management plan.” Knowing if pain is acute or chronic helps choose the right treatment.
Pain Patterns: Radiating, Localized, and Referred
Pain in the back of the legs can also be classified by its pattern. Radiating pain travels along a nerve path, feeling sharp and shooting. Localized pain stays in one area, showing a problem there. Referred pain is felt in the leg but comes from another spot, like the lower back.
For example, sciatica is radiating pain following the sciatic nerve from the lower back to the legs. Localized pain might stem from muscle strain or injury in the calf or hamstring. Referred pain could be from issues like a lumbar disc herniation, where the spine problem causes leg pain.
An orthopedic specialist notes, “Knowing the pain pattern is vital for finding the cause and creating a treatment plan.” By identifying if pain is radiating, localized, or referred, doctors can focus on the right causes and treatments.
Cause #1: Muscle Cramps and Dehydration
Dehydration and mineral imbalances often cause painful muscle cramps in the legs. These cramps are a common reason for back of legs ache. We will look at what causes this and how to find relief.
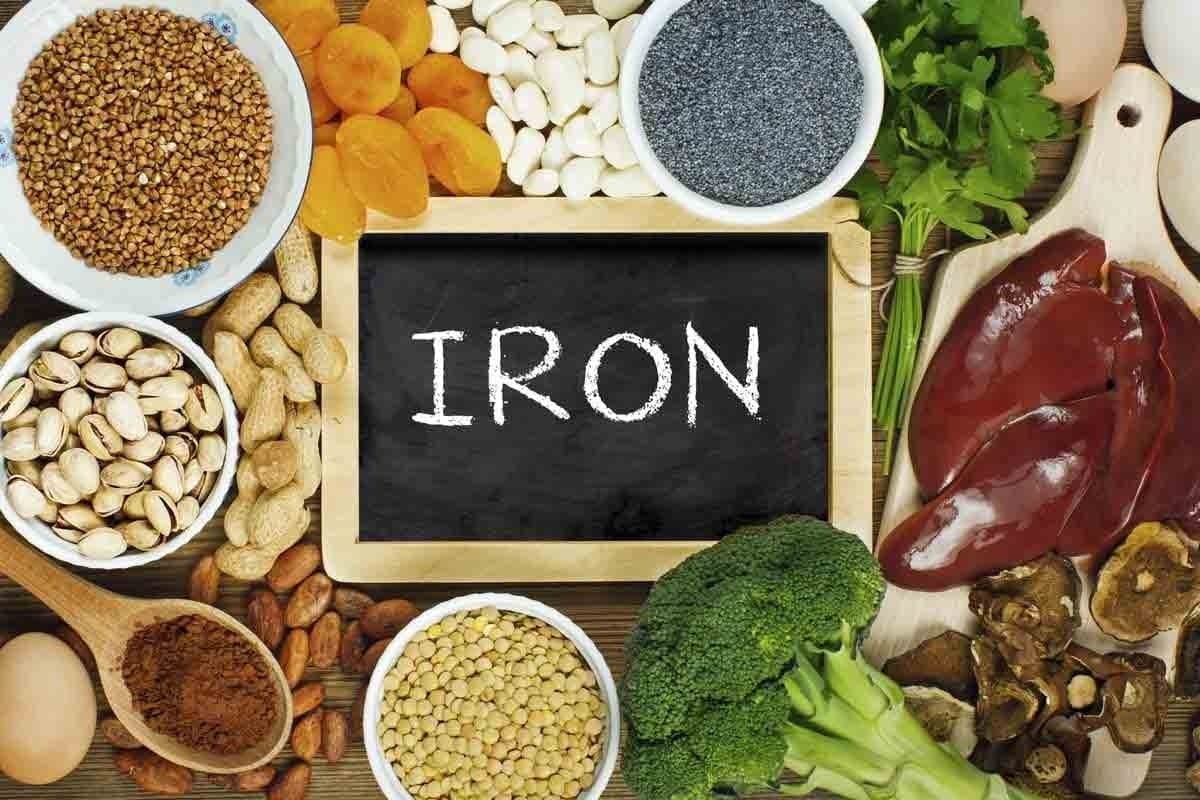
Mineral Imbalances and Their Effect on Leg Muscles
Mineral imbalances, like sodium, potassium, calcium, and magnesium, affect muscle function. An imbalance can cause muscle cramping. Potassium and magnesium are key because they control muscle contractions.
“The role of magnesium in muscle function cannot be overstated,” say healthcare experts. “It helps muscles relax after contraction, and a lack of it can cause cramping.”
Immediate Relief Strategies for Muscle Cramps
Several methods can help when you have a muscle cramp:
- Stretching the affected muscle
- Applying heat or cold packs
- Massaging the cramped area
- Replenishing fluids and electrolytes
For hamstring discomfort, stretching the back of the leg can help quickly. It’s also important to drink plenty of water and keep electrolyte levels balanced to avoid future cramps.
Prevention Through Proper Hydration and Nutrition
To prevent muscle cramps, you need to stay hydrated and eat right. Drinking enough water and getting the right minerals is key. Eating fruits, vegetables, and whole grains helps keep electrolyte levels up.
| Mineral | Food Sources | Role in Muscle Function |
|---|---|---|
| Potassium | Banana, Spinach, Avocado | Regulates muscle contractions |
| Magnesium | Nuts, Seeds, Whole Grains | Relaxation of muscles |
Knowing why muscle cramps happen and taking steps to prevent them can help. A healthy lifestyle, including drinking enough water and eating well, is essential to avoid muscle cramps.
Cause #2: Sciatica and Nerve Root Compression
Many people experience pain in the back of their legs due to sciatica. This condition is caused by nerve root compression. Sciatica pain follows the sciatic nerve from the lower back to the hips and down each leg. Knowing what causes sciatica is key to managing it effectively.
How Sciatica Creates Radiating Back of Legs Ache
Sciatica happens when the sciatic nerve gets irritated or compressed. This can be due to a herniated disk, bone spur, or a narrowed spine. The compression leads to pain that spreads from the lower back to the legs. This pain can be mild or severe and may also cause tingling, numbness, or weakness in the leg.
Conservative Treatment Approaches
For sciatica, treatments often include physical therapy, stretching, and pain management. Physical therapy helps improve flexibility and strengthens back muscles. Stretching exercises help ease tension on the sciatic nerve. Over-the-counter pain relievers and anti-inflammatory drugs can also help.
- Physical therapy to improve flexibility and strength
- Stretching exercises to alleviate tension on the sciatic nerve
- Pain management through medication
When to Consider Medical Intervention
While many cases of sciatica can be treated without surgery, some need medical help. If the pain is very bad, doesn’t go away, or comes with other symptoms like weakness, loss of bladder or bowel control, or fever, you should see a doctor. Doctors might suggest corticosteroid injections or surgery to relieve nerve compression.
Figuring out why you have leg pain is the first step to getting better. By tackling the root cause of sciatica, you can find relief and live better.
Cause #3: Lumbar Herniated Discs
Herniated discs in the lumbar area often cause lower limb discomfort. When the soft inner gel leaks out, it can irritate nerves. This leads to pain that spreads down to the legs. We’ll look at how this affects leg pain, the importance of physical therapy, and long-term management strategies.
The Disc-Nerve Connection in Leg Pain
The lumbar spine has discs that act as shock absorbers. When a disc herniates, it can press on or irritate nerves. This can cause pain, numbness, or weakness in the legs, depending on the nerve affected.
Understanding the disc-nerve connection is key to diagnosing and treating leg pain from herniated discs. We use MRI to see how the disc affects nerves. This helps us make the right treatment choices.
Physical Therapy Protocols for Disc-Related Pain
Physical therapy is essential for managing pain from herniated discs. Our therapists create custom exercise plans. These plans strengthen the muscles supporting the spine, improve flexibility, and enhance posture. This can help reduce pressure on nerves, easing leg pain and improving function.
Some common physical therapy protocols include:
- Core strengthening exercises to support the lumbar spine
- Stretching routines to improve flexibility and reduce muscle tension
- Manual therapy techniques to mobilize the spine and surrounding tissues
Long-Term Management Strategies
Managing herniated discs long-term requires a variety of strategies. We suggest maintaining a healthy weight, exercising regularly, and practicing good posture. Also, learning proper lifting techniques and taking breaks when sitting or standing for long periods can help prevent worsening symptoms.
For some, lifestyle modifications may need to be combined with ongoing physical therapy or other treatments. We work with our patients to create a detailed plan. This plan addresses their unique needs and promotes long-term spinal health.
Cause #4: Spinal Stenosis and Age-Related Changes
Spinal stenosis is a common cause of leg pain in older adults. It happens when the spinal canal narrows. This can put pressure on nerves, causing pain, numbness, or weakness in the legs.
Narrowing of the Spinal Canal and Its Effects
The spinal canal is like a tube that holds the spinal cord and nerves. When it narrows, it can compress nerves. This can lead to pain, numbness, or weakness in the legs, making it hard to walk or stand for long.
For more information on managing back pain, you can visit Total Pain Specialist. They offer insights into effective treatments and debunk common myths about back pain.
Activity Modifications to Reduce Symptoms
Making lifestyle changes can help with spinal stenosis symptoms. These include:
- Maintaining a healthy weight to reduce pressure on the spine
- Engaging in exercises that strengthen the back and abdominal muscles
- Avoiding activities that worsen the condition, such as heavy lifting or bending
- Using proper posture techniques when sitting, standing, or sleeping
| Activity | Benefit |
|---|---|
| Swimming | Low-impact exercise that strengthens muscles without straining the spine |
| Cycling | Improves cardiovascular health and strengthens leg muscles |
| Stretching | Enhances flexibility and reduces muscle tension |
Medical and Surgical Options for Severe Cases
If conservative treatments don’t work, medical or surgical options may be needed. These include:
- Medications: Pain relievers, corticosteroids, or muscle relaxants to manage pain and inflammation
- Physical Therapy: Customized exercise programs to improve mobility and strength
- Surgery: Procedures such as laminectomy or spinal fusion to relieve pressure on the nerves or stabilize the spine
It’s important to talk to a healthcare professional to find the best treatment. This depends on the severity of symptoms and overall health.
Cause #5: Overuse Injuries in Athletes and Active Individuals
Repetitive strain from overuse injuries can cause hamstring discomfort and calf soreness in athletes. These injuries happen when athletes do the same activities too much without resting. This puts a lot of strain on the muscles and tendons in the back of the leg.
Common Overtraining Patterns Leading to Posterior Leg Pain
Overtraining can lead to pain in the back of the leg. This includes sudden increases in training, not warming up or cooling down properly, and poor movement. Many athletes forget to take rest days, which increases the risk of injury.
To lower this risk, athletes should slowly increase their training. This lets their muscles and tendons get used to the demands.
The RICE Protocol and Its Application
The RICE protocol is a good treatment for overuse injuries. RICE means Rest, Ice, Compression, and Elevation.
- Rest: Stay away from activities that make the injury worse.
- Ice: Use ice to lessen pain and swelling.
- Compression: Wear compression bandages to reduce swelling.
- Elevation: Keep the injured leg higher than your heart to lessen swelling.
By using the RICE protocol, athletes can lessen the severity of injuries and help their body heal.
Gradual Return to Activity Guidelines
After an injury, it’s important to follow a gradual return to activity plan. This means slowly adding more intensity and volume to your training. This lets the injured areas get stronger and more resilient.
Start with easy activities and gradually make them harder as you can. Always watch for signs of injury, like pain or swelling, during this time.
Cause #6: Vascular Disorders and Circulation Problems
Vascular disorders can really hurt your legs, causing pain and discomfort. These issues affect the blood vessels and how blood flows. If not treated, they can lead to serious problems.
Peripheral Artery Disease Symptoms in the Legs
Peripheral artery disease (PAD) happens when arteries narrow, cutting off blood to the legs. You might feel pain in your legs when you walk. You could also notice your lower leg or foot feels cold. And, wounds or sores that won’t heal are a sign too.
Deep Vein Thrombosis Warning Signs
Deep vein thrombosis (DVT) is a blood clot in the deep veins, often in the legs. Look out for swelling in one leg, pain or tenderness, and warmth or redness.
Improving Circulation Through Lifestyle Changes
There are ways to improve circulation and ease symptoms of vascular disorders. Start by exercising regularly, quitting smoking, and keeping a healthy weight.
| Lifestyle Change | Benefit |
|---|---|
| Regular Exercise | Improves blood flow and overall circulation |
| Quitting Smoking | Reduces vascular constriction and improves circulation |
| Healthy Weight | Reduces pressure on veins and improves circulation |
By making these lifestyle changes, you can boost your circulation. This can help lower the risk of serious problems from vascular disorders.
Cause #7: Piriformis Syndrome and Deep Muscle Issues
The piriformis muscle is deep in the buttocks. It can cause leg pain when it’s irritated or inflamed. This muscle helps rotate the hip and stabilize the hip joint.
When it’s tight or inflamed, it can press on the sciatic nerve. This leads to pain, numbness, and tingling in the back of the leg.
Differentiating Piriformis Pain from Other Conditions
Piriformis syndrome can be hard to diagnose because its symptoms are similar to other conditions. But, there are signs that can help tell it apart:
- Pain is usually in the buttock area and can spread down the back of the leg.
- Symptoms get worse with activities that involve hip rotation, like climbing stairs or getting in and out of a car.
- The piriformis muscle area is tender to the touch.
Healthcare professionals use physical exams, patient history, and sometimes imaging to diagnose piriformis syndrome. They do this to rule out other causes.
Targeted Stretches for the Piriformis Muscle
Stretching is key in managing piriformis syndrome. Here are some effective stretches:
- Piriformis Stretch: Sit on the floor with the affected leg crossed over your other leg. Place your hand on the knee of the crossed leg and pull it toward your opposite shoulder. You should feel a stretch in the back of your leg.
- Supine Piriformis Stretch: Lie on your back with both knees bent. Cross the affected leg over the other, placing the ankle on the opposite knee. Gently pull the knee toward your chest until you feel a stretch.
Regular stretching can ease tension in the piriformis muscle and reduce symptoms.
Manual Therapy and Massage Techniques
Manual therapy, including massage, is very effective for piriformis syndrome. Techniques may include:
| Therapy Type | Description | Benefits |
|---|---|---|
| Deep Tissue Massage | Targets the deeper layers of muscle and connective tissue | Relieves tension in the piriformis muscle |
| Myofascial Release | Applies sustained pressure to connective tissue | Reduces muscle tightness and improves range of motion |
| Trigger Point Therapy | Applies pressure to specific areas of muscle tension | Relieves pain and stiffness in the piriformis muscle |
These manual therapies can be used with stretching exercises for full relief from piriformis syndrome symptoms.
Comprehensive Relief Plan for Persistent Back of Legs Ache
Managing back of legs ache needs a full plan that covers all angles. This pain can really affect your daily life. So, it’s key to use many ways to ease the pain and boost your health.
Creating a Multi-Modal Pain Management Strategy
A good plan mixes different treatments for back of legs ache. This might include:
- Medicines to control pain and swelling
- Physical therapy to build strength and improve posture
- Changes in lifestyle like diet, exercise, and managing stress
Doctors say, “A multi-modal plan is more personalized. It meets each patient’s specific needs.”
Complementary Approaches: Acupuncture, Yoga, and Mindfulness
Along with usual treatments, other methods can help too. Acupuncture, yoga, and mindfulness can lessen pain and make life better.
“Mindfulness and yoga can help reduce pain perception by promoting relaxation and reducing stress.”
Adding these methods to your plan can make it more effective.
Building a Support Team of Healthcare Professionals
Dealing with ongoing back of legs ache often means having a team. This team might include:
- Primary care doctors for overall health
- Orthopedic specialists for bone and muscle issues
- Physical therapists for custom exercise plans
- Pain management experts for advanced treatments
Together, these experts can offer a unified care plan. This ensures all parts of the condition are looked after.
Prevention Strategies for Recurring Leg Pain
To stop leg pain from coming back, we need to make lifestyle changes and do specific exercises. Knowing why leg pain happens helps us avoid it. This way, we can stay comfortable and keep moving easily.
Ergonomic Considerations for Daily Activities
Our daily tasks can affect our leg health. Making sure our workspaces are set up right helps our legs. For example, changing chair heights and using standing desks helps spread out our weight.
Making small changes, like stretching and moving often, can also help avoid leg pain.
| Ergonomic Adjustment | Benefit |
|---|---|
| Adjusting chair height | Reduces strain on legs |
| Using standing desks | Distributes weight evenly |
| Taking regular breaks | Reduces muscle fatigue |
Strengthening Exercises for Posterior Leg Stability
It’s important to make the muscles in the back of our legs strong. This helps keep our legs stable and lowers pain risk. Doing hamstring curls and calf raises is very helpful.
“Strengthening the hamstrings and calf muscles through regular exercise can significantly reduce the incidence of leg pain.”
- Hamstring curls: Strengthens the hamstring muscles
- Calf raises: Strengthens calf muscles
- Deadlifts: Works multiple muscle groups including hamstrings
Flexibility Routines to Maintain Muscle Health
Keeping our muscles flexible is key to avoiding muscle strain and pain. Regular stretching boosts our range of motion and lowers muscle tightness.
Doing hamstring and calf stretches daily is great. It boosts flexibility and cuts down on leg pain risk.
When to Seek Immediate Medical Attention
It’s important to know when your leg pain needs quick medical help to avoid lasting damage. Many leg pain causes are not serious and can be treated without surgery. But, some symptoms need urgent medical check-ups.
Red Flag Symptoms That Shouldn’t Be Ignored
Some symptoms with leg pain are “red flags” because they might mean a serious problem. These include:
- Sudden, severe pain that doesn’t get better with rest or medicine.
- Swelling, warmth, or redness in the leg, which could be a blood clot or infection.
- Numbness or tingling that keeps getting worse.
- Weakness in the leg that makes it hard to walk or do daily tasks.
- Loss of bladder or bowel control, which is a medical emergency.
What to Tell Your Doctor About Your Leg Pain
When you see a doctor for leg pain, being ready with all the details helps them diagnose you right. Here’s what to remember:
- The location and how bad your pain is.
- How long you’ve had symptoms and what makes them better or worse.
- Any recent injuries or activities that might be linked to your pain.
- Your medical history, including any health issues you already have.
- Any medications or supplements you’re taking now.
As
“The more information you can give your doctor, the better they can understand your condition and come up with a good treatment plan.”
Telling your doctor all about your symptoms and health history is key to getting the right care.
Conclusion: Taking Control of Your Leg Health and Comfort
Back of legs ache can come from many sources. This includes muscle cramps, sciatica, and spinal problems. Knowing what causes the pain is key to feeling better.
We’ve looked at ways to ease leg pain. This includes quick fixes and long-term plans. Drinking enough water, eating right, and staying active can help a lot. If pain doesn’t go away, seeing a doctor is important.
Looking after your legs is important for your health. Being aware and taking action can help reduce pain. We suggest talking to a doctor to make a plan for better leg health.
FAQ
What are the most common causes of back of legs ache?
Common causes include muscle cramps, sciatica, and lumbar herniated discs. Spinal stenosis, overuse injuries, and vascular disorders also play a role. Piriformis syndrome is another common cause.
How can I differentiate between acute and chronic posterior leg pain?
Acute pain comes from sudden injuries or strains. Chronic pain lasts longer and might be due to spinal stenosis or vascular disorders.
What are the symptoms of sciatica and how is it treated?
Sciatica causes pain that radiates down the leg, often with numbness or tingling. Treatment includes physical therapy, steroid injections, or surgery.
How can I prevent muscle cramps and dehydration-related leg pain?
Stay hydrated and eat enough minerals like potassium, magnesium, and calcium. Regular stretching also helps prevent muscle cramps.
What lifestyle changes can improve circulation and reduce vascular-related leg pain?
Quit smoking and exercise regularly. Keep a healthy weight and manage diabetes and hypertension to improve circulation.
What are the warning signs of deep vein thrombosis (DVT) that I should be aware of?
Look out for sudden swelling, pain, or tenderness in one leg. Also, watch for warmth or redness and fever. Seek medical help if you notice these signs.
How can I manage piriformis syndrome and alleviate its symptoms?
Use targeted stretches for the piriformis muscle. Manual therapy and physical therapy can also help improve mobility in the hip and lower back.
What are the benefits of a multi-modal pain management strategy for back of legs ache?
A multi-modal approach combines treatments like medication and physical therapy. It also includes complementary therapies and lifestyle changes for better relief.
When should I seek immediate medical attention for my leg pain?
Get medical help right away for red flag symptoms. These include sudden severe pain, loss of bladder or bowel control, fever with leg pain, or signs of DVT.
How can I prevent recurring leg pain through ergonomic considerations and exercise?
Make ergonomic changes to daily activities. Do strengthening exercises for the posterior leg and keep up with flexibility routines to prevent pain.
What information should I provide to my doctor about my leg pain?
Tell your doctor about your pain’s location, severity, and how long it lasts. Mention any triggers and associated symptoms. Share your medical history and lifestyle factors too.
References
Healthline — What’s Causing My Lower Back and Leg Pain?