Last Updated on November 27, 2025 by Bilal Hasdemir
Getting a brain tumor diagnosis can be scary. But, it’s important to know that most meningiomas are benign and can be treated. Removing meningiomas is a common treatment when they cause problems or press on important areas.
At Liv Hospital, we provide world-class healthcare for international patients. Our team focuses on safe, patient-centered care at the highest standards. Knowing your treatment options is key for meningioma surgery success.
Key Takeaways
- Most meningiomas are benign and treatable.
- Meningioma removal is a key treatment procedure.
- Surgery is often successful for benign meningioma.
- Understanding treatment options is vital for patients.
- Liv Hospital offers complete care for international patients.
What Are Meningiomas? Understanding the Basics

Meningiomas are tumors that grow from the meninges. These are protective layers around the brain and spinal cord. Understanding meningiomas starts with knowing their basic traits and how they form.
Definition and Formation of Meningiomas
Meningiomas come from the meningeal layers that cover the central nervous system. Johns Hopkins says these tumors grow slowly and are usually benign. They form when cells in the meninges grow abnormally.
The exact reason for meningioma growth is not known. But, genetics are thought to play a big part. Meningioma definition includes their origin from meningeal tissue. This is key to understanding their behavior and treatment.
Benign vs. Malignant Meningiomas: What’s the Difference?
Meningiomas are mainly divided into benign and malignant types. Benign meningiomas make up about 90% of cases. They grow slowly and are not cancerous.
Malignant meningiomas are rare and aggressive. They can spread to nearby brain tissue and come back after treatment. Knowing the difference is important for choosing the right treatment.
Being diagnosed with meningioma can be scary. But, knowing the details of your condition helps in making treatment choices. It also gives a clearer idea of what to expect.
Essential Fact #1: Most Meningiomas Are Benign with High Survival Rates
Most meningiomas are benign, which is good news for many patients. This fact is key to understanding the prognosis and treatment options for those with meningiomas.
Grade I Meningiomas and Their Prognosis
Grade I meningiomas make up about 75% of all meningioma cases, as UCLA Health notes. These tumors grow slowly and are benign, leading to a good prognosis. Patients with Grade I meningiomas often have a high chance of successful treatment and long-term survival.
Key characteristics of Grade I meningiomas include:
- Slow growth rate
- Benign nature
- High success rate with appropriate treatment
Five-Year Survival Rates Exceeding 90%
The five-year survival rate for patients with benign meningiomas, like Grade I tumors, is over 90%. This shows the positive outlook for these tumors. Studies point to the benign nature and medical treatment improvements as reasons for the high survival rate.
Factors contributing to high survival rates include:
- Early detection and diagnosis
- Effective surgical interventions
- Advancements in radiation therapy
Understanding these statistics can offer comfort and guidance to patients. By focusing on the benign nature of most meningiomas and their high survival rates, we aim to give patients knowledge and hope.
Essential Fact #2: Meningioma Removal Is Often Necessary When Symptoms Appear
Symptoms of meningioma often mean surgery is needed. When symptoms show up, it’s key to get tests to confirm the meningioma. Then, doctors can figure out the best treatment.
Recognizing Symptoms That Require Intervention
Meningiomas can cause different symptoms based on where they are. The Cleveland Clinic says headaches, nausea, and vomiting are common. Vision problems can happen if the tumor is near the optic nerve.
Spotting these symptoms early is very important. It lets doctors act fast. For example, if a meningioma is pressing on a brain area, surgery might be needed. This helps relieve pressure and prevent more harm.
Diagnostic Procedures to Confirm Meningioma
To confirm a meningioma, doctors use several tests. MRI and CT scans help see the tumor and its size. Sometimes, a biopsy is done to check if the meningioma is cancerous.
A study in the academic repository says accurate diagnosis is vital. “The diagnosis of meningioma is typically made through a combination of imaging studies and clinical evaluation,” it notes. This shows the need for a detailed diagnostic process.
By knowing the symptoms and getting the right tests, patients can get the best treatment for meningioma.
Essential Fact #3: Surgical Success Rates Are Remarkably High
Surgical success rates for removing meningiomas are very high. This gives hope to patients all over the world. Surgery for meningiomas has improved a lot. Now, doctors aim to remove the tumor completely while keeping risks low.
Studies show that total removal rates change with age. Elderly patients see success rates up to 84.5%, while younger ones see rates around 76.2%. These numbers show how good modern surgery is. They also highlight the need for skilled neurosurgeons.
Total Resection Rates in Different Age Groups
The success of meningioma surgery depends on several things, including the patient’s age. A study on meningioma surgery outcomes found that total removal rates vary between the elderly and the young.
| Age Group | Total Resection Rate |
|---|---|
| Elderly Patients | Up to 84.5% |
| Younger Patients | Around 76.2% |
These numbers show that both age groups have high success rates. But, there’s a clear difference in total removal rates between them.
Factors That Influence Surgical Outcomes
Many things affect the success of meningioma surgery. The neurosurgeon’s skill and experience are key. So is the use of new surgical methods and technology.
“The outcome of meningioma surgery is significantly influenced by the surgeon’s expertise and the use of modern neurosurgical techniques.”
Other important factors include the tumor’s location, size, and grade. The patient’s health and age also play a role.
Understanding these factors and using new neurosurgery techniques helps doctors give patients the best results. The high success rates of meningioma surgery show how far this field has come.
Essential Fact #4: Location Determines Surgical Approach and Complexity
The place where a meningioma grows affects how it’s treated. The brain’s layout is complex. Tumors can grow in many spots, each with its own set of challenges for doctors.
Experts at Johns Hopkins say the meningioma’s location is key. Tumors in places like behind the eye are tricky. This means each case needs a special plan, making experience and personal care vital.
Frontal Lobe Meningioma Surgery Techniques
Frontal lobe meningiomas are common. Surgery often means removing a part of the skull, called a craniotomy. The method depends on the tumor’s size and where it is in the frontal lobe.
Doctors use intraoperative MRI for precise removal. They aim to remove the tumor completely while keeping the brain safe. This reduces the risk of brain damage.
Surgical Approaches for Meningiomas Behind the Eye
Meningiomas behind the eye, or orbital meningiomas, are special challenges. They can cause vision problems and make the eye bulge. A team of doctors, including neurosurgeons and eye specialists, works together for these cases.
The surgery might involve opening the eye socket, called a combined orbitotomy. This careful approach helps avoid harming the eye’s delicate parts.
Sphenoid Wing Meningioma Treatment Challenges
Sphenoid wing meningiomas are hard to treat because of their location. They’re near important blood vessels and the cavernous sinus. The surgery needs great skill and precision.
One big challenge is removing the tumor without harming nearby important structures. Sometimes, doctors use stereotactic radiosurgery for parts of the tumor that can’t be removed surgically.
| Meningioma Location | Surgical Challenges | Common Surgical Techniques |
|---|---|---|
| Frontal Lobe | Accessing the tumor without damaging frontal lobe structures | Craniotomy, Intraoperative MRI |
| Behind the Eye (Orbital) | Preserving vision and eye movement | Combined Orbitotomy |
| Sphenoid Wing | Avoiding damage to cavernous sinus and major blood vessels | Stereotactic Radiosurgery, Microsurgical Techniques |
A study in a top neurosurgery journal says understanding the tumor’s location is key. It shows the need for custom treatment plans and skilled neurosurgeons in handling these complex cases.
Essential Fact #5: Radiation Therapy Offers Non-Surgical Treatment Options
Radiation therapy is a key treatment for meningiomas, giving patients a non-surgical choice. Not everyone can have surgery because of where the tumor is, its size, or their health. In these cases, radiation therapy is a good option.
Types of Radiation Treatment for Meningiomas
There are different types of radiation therapy for meningiomas, each with its own use and benefits. The main types are:
- Stereotactic Radiosurgery (SRS): This is a precise radiation therapy that gives a big dose of radiation in one session. SRS works well for small to medium-sized meningiomas.
- Fractionated Radiation Therapy: This method gives radiation in many sessions. It lets you get a higher dose while protecting healthy tissue. It’s used for bigger tumors or those in sensitive spots.
- Intensity-Modulated Radiation Therapy (IMRT): IMRT is a type of fractionated radiation therapy. It targets the tumor with different levels of radiation. This helps protect more of the healthy tissue around it.
When Radiation Is Preferred Over Surgery
Radiation therapy is often chosen over surgery in certain situations:
- Tumor Location: For meningiomas in hard-to-reach or critical areas, radiation therapy is safer than surgery.
- Patient Health: People with serious health problems that make surgery risky might do better with radiation therapy.
- Residual Tumor: If some tumor stays after surgery, radiation therapy can treat it.
UCLA Health says radiation therapy is great for those who can’t have surgery or have leftover tumor tissue. Our team helps decide the best treatment plan for each patient based on their situation.
Essential Fact #6: Surgery for Non-Cancerous Meningioma Often Restores Quality of Life
Surgery to remove non-cancerous meningiomas greatly improves patients’ lives. After the surgery, patients often see big changes in their symptoms and overall health.
Functional Improvements After Successful Surgery
Many patients see big improvements after surgery for non-cancerous meningioma. They might notice better thinking skills, fewer seizures, and stronger muscles. How much they improve depends on the tumor’s size and location, and their health.
For example, if a meningioma is near important brain areas, patients might feel much better. They could stop having headaches, vision problems, or weakness in their limbs. Surgery can make these symptoms go away, helping patients get back to normal.
Patient Stories and Outcomes
Real-life stories show how surgery can change lives. A patient with a big meningioma near the optic nerve saw their vision improve a lot after surgery. Another patient, who had seizures because of a meningioma, stopped having seizures after the tumor was removed.
These stories show why it’s key to have good care and support during treatment. With the right medical help and rehab, patients can get their lives back on track and feel better.
Essential Fact #7: Recovery Timeline and Expectations
Knowing how to recover after meningioma surgery is key for patients. It helps them know what to expect and plan for their care after surgery. The time it takes to recover can differ based on the person and the surgery’s complexity, as experts at Johns Hopkins say.
Immediate Post-Operative Recovery
The recovery right after surgery can last from a few days to weeks. During this time, patients are watched closely for any problems. They also get pain medicine as needed. It’s important for healthcare teams to keep a close eye on patients to catch any issues early.
Patients might stay in the ICU or a regular room for a few days. They may feel tired, have headaches, or other symptoms. These are managed with medical care.
Long-term Rehabilitation Process
After the first recovery, patients start a long-term rehab to get stronger and think clearer. This can take weeks to months. They do physical, occupational, and sometimes speech therapy, based on the surgery.
Rehab is a big part of getting better. It helps patients become independent again and live better lives. The rehab team makes therapy plans that fit each patient’s needs.
Returning to Normal Activities
How long it takes to get back to normal varies a lot. It depends on the patient’s health, the surgery’s extent, and if there were any complications.
Patients are told to start with simple tasks and then do more. It’s important to keep up with follow-up care to check on progress and solve any problems.
By knowing what to expect, patients can prepare for their recovery. With the right care and support, many can fully recover and get back to their lives.
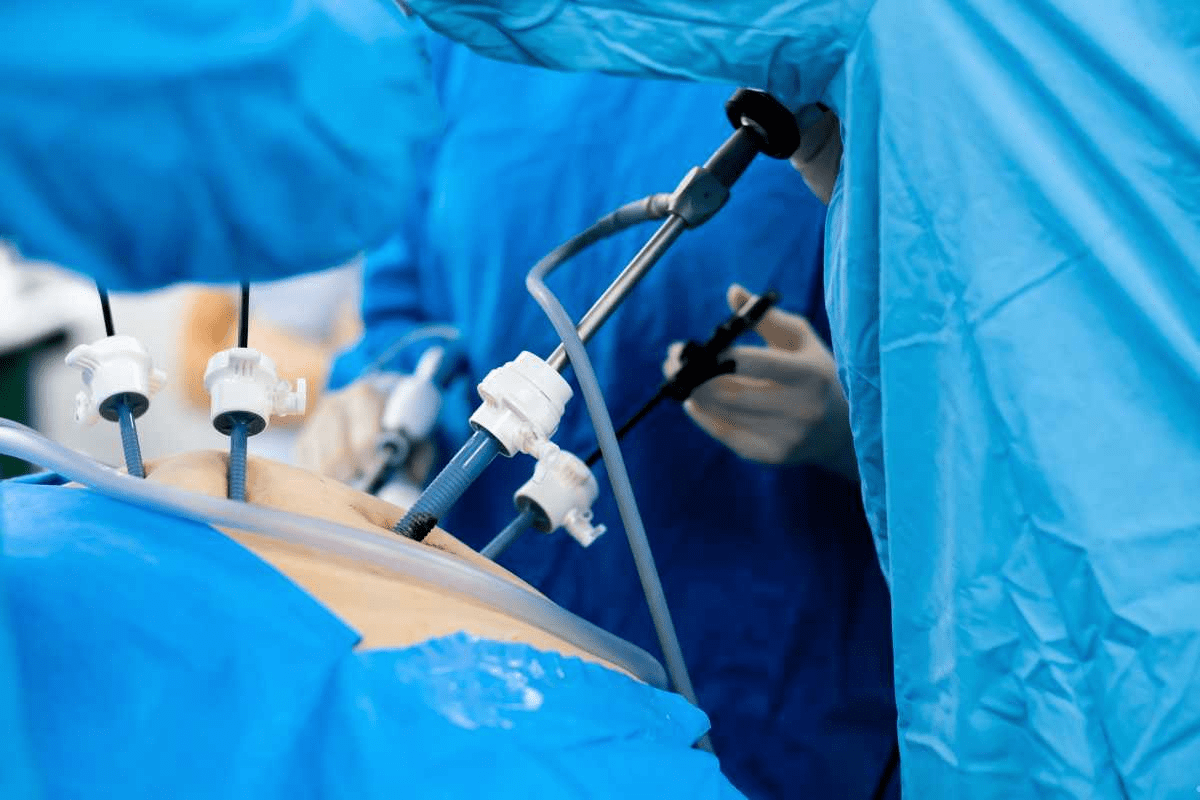
Advanced Surgical Techniques for Meningioma Removal
Advanced surgical techniques are changing how we treat meningiomas. UCLA Health says these new methods, like minimally invasive surgery and tech innovations, have made treatments better. Now, neurosurgery focuses on being precise, safe, and effective.
Minimally Invasive Approaches
Minimally invasive surgery is making a big difference in neurosurgery. It uses smaller cuts, less damage, and quicker healing. “The use of minimally invasive techniques in meningioma surgery has been associated with fewer complications and improved patient outcomes,” showing better lives for patients after surgery.
Technological Innovations in Neurosurgery
New tech is making surgery more precise and safe. Tools like intraoperative MRI, neuro-navigation systems, and advanced imaging help surgeons. These tools help save more brain tissue and lead to better results.
Key technological innovations include:
- Intraoperative MRI for real-time imaging
- Neuro-navigation systems for precise tumor localization
- Advanced imaging techniques for enhanced visualization
The use of advanced techniques, like minimally invasive surgery and new tech, is a big step forward. As neurosurgery keeps improving, we’ll see even better care and results for patients.
Alternative and Complementary Treatment Approaches
Meningioma treatment has grown, giving patients new options beyond surgery. Medical research keeps improving, giving patients more ways to manage their condition.
Not all meningiomas need immediate treatment. Some patients find alternative methods work better than traditional treatments.
Watchful Waiting for Asymptomatic Meningiomas
For those with no symptoms, watchful waiting is a good choice. It means keeping an eye on the tumor without rushing into surgery. Johns Hopkins Medicine suggests this for small, harmless meningiomas.
Watchful waiting has its perks:
- It avoids the risks of surgery
- It delays treatment if not needed
- It watches for any tumor changes
But, it needs regular check-ups and scans to catch any growth or symptoms.
Emerging Therapies and Clinical Trials
New treatments and clinical trials offer hope for meningioma patients. These new methods aim to better treatment results and improve life quality.
Some new therapies being looked into are:
- Targeted treatments that attack specific cancer cells
- Immunotherapies that use the body’s immune system
- Advanced radiation that spares healthy tissue
Clinical trials test these new treatments. Patients should talk to their doctors about the benefits and risks of joining a trial.
Keeping up with meningioma treatment news helps patients make better choices. Alternative treatments offer more options than just surgery, helping manage meningiomas in new ways.
Conclusion: Making Informed Decisions About Your Meningioma Treatment
Understanding meningioma removal, surgery, and treatment options is key for patients. We’ve looked at the important facts about meningiomas. This includes their benign nature and the need for timely treatment.
The Cleveland Clinic stresses the importance of a personalized treatment plan. Patients should know about surgery, radiation therapy, and other options. This ensures they get the best care.
By making informed decisions, patients can actively participate in their recovery. We urge patients to talk to their healthcare provider about treatment options. This helps find the most effective treatment for their needs.
FAQ
What is a meningioma, and is it cancerous?
A meningioma is a tumor in the meninges, which protect the brain and spinal cord. Most are benign, meaning they are not cancerous and grow slowly.
What are the symptoms of a meningioma that require medical attention?
Signs that need medical help include headaches, seizures, vision issues, and weakness or numbness in the arms or legs. If you notice these, see a doctor right away.
How is a meningioma diagnosed?
Diagnosis often uses MRI or CT scans. Sometimes, a biopsy is needed to confirm the tumor’s presence.
What is the success rate of meningioma surgery?
Surgery for meningiomas usually works well. The success rate depends on the tumor’s location and age. Skilled neurosurgeons and modern techniques help achieve good results.
How does the location of a meningioma affect surgical approach and complexity?
The tumor’s location affects the surgery’s approach and difficulty. For example, tumors in the frontal lobe or behind the eye need special techniques.
What are the treatment options for meningiomas?
Treatment options include surgery, radiation, or watching the tumor if it’s not causing symptoms. The choice depends on the tumor’s size, location, and type, and the patient’s health.
What is radiation therapy for meningiomas, and when is it preferred over surgery?
Radiation therapy is a non-surgical option for meningiomas. It’s often chosen for patients who can’t have surgery or have tumors that are hard to remove.
Can meningioma surgery restore quality of life?
Yes, surgery for non-cancerous meningiomas can improve quality of life. Patients often see functional gains and can return to their usual activities.
What is the recovery timeline for meningioma surgery?
The recovery time varies based on the surgery’s complexity and the individual. Patients usually have an immediate recovery period, followed by rehabilitation, and then return to normal activities.
Are there alternative and complementary treatment approaches for meningiomas?
Yes, options include watching the tumor if it’s not causing symptoms and new therapies like clinical trials. Personalized plans and ongoing research are key for the best care.
What are the latest advancements in surgical techniques for meningioma removal?
New advancements include minimally invasive methods and tech innovations in neurosurgery. These improve outcomes and reduce recovery time.
Are meningiomas benign?
Most meningiomas are benign, but some can be malignant. Proper diagnosis and treatment are vital to determine the best course of action.
What is the role of radiation for meningioma treatment?
Radiation therapy is important for meningioma treatment, mainly for patients who can’t have surgery or have tumors that are hard to remove.
Can sphenoid wing meningioma be treated effectively?
Yes, sphenoid wing meningioma can be treated with surgery and radiation. The treatment depends on the tumor’s size, location, and type, and the patient’s health.
Reference:
https://www.e-neurospine.org/journal/view.php?number=1248
https://braintumourresearch.org/pages/types-of-brain-tumours-meningioma
https://pmc.ncbi.nlm.nih.gov/articles/PMC8484216
https://pmc.ncbi.nlm.nih.gov/articles/PMC7735868
FAQ
What is a meningioma, and is it cancerous?
A meningioma is a tumor in the meninges, which protect the brain and spinal cord. Most are benign, meaning they are not cancerous and grow slowly.
What are the symptoms of a meningioma that require medical attention?
Signs that need medical help include headaches, seizures, vision issues, and weakness or numbness in the arms or legs. If you notice these, see a doctor right away.
How is a meningioma diagnosed?
Diagnosis often uses MRI or CT scans. Sometimes, a biopsy is needed to confirm the tumor’s presence.
What is the success rate of meningioma surgery?
Surgery for meningiomas usually works well. The success rate depends on the tumor’s location and age. Skilled neurosurgeons and modern techniques help achieve good results.
How does the location of a meningioma affect surgical approach and complexity?
The tumor’s location affects the surgery’s approach and difficulty. For example, tumors in the frontal lobe or behind the eye need special techniques.
What are the treatment options for meningiomas?
Treatment options include surgery, radiation, or watching the tumor if it’s not causing symptoms. The choice depends on the tumor’s size, location, and type, and the patient’s health.
What is radiation therapy for meningiomas, and when is it preferred over surgery?
Radiation therapy is a non-surgical option for meningiomas. It’s often chosen for patients who can’t have surgery or have tumors that are hard to remove.
Can meningioma surgery restore quality of life?
Yes, surgery for non-cancerous meningiomas can improve quality of life. Patients often see functional gains and can return to their usual activities.
What is the recovery timeline for meningioma surgery?
The recovery time varies based on the surgery’s complexity and the individual. Patients usually have an immediate recovery period, followed by rehabilitation, and then return to normal activities.
Are there alternative and complementary treatment approaches for meningiomas?
Yes, options include watching the tumor if it’s not causing symptoms and new therapies like clinical trials. Personalized plans and ongoing research are key for the best care.
What are the latest advancements in surgical techniques for meningioma removal?
New advancements include minimally invasive methods and tech innovations in neurosurgery. These improve outcomes and reduce recovery time.
Are meningiomas benign?
Most meningiomas are benign, but some can be malignant. Proper diagnosis and treatment are vital to determine the best course of action.
What is the role of radiation for meningioma treatment?
Radiation therapy is important for meningioma treatment, mainly for patients who can’t have surgery or have tumors that are hard to remove.
Can sphenoid wing meningioma be treated effectively?
Yes, sphenoid wing meningioma can be treated with surgery and radiation. The treatment depends on the tumor’s size, location, and type, and the patient’s health.