Last Updated on November 27, 2025 by Bilal Hasdemir

Aortic valve thickening makes the valve thicker, blocking blood flow from the heart. This can lead to aortic stenosis, a serious narrowing of the valve. Facing severe aortic stenosis can change your life, but there are advanced treatment options to help you live better.
The main cause of aortic stenosis is age-related calcification and congenital issues. At Liv Hospital, our team is committed to top-notch healthcare and support. We’ll look at the best treatment options for severe heart stenosis, like medicines and surgery.
Key Takeaways
- Understanding the causes and symptoms of aortic stenosis is key for managing it well.
- There are advanced treatment options for severe aortic stenosis.
- Liv Hospital offers full care with a team of dedicated experts.
- Treatment plans are made just for each patient.
- With the right treatment, you can improve your quality of life.
Understanding Aortic Valve Thickening and Stenosis
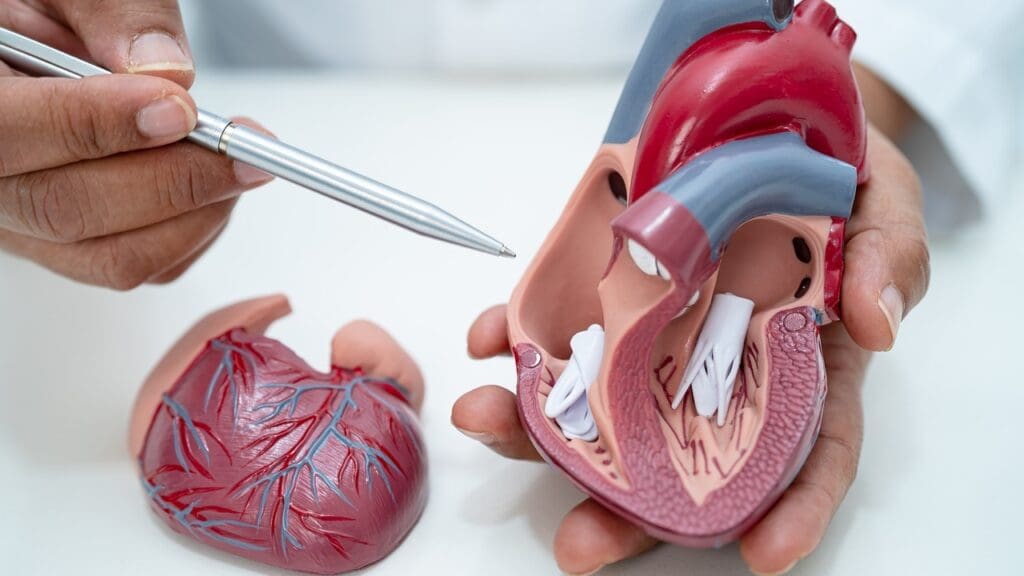
It’s important to know how the aortic valve works to understand thickening and stenosis. The aortic valve controls blood flow from the heart to the body. Any problems with it can cause serious health issues.
Anatomy of the Aortic Valve
The aortic valve has three cusps that open to let blood flow into the aorta. Proper valve function is key for good blood circulation. The valve’s design ensures blood flows only one way, preventing it from going back to the heart.
The Progression from Thickening to Stenosis
Thickening of the aortic valve often happens due to age-related calcification. Calcium builds up on the valve cusps, making them stiff and thick. This can lead to aortic stenosis, where the valve opening narrows, blocking blood flow.
Impact on Heart Function and Blood Flow
Aortic stenosis makes the heart work harder, increasing the left ventricle’s workload. As stenosis gets worse, the heart must pump blood harder through the narrowed valve. This can lead to heart failure if not treated. Reduced blood flow can cause chest pain, shortness of breath, and fatigue.
Common Causes of Aortic Valve Thickening

Aortic valve thickening can come from many sources. Understanding these causes is key to managing the condition. We will look at the different factors that lead to this issue. This will help doctors create better treatment plans.
Age-Related Calcification
Age is a big risk for aortic valve thickening. As we get older, our valves can become calcified. This can make the valve thicker and may lead to stenosis. This problem is linked to aging and can get worse with other heart risks.
Congenital Abnormalities
Some people are born with heart issues that raise the risk of valve thickening. For example, a bicuspid aortic valve has only two cusps instead of three. This can cause problems with the valve over time.
Bicuspid Aortic Valve
A bicuspid aortic valve is a common heart defect at birth. It can cause the valve to thicken. People with this condition need regular checks to see if they need treatment.
Other Congenital Valve Defects
Other heart defects at birth can also cause valve thickening. These defects can affect how the valve works. Each case needs a special plan for treatment.
Rheumatic Heart Disease
Rheumatic heart disease is another reason for valve thickening. It’s more common in areas where rheumatic fever is common. This disease damages the valve and can make it thicker.
Other Contributing Factors
High blood pressure and high cholesterol can also make the valve thicker. It’s important to manage these conditions to prevent more damage.
| Cause | Description | Impact on Valve |
|---|---|---|
| Age-Related Calcification | Calcific changes due to aging | Thickening and possible stenosis |
| Congenital Abnormalities | Structural defects, e.g., bicuspid aortic valve | Higher risk of thickening and dysfunction |
| Rheumatic Heart Disease | Valve damage from rheumatic fever | Thickening and possible stenosis |
Diagnosing Aortic Valve Thickening and Stenosis
To diagnose aortic valve thickening and stenosis, doctors use physical exams, imaging, and lab tests. Getting the diagnosis right is key to managing the condition well.
Physical Examination Findings
A detailed physical exam is vital for spotting aortic valve issues. Doctors listen for a systolic ejection murmur, which hints at stenosis.
Diagnostic Imaging Techniques
Imaging is a big help in finding aortic valve problems. Echocardiography is a top choice, giving clear views of valve function and how severe the stenosis is.
Echocardiography
Echocardiography checks the valve’s shape, including any thickening or calcification. It also looks at the valve area and how well the left ventricle is working.
Cardiac CT and MRI
Cardiac CT and MRI offer more details on the valve’s structure and how it works. They help figure out how bad the stenosis is and what treatment might be best.
Laboratory Tests
Labs can run tests like blood biomarkers to help confirm the diagnosis. These tests aren’t the final word but can spot patients at risk.
Cardiac Catheterization
Cardiac catheterization is a more invasive test that looks at how the valve works. It’s often used when considering treatment options.
“The accurate diagnosis of aortic valve stenosis is critical for guiding appropriate treatment and improving patient outcomes.”
Grading the Severity of Aortic Stenosis
Doctors need to grade aortic stenosis to plan the best treatment. They look at the valve area, mean gradient, and peak velocity to decide.
Mild Aortic Valve Stenosis
Mild aortic valve stenosis means the valve area is over 1.5 cm and the mean gradient is under 20 mmHg. At this point, many patients don’t show symptoms. They usually just need regular check-ups.
Moderate Aortic Stenosis
For moderate aortic stenosis, the valve area is between 1.0 and 1.5 cm, and the mean gradient is 20-40 mmHg. Symptoms might start to show up. So, doctors need to keep a closer eye on these patients.
Severe Aortic Stenosis
Severe aortic stenosis is when the valve area is under 1.0 cm and the mean gradient is over 40 mmHg. People with symptomatic severe aortic stenosis often need treatment right away. Symptoms can really hurt their quality of life.
Critical Aortic Stenosis
Critical aortic stenosis is a very advanced stage. The valve area is very small, and the mean gradient is extremely high. This situation requires quick medical action and often urgent treatment.
Knowing these levels helps doctors create the right treatment plan for each patient. This way, they can improve outcomes for aortic stenosis management.
Recognizing Symptoms of Progressive Aortic Stenosis
As aortic stenosis gets worse, it’s key to spot its signs early. This condition narrows the aortic valve opening. It blocks blood flow from the heart to the body.
Asymptomatic Phase
At first, many with aortic stenosis don’t show symptoms. They might only find out during regular check-ups.
Early Warning Signs
As it gets worse, you might start to feel tired, out of breath when active, or have irregular heartbeats.
Classic Symptomatic Triad
The main symptoms are angina (chest pain), syncope (fainting), and dyspnea (shortness of breath). These signs mean the disease is getting serious.
Angina (Chest Pain)
Angina happens when the heart muscle doesn’t get enough blood. It usually happens when you’re active and goes away when you rest.
Syncope (Fainting)
Syncope in aortic stenosis can be due to not being able to pump enough blood when active or from irregular heartbeats.
Dyspnea (Shortness of Breath)
Dyspnea shows the heart is failing to meet the body’s needs. It’s a sign of heart failure.
Complications of Untreated Severe Stenosis
Severe aortic stenosis without treatment can cause heart failure and dangerous heart rhythms.
Doctors stress that catching aortic stenosis early can greatly improve treatment results. Spotting its symptoms is the first step to managing and treating it.
Aortic Valve Thickening Treatment: Medical Management Approaches
Medical management is key in treating aortic valve thickening and stenosis. It aims to ease symptoms and slow disease growth through various treatments.
Medication Options for Symptom Control
Several medications help manage symptoms of aortic stenosis. These include:
Beta Blockers
Beta blockers lower the heart’s workload. They slow the heart rate and reduce contraction force. This helps ease chest pain and shortness of breath.
Diuretics
Diuretics help manage fluid overload. They reduce symptoms like edema and dyspnea.
ACE Inhibitors and ARBs
ACE inhibitors and ARBs manage high blood pressure. They reduce heart strain. But, their use in severe aortic stenosis is cautious due to the risk of low blood pressure.
Anticoagulation Therapy
Anticoagulation therapy is key for those with atrial fibrillation or mechanical valve prostheses. It prevents blood clots.
Statins and Lipid Management
Statins help manage cholesterol levels. They may slow aortic stenosis progression. But, research on their effectiveness is ongoing.
Limitations of Medical Therapy
Medical management is vital but has its limits. Severe aortic stenosis often needs more than just medication. It may require valve replacement or repair.
Balloon Valvuloplasty: Procedure and Outcomes
For those with severe aortic stenosis, balloon valvuloplasty is a less invasive treatment. It uses a balloon catheter to widen the aortic valve. This improves blood flow from the heart.
Candidate Selection for Valvuloplasty
We choose who gets balloon valvuloplasty carefully. We look at how severe their aortic stenosis is, their overall health, and if they can handle surgery. This procedure is for those who can’t have surgery because of health issues.
Procedural Technique
The procedure starts by accessing the heart through a large artery in the groin. A balloon catheter is then guided to the aortic valve. The balloon is inflated to widen the valve, improving blood flow. This technique needs precise imaging and skilled operators.
Recovery and Aftercare
After the procedure, patients are watched closely for any problems. They usually stay in the hospital for a short time. We manage symptoms and watch for issues like bleeding or valve rupture. After leaving the hospital, they get advice on care, including medication and follow-up visits.
Long-term Results and Limitations
While balloon valvuloplasty can help symptoms, it has limits. Valve restenosis can happen over time. We talk about this with patients and plan their care based on this risk. Below is a summary of balloon valvuloplasty.
| Aspect | Description | Outcome |
|---|---|---|
| Candidate Selection | Patients with severe aortic stenosis not suitable for surgery | Improved symptom management |
| Procedural Technique | Balloon catheter dilation of the aortic valve | Increased valve opening |
| Recovery and Aftercare | Monitoring for complications and post-procedure care | Reduced risk of immediate complications |
| Long-term Results | Limited by the risk of valve restenosis | Temporary symptom relief |
In conclusion, balloon valvuloplasty is a good option for some patients with severe aortic stenosis. We see it as part of a complete care plan, made just for each patient.
Surgical Valve Repair Techniques
Surgical valve repair is a good option for those with aortic valve disease. It uses different techniques to fix the valve. We tackle the complex issues of aortic valve problems with various methods.
Commissurotomy
Commissurotomy is a surgery for fused or stenotic valve leaflets. We cut the commissures to make the leaflets move better. This helps the valve work right again, which is great for those with valve stenosis.
Decalcification Procedures
Decalcification removes calcium from the valve leaflets. We use special methods to clean out the calcium. This makes the leaflets more flexible and reduces stenosis, helping those with calcified valves.
Aortic Root Remodeling
Aortic root remodeling reshapes the aortic root to improve valve function. It’s often used with other repair methods. This way, we can make the valve work better and lower the risk of future problems.
Recovery Timeline and Rehabilitation
The time it takes to recover from valve repair surgery varies. Patients usually stay in the hospital for a few days. Then, they start a rehabilitation period. We stress the importance of proper care and rehab for the best recovery and long-term health.
Long-term Outcomes and Survival Rates
Most patients see big improvements after valve repair surgery. Studies show it can lead to better survival rates and fewer heart problems later on. We keep a close eye on our patients to ensure they get the best long-term results.
Valve Replacement Options
Valve replacement is a key treatment for severe aortic stenosis. It aims to restore normal heart function. Several factors are important, like the type of prosthetic valve and the surgical method.
Mechanical Valve Prostheses
Mechanical valves are made from materials like titanium and carbon. They last long but need lifelong blood thinner therapy to avoid clots.
Types and Materials
There are different mechanical valve designs, like bileaflet and tilting disk valves. The material and design impact the valve’s performance and durability.
Advantages and Disadvantages
Mechanical valves are durable. But, they require lifelong blood thinners, which is a big drawback for some.
Anticoagulation Requirements
People with mechanical valves must take blood thinners to prevent clots. They need regular checks to make sure the dose is right.
Biological Valve Prostheses
Biological valves are made from animal tissue, like porcine or bovine. They are less likely to cause clots and often don’t need long-term blood thinners.
Tissue Types and Sources
Biological valves can be made from porcine or bovine tissue. The type of tissue used affects the valve’s durability and how well it works.
Durability and Lifespan
Biological valves usually need to be replaced after 10 to 15 years. But, they are less likely to cause clotting problems.
Ideal Candidates
Biological valves are often suggested for older patients or those who can’t handle long-term blood thinners.
Surgical Approach Considerations
The surgical method for valve replacement varies. The choice between open surgery and minimally invasive techniques depends on the patient’s health and the surgeon’s skills.
Traditional Open Surgery
Open surgery involves a bigger chest incision. It gives the surgeon a clear view of the area.
Minimally Invasive Techniques
Minimally invasive surgery uses smaller cuts and may lead to faster recovery. But, it needs special skills and tools.
| Valve Type | Durability | Anticoagulation Requirements |
|---|---|---|
| Mechanical | High | Lifelong |
| Biological | Moderate (10-15 years) | Short-term or none |
Transcatheter Aortic Valve Implantation (TAVI)
TAVI is a new way to treat severe aortic stenosis without surgery. It’s less invasive than traditional surgery. This method has shown to improve patient outcomes and reduce recovery time.
Advancements in TAVI Technology
TAVI technology has made big strides. Improved device designs and delivery systems have made the procedure safer and more effective. Newer valves can be repositioned and last longer.
Patient Selection Criteria
Choosing the right patient for TAVI is key. We look at the patient’s health, the severity of aortic stenosis, and any other health issues. Multidisciplinary heart teams help decide if TAVI is right for each patient.
Procedural Techniques
TAVI can be done in different ways. The most common is the transfemoral approach, which goes through the femoral artery in the leg.
Transfemoral Approach
The transfemoral approach is the most common and considered the best. It’s less invasive and leads to quicker recovery. We use advanced imaging to guide the procedure and place the valve correctly.
Alternative Access Routes
If the transfemoral approach isn’t possible, we might use other routes. These include the transapical or transaortic approaches. Each requires careful planning to ensure the best results.
Complications and Management
While TAVI is safe, complications can happen. We watch for vascular injury, stroke, or paravalvular leak. Prompt management of these issues is critical to minimize their effects.
Comparing TAVI to Surgical Replacement
Studies have compared TAVI to surgical valve replacement. TAVI is as effective as surgery for high-risk patients but is less invasive. The choice between TAVI and surgery depends on the patient’s situation and preferences.
Recent Innovations and Future Directions
The field of TAVI is always evolving. Ongoing research aims to improve device technology and expand who can get TAVI. We expect future advancements to make TAVI even safer and more effective for more patients.
Conclusion: Optimizing Treatment Decisions for Aortic Valve Disease
Improving treatment choices is key to better patient care in aortic valve disease. We’ve looked at many treatment paths, like medical care, balloon valvuloplasty, and surgery. Knowing a lot about the disease and its treatments is vital for the best care.
When picking treatments, we look at how severe the disease is, the patient’s symptoms, and their health. Understanding the disease and treatments helps us make choices that help patients. Making these decisions needs a team effort, with doctors, surgeons, and other experts.
By making better treatment choices, we can make life better for those with aortic valve disease. We focus on treating each patient as an individual, considering their unique needs. Our aim is to offer top-notch care to patients from around the world who need advanced treatments.
FAQ
What is aortic valve thickening, and how does it lead to stenosis?
Aortic valve thickening makes the valve thicker, blocking blood flow. This can turn into aortic stenosis, a severe narrowing of the valve.
What are the common causes of aortic valve thickening?
Aortic valve thickening can be caused by age, congenital issues, or rheumatic heart disease. High blood pressure and high cholesterol also play a role.
How is aortic stenosis diagnosed?
Doctors use physical exams, imaging, lab tests, and cardiac catheterization to diagnose aortic stenosis. Echocardiography is key.
What are the symptoms of progressive aortic stenosis?
Symptoms include chest pain, fainting, and shortness of breath. If not treated, it can lead to heart failure and irregular heartbeats.
What are the treatment options for aortic valve thickening and stenosis?
Treatments include medication, balloon valvuloplasty, and surgery. The best option depends on the condition’s severity and the patient’s needs.
What is balloon valvuloplasty, and when is it used?
Balloon valvuloplasty uses a balloon to widen the valve. It’s used in certain cases, like in younger patients or those with specific valve types.
What is the difference between mechanical and biological valve prostheses?
Mechanical valves last longer but need lifelong blood thinners. Biological valves don’t need blood thinners but last less long. The choice depends on the patient’s health.
What is Transcatheter Aortic Valve Implantation (TAVI), and who is it for?
TAVI is a minimally invasive procedure for new valve implantation. It’s for those at high risk for surgery or with specific anatomical features.
Can aortic stenosis cause heart failure?
Yes, severe aortic stenosis can cause heart failure. This is because the heart works harder to pump blood.
What is the significance of grading the severity of aortic stenosis?
Grading aortic stenosis severity is key for choosing the right treatment. It’s based on valve area, mean gradient, and peak velocity.
How does aortic valve thickening affect heart function and blood flow?
Thickening restricts blood flow, increasing heart pressure and workload. Untreated, it can lead to heart failure.
References
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC5566726
- AHA Journals (Circulation Research) : https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.121.318040
- American Heart Association (Options for Heart Valve Replacement) : https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/understanding-your-heart-valve-treatment-options/options-for-heart-valve-replacement