Last Updated on November 27, 2025 by Bilal Hasdemir
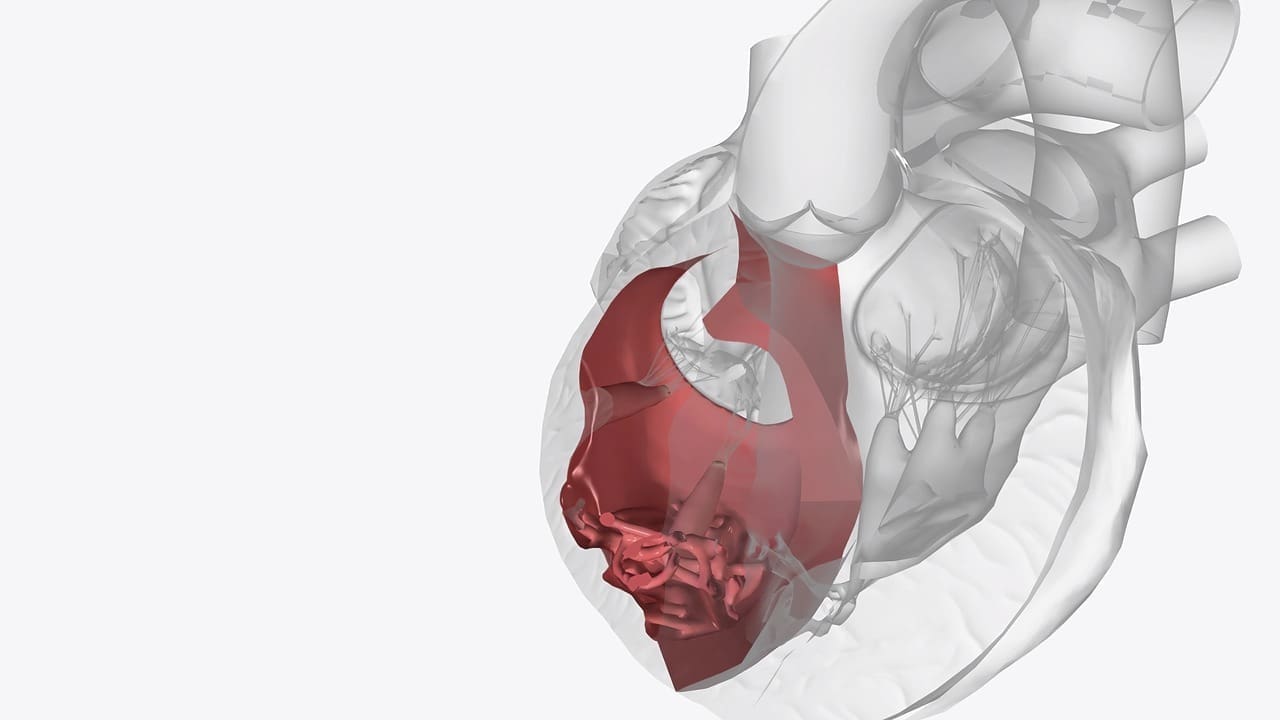
Calcification of heart valves is a serious condition. It happens when calcium builds up on the valve tissue or annulus. This can cause big problems, like aortic valve calcification, which affects many people worldwide.
At Liv Hospital, we know how important it is to understand why heart valves get calcified. Studies show that aging, birth defects, chronic inflammation, metabolic disorders, and lifestyle choices are key factors. We’ll dive into these causes and share useful tips to manage this condition well.
Calcified heart valves are a common issue, mainly seen in older adults. This happens when calcium builds up on the valve tissue, making it stiff and less functional. It can greatly affect a person’s life and may cause serious problems if not treated.
The buildup of calcium on valve tissue is complex. It’s influenced by aging, inflammation, and metabolic disorders. As we get older, our valve tissue changes, making it more prone to calcification. High blood pressure and kidney disease can also speed up this process.
Calcium deposits on heart valves make them stiff and less flexible. This can cause blood flow issues, as the heart has trouble pumping. If not managed, it can lead to heart failure.
The aortic and mitral valves are most often affected by calcification. These valves are key to ensuring blood flows properly through the heart.
Aortic valve calcification causes calcium to build up on the aortic valve. This can lead to aortic stenosis, where the valve opening narrows. This narrowing blocks blood flow, causing symptoms like chest pain, shortness of breath, and fatigue.
Mitral valve calcification involves calcium deposits on the mitral valve. It can cause mitral annular calcification (MAC), where calcium builds up around the valve ring. MAC is more common in older adults and can lead to mitral regurgitation, where blood leaks back through the valve.
Knowing the causes and effects of calcification on these valves is key to finding effective treatments and improving patient care.
Aging is a key factor in heart valve calcification. As we age, our heart valves change, making them more likely to calcify.
Heart valves change with age, becoming thicker and stiffer. This is due to calcium buildup, sped up by aging. These changes are a main reason for calcification, often seen in the aortic valve.
Elderly people face a higher risk of heart valve calcification. This is because their valve tissue deteriorates over time. Older adults also have more health issues, like high blood pressure and atherosclerosis. These factors greatly increase the risk.
Heart valve calcification usually starts after 65. As we get older, the risk grows. Knowing when it starts helps in early treatment.
Understanding aging’s role in heart valve calcification helps us prevent and manage it better.
Congenital valve anomalies are key in calcification development, impacting valve function over time. These heart valve defects can alter valve structure and function. This increases the risk of calcification.
A bicuspid aortic valve is a common congenital heart defect. It affects the aortic valve, making it have only two cusps instead of three. This condition raises the risk of calcification due to abnormal blood flow and increased pressure on the valve.
Studies have shown that individuals with a bicuspid aortic valve are more likely to develop calcification. This can lead to valve stenosis and other complications.
Other congenital heart valve defects, like pulmonary valve stenosis and mitral valve prolapse, also raise calcification risk. These defects cause abnormal blood flow, leading to increased pressure on the valve and calcification. Early detection and monitoring of these conditions are key to prevent long-term damage.
Early detection and monitoring of congenital valve anomalies are vital to prevent complications from calcification. Regular echocardiograms and other diagnostic tests help identify valve abnormalities. They also monitor their progression over time.
“Early intervention can significantly improve outcomes for individuals with congenital heart valve defects,” says a leading cardiologist.
By identifying these conditions early, healthcare providers can develop effective management plans. These plans help reduce the risk of calcification and other complications.
Chronic inflammation plays a big role in heart valve calcification. It can cause many heart diseases. Heart valves are very affected by it.
Inflammation starts a chain of events that can harden heart valves. This makes valves stiff and less functional.
Rheumatic heart disease is a major cause of valve damage. It comes from an immune reaction to strep infections. This can scar and harden heart valves.
Endocarditis, an infection inside the heart, can also harm valves. It causes inflammation that damages valve structures. This can lead to serious long-term problems.
The change from inflammation to calcification is complex. It involves many cellular and molecular steps. Knowing this is key to finding ways to stop or treat it.
| Condition | Effect on Heart Valves | Potential Outcome |
|---|---|---|
| Rheumatic Heart Disease | Scarring and Calcification | Valve Dysfunction |
| Endocarditis | Valve Damage and Scarring | Calcification and Stenosis |
| Chronic Inflammation | Progressive Calcification | Heart Valve Disease |
Understanding how chronic inflammation damages heart valves is important. It helps us manage and maybe even prevent calcification.
Metabolic disorders and heart valve calcification are closely linked. Several conditions are major risk factors. We’ll look at how kidney disease, diabetes, and other disorders contribute to calcification.
Kidney disease is a key metabolic disorder affecting heart valves. It causes a calcium-phosphate imbalance. This imbalance leads to calcium deposits on heart valves, causing calcification. Patients with chronic kidney disease are at higher risk.
Diabetes is also linked to heart valve calcification. High blood sugar damages heart valves, making them more prone to calcification. Diabetes speeds up valve deterioration and complicates calcification management.
Other metabolic conditions also raise heart valve calcification risk. Hyperparathyroidism and Paget’s disease are notable examples.
Hyperparathyroidism causes an imbalance in calcium levels. This imbalance can lead to heart valve calcification. We must closely monitor patients with hyperparathyroidism for valve calcification signs.
Paget’s disease affects bone remodeling, leading to abnormal bone structure. It also affects heart valves, making them more susceptible to calcification. Managing Paget’s disease is key to preventing valve calcification.
In conclusion, metabolic disorders are critical in heart valve calcification. Understanding these conditions is vital for effective management. We must consider our patients’ metabolic health when assessing calcification risk.
Abnormal blood lipids, like high cholesterol and triglycerides, are key in valve calcification. We’ll look at how these lipids affect valve calcification. We’ll also talk about how to prevent it.
High cholesterol and triglycerides increase heart disease risk. Elevated LDL cholesterol, or “bad” cholesterol, causes lipid buildup in valves. This leads to calcification. High triglycerides also contribute to atherosclerosis, which is linked to valve calcification.
Atherosclerosis, or plaque buildup in arteries, shares risk factors with valve calcification. It can cause valve tissue calcification, mainly in the aortic valve. Studies have shown a link between atherosclerosis and valve calcification, indicating a common cause.
Controlling blood lipids is key to preventing valve calcification. Lipid-lowering therapies, like statins, can lower cholesterol and slow atherosclerosis. A healthy diet and exercise also help keep lipid levels in check. These steps can lower the risk of valve calcification.
Lifestyle choices greatly affect heart valve calcification. Some habits can speed up this process. It’s important to know which ones to avoid.
Smoking is bad for your heart, including your valves. It causes oxidative stress, which harms the valves. Quitting smoking is key to lowering your risk.
Being overweight is linked to metabolic syndrome, a heart disease risk. Obesity’s inflammation and metabolic issues speed up valve calcification. Staying at a healthy weight is essential for your heart.
Hypertension, or high blood pressure, strains the heart valves, like the aortic valve. This strain can cause calcification over time. It’s important to manage high blood pressure to prevent valve damage.
A sedentary lifestyle increases heart valve calcification risk. Exercise keeps your heart healthy and lowers calcification risk. Try brisk walking a few times a week for better heart health.
In summary, smoking, obesity, hypertension, and a sedentary lifestyle all speed up heart valve calcification. Making smart lifestyle choices can help prevent this condition and keep your heart healthy.
Diagnosing calcified heart valves needs a detailed approach. This includes advanced imaging and clinical checks. We’ll look at how to diagnose and manage these valves.
Advanced imaging is key in finding and checking calcified heart valves. Two main tools are echocardiography and CT scanning.
Echocardiography is a non-invasive method. It gives clear images of the heart valves. This helps check their structure and function. It’s often used at first and for follow-ups.
CT scanning helps measure calcium buildup on heart valves. This score shows how severe the calcification is. It helps doctors decide on the best treatment.
Medical management aims to control symptoms and slow the disease. It includes medicines for high blood pressure and cholesterol. These are risk factors for valve calcification.
For severe calcification, surgery might be needed. There are two main options: valve replacement and transcatheter procedures.
Valve replacement surgery replaces the damaged valve with a new one. This can be mechanical or bioprosthetic. It’s a traditional and effective treatment for severe calcification.
Transcatheter procedures, like TAVR, are less invasive than surgery. They’re great for patients at high risk for surgery complications.
Understanding why heart valves calcify is key to managing and preventing it. Aging, congenital issues, chronic inflammation, metabolic disorders, and lifestyle choices all play a part. Recent studies highlight the importance of a holistic approach, combining medical treatments and lifestyle changes.
By being proactive, people can lower their risk of heart valve calcification. A healthy lifestyle, managing health conditions, and regular check-ups are essential. Medical treatments like lowering cholesterol and controlling blood pressure are also vital.
Working with healthcare providers and making smart choices can help control heart valve health. Managing calcification of heart valves needs a team effort. We’re dedicated to top-notch healthcare for international patients.
Calcification of heart valves is when calcium builds up on the valves. This makes the valves stiff and can stop them from working right. It can happen to the aortic and mitral valves, among others.
Many things can cause heart valve calcification. These include getting older, being born with certain heart issues, long-term inflammation, metabolic problems, and lifestyle choices like smoking and being overweight.
As people get older, their heart valves can start to calcify. This is because the valves change with age, making older people more likely to get this condition.
Heart valve problems you’re born with, like a bicuspid aortic valve, can make you more likely to get calcification. It’s important to catch and watch these problems early to help prevent them.
Long-term inflammation, like in rheumatic heart disease and endocarditis, can cause calcification. This is because it damages and scars the valves.
Certain metabolic problems, like kidney disease, diabetes, hyperparathyroidism, and Paget’s disease, can lead to more calcium on the valves. This makes the valves wear down faster.
Yes, things like smoking, being overweight, high blood pressure, and not being active can make heart valve calcification worse. They can cause more stress on the valves and harm the heart.
Doctors use imaging like echocardiography and CT scans to see how much calcium is on the valves. This helps them figure out how bad the calcification is.
Doctors can treat calcified heart valves with medicine or surgery. Surgery might include replacing the valve or using a new procedure for severe cases.
While some risks can’t be changed, managing your lifestyle and health can help prevent or slow calcification. This includes keeping your blood lipids in check.
Aortic valve calcification is serious because it can lead to aortic stenosis. This is a serious heart disease that needs quick treatment.
High levels of cholesterol and triglycerides can increase the risk of valve calcification. This is because they contribute to atherosclerosis, which is linked to valve disease.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!