Last Updated on November 18, 2025 by Ugurkan Demir

Medical technology has made big strides in spinal surgery types. Now, patients have many effective treatments for back issues.
At Liv Hospital, we know how complex back problems can be. We’re here to offer top-notch healthcare to international patients. Issues like herniated or ruptured disks, spinal stenosis, and degenerative disk disease might need surgery.
Our team is here to help you understand the back procedures available. We aim to support you in making the best choices for your care. Our focus is on improving your quality of life through exceptional care.
Key Takeaways
- Modern spinal surgery techniques address a range of back conditions.
- Various back procedures are available, including those for degenerative disk disease.
- Liv Hospital provides complete support for international patients.
- Expert guidance is available for navigating treatment options.
- Patient-centered care is a top priority.
The Evolution of Modern Spine Surgery

Modern spine surgery has become more effective and less invasive. We’ve seen big improvements in surgical techniques, diagnostic tools, and patient care. These changes have greatly improved results for those having spinal operations.
Advancements in Surgical Techniques
Today’s spine surgery uses advanced techniques like minimally invasive procedures and new tools. These changes have cut down recovery times and reduced complications. This makes spinal surgery a better option for more people. Minimally invasive spine surgery uses smaller cuts, less damage to tissue, and less blood loss. This leads to faster recovery times.
Common Spinal Conditions Requiring Surgery
Many spinal conditions need surgery, like herniated discs, spinal stenosis, scoliosis, and vertebral fractures. Surgery is usually considered after other treatments don’t work. Spinal fusion, laminectomy, and discectomy are common surgeries for these issues.
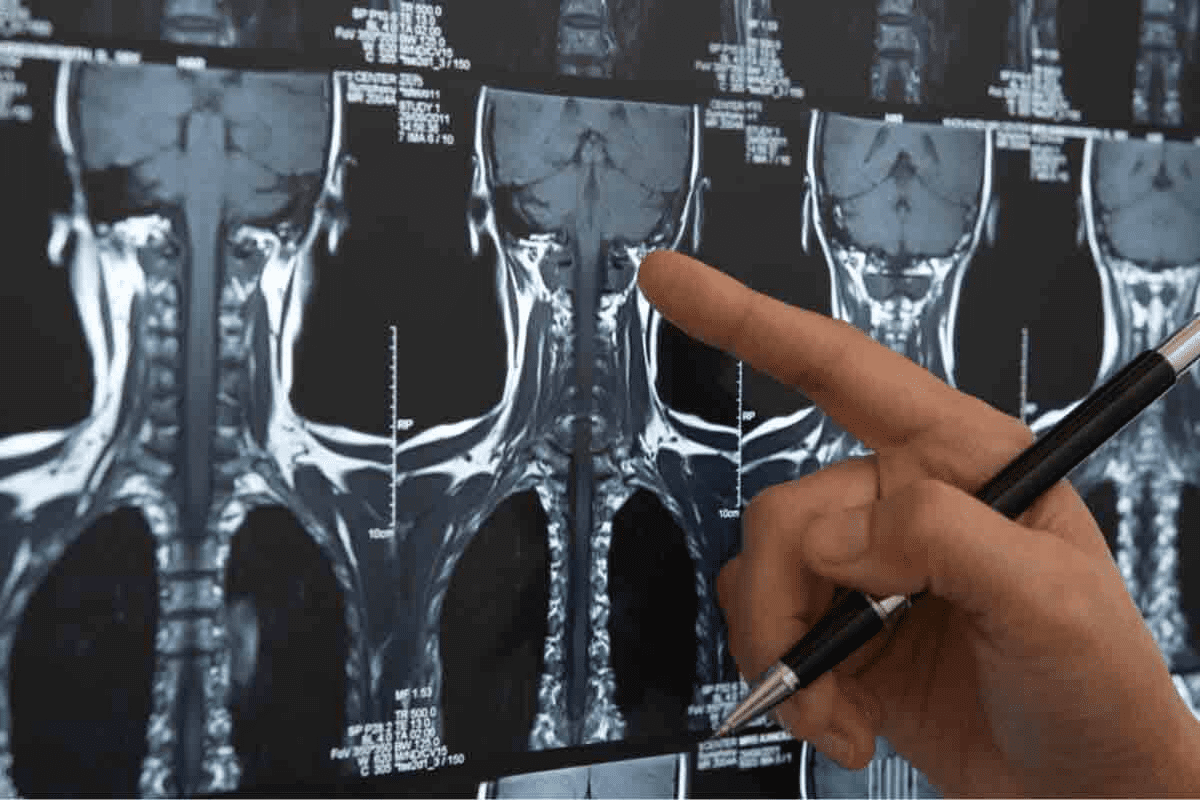
Pre-Surgical Evaluation Process
A detailed pre-surgery check is key to picking the right surgery. This includes a full medical history, physical exam, and imaging tests. We use this info to weigh the surgery’s risks and benefits and create a custom plan. We consider the patient’s health, age, and condition during this step.
Overview of Common Spinal Surgery Types

It’s important for patients with back pain to know about spinal surgeries. These operations can help by either relieving pressure on nerves or stabilizing the spine. Each type is designed to address different spinal issues.
Categorizing Spine Procedures
Spine procedures fall into several types based on their goals and methods. We group them to understand their uses and benefits. The main groups are decompression, stabilization, and a mix of both.
Decompression vs. Stabilization Surgeries
Decompression surgeries aim to ease pressure on the spinal cord or nerves. Examples include laminectomy and discectomy. Stabilization surgeries, like spinal fusion, focus on strengthening the spine.
Decompression and stabilization surgeries have different goals. Decompression aims to reduce pressure. Stabilization works to improve the spine’s stability.
Factors Influencing Surgical Approach
The type of surgery chosen depends on several factors. These include the patient’s health, the spinal condition, and how severe it is. Treatment plans for thoracolumbar spine fractures are tailored to each patient.
We consider these factors to pick the best surgical method. This ensures the best results for the patient. Knowing about back surgery types helps patients make better treatment choices.
Spinal Fusion: Permanently Connecting Vertebrae
Spinal fusion is a top choice for treating serious spinal problems. It makes two or more vertebrae stick together. This helps stabilize the spine and reduce pain.
The Fusion Process and Bone Grafting
The spinal fusion starts with getting the vertebrae ready. We take out any damaged parts and get the area ready for bone grafting. Bone grafting is key because it helps the vertebrae fuse together.
We use either bone from the patient or donor bone for grafting. This material is essential for the fusion to happen.
Instrumentation Used in Fusion Surgery
To keep the spine stable during fusion, we use special tools. Rods, screws, and cages help hold the vertebrae in place. This lets the bone graft heal and fuse the vertebrae together.
| Instrumentation Type | Purpose | Benefits |
|---|---|---|
| Rods | Provide additional stability to the spine | Enhance fusion success rates |
| Screws | Secure vertebrae in place | Improve spinal alignment |
| Cages | Support the spine while fusion occurs | Promote healthy bone growth |
Recovery Timeline and Success Rates
The time it takes to recover from spinal fusion varies. It depends on the patient’s condition and the surgery’s complexity. Usually, it takes several months to recover.
Research shows spinal fusion works well for many patients. It helps a lot with pain and improves life quality.
Success Rates: Studies show spinal fusion works for over 80% of patients. It helps them feel better and have less pain.
Laminectomy and Decompression Procedures
Laminectomy and decompression procedures are key surgeries for easing pressure on the spinal cord and nerves. They are often needed when spinal stenosis narrows the spinal canal too much. This can lead to pain, numbness, or weakness.
Removing the Lamina to Relieve Pressure
A laminectomy removes part or all of the lamina, a bony part of the spine. This makes more space in the spinal canal. It’s done to take pressure off the spinal cord or nerves from spinal stenosis.
By taking out the lamina, we can decompress the area. This helps reduce symptoms and improves how patients feel.
Foraminotomy and Related Techniques
Other decompression methods, like foraminotomy, are also used. This procedure makes the foramina, where nerves exit the spinal canal, wider. It helps relieve nerve compression.
These methods can be used alone or together. They help achieve the best decompression and symptom relief.
Outcomes and Possible Complications
The results of laminectomy and decompression are usually good, with many feeling much better. But, like any surgery, there are risks. These include infection, nerve damage, or spine instability.
We carefully look at each patient’s situation to lower risks. This helps ensure the best outcome for them.
Knowing about laminectomy and decompression helps patients make better choices. They can work with their healthcare team for the best results.
Discectomy: Treating Herniated and Damaged Discs
Discectomy is a surgery for herniated or damaged discs in the spine. It removes the disk when it presses on nerves or the spinal cord. This can cause pain, numbness, and weakness in the back and limbs.
There are several ways to do discectomy, each with its own benefits.
Open vs. Microdiscectomy Approaches
Open discectomy uses a big incision to reach the herniated disc. Microdiscectomy, on the other hand, is a small incision surgery. It uses a microscope for better view. Microdiscectomy causes less damage, less bleeding, and faster healing than open surgery.
Endoscopic Discectomy Innovations
Endoscopic discectomy is a new way to do spinal surgery. It uses a small endoscope and tools to remove the disc through tiny cuts. It causes less muscle damage, less pain, and quicker recovery than other methods.
Post-Operative Rehabilitation Protocol
After surgery, a careful recovery plan is key. It includes:
- Rest and pain control
- Slow start with physical therapy
- Exercises to strengthen the spine
- Learning good posture and body mechanics
By sticking to this plan, patients can see big improvements. Discectomy is a proven way to treat herniated and damaged discs, helping many people feel better and move more easily.
Artificial Disc Replacement: Preserving Spinal Motion
Spinal surgery has made big strides, leading to artificial disc replacement. This method keeps the spine moving. It replaces a damaged disc with a synthetic one, restoring height and movement between vertebrae.
Cervical and Lumbar Disc Replacement Options
Artificial disc replacement works for both the neck and lower back. Cervical disc replacement helps with neck pain from degenerative disc disease. Lumbar disc replacement is for lower back pain.
Ideal Candidates for the Procedure
Not everyone is right for artificial disc replacement. It’s best for those with severe disc problems that haven’t gotten better with other treatments. Doctors need to check with imaging studies to see if it’s a good fit.
Comparative Benefits Over Fusion
Artificial disc replacement has big advantages over spinal fusion. The main plus is keeping the spine moving. This can mean a more natural feel and fewer problems later on.
| Feature | Artificial Disc Replacement | Spinal Fusion |
|---|---|---|
| Motion Preservation | Yes | No |
| Recovery Time | Generally shorter | Variable, often longer |
| Adjacent Segment Disease Risk | Lower | Higher |
A study found that artificial disc replacement keeps the spine moving. It also lowers the risk of problems in other parts of the spine compared to fusion. This makes it a good choice for those wanting to keep their spine flexible.
Minimally Invasive Spine Surgery Techniques
Spinal surgery is changing towards less invasive methods. These new techniques promise faster healing and fewer side effects. They aim to reduce the harm of traditional surgery, making recovery smoother.
Tubular Retractor Systems
Tubular retractor systems are key in new spine surgery. They let surgeons work through small cuts, causing less damage. This leads to quicker healing.
Laser and Endoscopic Approaches
Laser and endoscopic methods are also vital. They allow for precise surgery through small openings. This cuts down on the need for big cuts, leading to less pain and faster healing.
Reduced Recovery Time and Complications
Minimally invasive surgery cuts down on recovery time and complications. It causes less damage and smaller cuts. This means less pain and quicker return to daily life.
| Technique | Benefits | Recovery Time |
|---|---|---|
| Tubular Retractor Systems | Less tissue damage, reduced post-operative pain | 2-4 weeks |
| Laser and Endoscopic Approaches | High precision, minimal tissue dissection | 1-3 weeks |
| Traditional Open Surgery | More invasive, higher risk of complications | 6-12 weeks |
The table shows the benefits of new spine surgery methods. They offer faster recovery and fewer risks. Choosing the right method means less pain, shorter hospital stays, and quicker return to life.
Vertebral Compression Fracture Treatments
Vertebral compression fractures can really hurt a person’s quality of life. It’s important to get the right treatment quickly. These fractures happen when a vertebra collapses, often because of osteoporosis or an injury. We’ll look at the main treatments, like kyphoplasty and vertebroplasty.
Kyphoplasty: Balloon-Assisted Vertebral Repair
Kyphoplasty is a small surgery that uses a balloon to make the vertebra bigger. Then, bone cement is injected to keep the vertebra stable.
- Benefits: It helps restore the vertebra’s height, reduces pain, and makes moving easier.
- Procedure: A balloon is put into the broken vertebra, inflated to make it taller, and then filled with bone cement.
Vertebroplasty: Cement Stabilization
Vertebroplasty is when bone cement is injected into the broken vertebra. This helps stabilize it and eases pain.
Key aspects:
- It quickly relieves pain
- It’s a minimally invasive procedure
- It stabilizes the vertebra
Patient Selection and Outcome Differences
Choosing between kyphoplasty and vertebroplasty depends on several things. These include how bad the fracture is, the patient’s health, and their symptoms.
Osteoporosis-Related Fractures
Both treatments work well for osteoporosis-related fractures. But, kyphoplasty might help more in making the vertebra taller.
Trauma-Induced Fractures
Trauma-induced fractures might need a different approach. Vertebroplasty might be better for some types of fractures.
It’s best to talk to a healthcare professional to figure out the best treatment.
Conclusion: Navigating Your Spinal Surgery Options
Understanding spinal surgery options is key. We’ve looked at different types of spinal surgery. This includes spinal fusion, laminectomy, discectomy, and artificial disc replacement.
It’s important to know when and why each surgery is used. This helps you make the right choice for your health. Lower back surgeries are often complex and need careful thought.
By exploring all your options, you can find the best treatment with your doctor. We aim to offer top-notch healthcare to international patients. We support those seeking advanced medical treatments.
FAQ
What are the most common types of spine surgery?
We offer many spinal surgeries. These include spinal fusion, laminectomy, discectomy, and artificial disc replacement. We also use minimally invasive techniques to treat different spinal issues.
What is the difference between decompression and stabilization surgeries?
Decompression surgeries, like laminectomy, relieve pressure on nerves. Stabilization surgeries, such as spinal fusion, connect vertebrae to stabilize the spine.
How do I know if I’m a candidate for spinal fusion surgery?
We assess each patient to see if spinal fusion is right for them. We look at the severity of spinal instability, disc degeneration, or fractures.
What is the recovery time for discectomy surgery?
Recovery from discectomy varies. Microdiscectomy and endoscopic discectomy usually have shorter recovery times than open discectomy.
What are the benefits of artificial disc replacement over spinal fusion?
Artificial disc replacement keeps the spine moving. This reduces the risk of further problems and promotes natural movement. Spinal fusion can make the spine stiffer and limit mobility.
Are minimally invasive spine surgery techniques effective?
Yes, minimally invasive techniques are effective. They reduce recovery time, lower complication risks, and lead to good outcomes.
What is the difference between kyphoplasty and vertebroplasty?
Kyphoplasty uses a balloon to restore height before cement is injected. Vertebroplasty injects cement directly into a fractured vertebra to stabilize it.
How do I choose the right spinal surgeon for my procedure?
Choose a spinal surgeon based on their experience and success with your procedure. Also, consider their ability to provide full care and support during treatment.
What are the possible complications of spinal surgery?
Spinal surgery carries risks like infection, nerve damage, and bleeding. We discuss these risks with patients before surgery.
How long does it take to recover from spinal surgery?
Recovery times vary by surgery type. Some may need weeks or months of rehabilitation. We guide each patient on post-operative care and rehabilitation for a smooth recovery.