Last Updated on December 3, 2025 by Bilal Hasdemir
Chemotherapy is a common treatment for many types of cancer, but it’s not always the right option for everyone. Some patients worry about the “signs chemo is killing you when they feel severe side effects. While chemotherapy can cause fatigue, nausea, infections, and low blood counts, these symptoms usually mean the treatment is working hard against cancer not that it’s killing you. However, if side effects become extreme or life-threatening, it’s important to seek medical attention right away. Always discuss any serious concerns with your oncologist.
For many, chemotherapy is a lifeline against cancer. Yet, it’s important to know when chemotherapy side effects are too much.
We’ll look into the concerns about chemotherapy. This includes when to stop chemo for colon cancer and what happens if an oncologist decides to stop treatment.
Key Takeaways
- Knowing when chemotherapy isn’t working is vital for cancer patients.
- Chemotherapy side effects can be severe and affect quality of life.
- Oncologists look at many factors before stopping chemotherapy.
- Patients should talk to their oncologist about treatment options and prognosis.
- There might be other treatments for those who don’t respond to chemotherapy.
Understanding Chemotherapy and Its Purpose

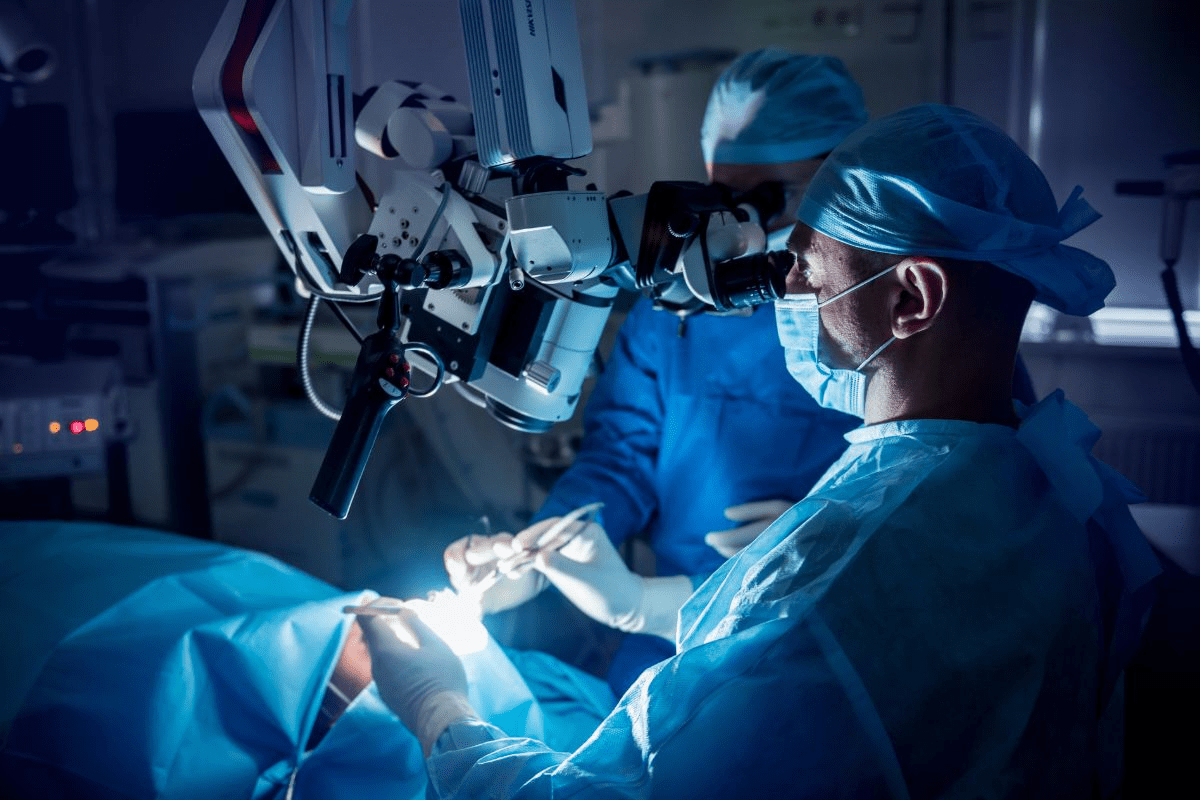
It’s important for patients to understand chemotherapy when looking at cancer treatment options. Chemotherapy uses drugs to kill cancer cells all over the body. It’s a key part of cancer care, often used with surgery and radiation therapy.
How Chemotherapy Works in Cancer Treatment
Chemotherapy targets cells that grow fast, like most cancer cells. The drugs in chemotherapy stop these cells from dividing and eventually kill them. This helps treat cancer that has spread or might spread.
Chemotherapy plays a big role in cancer treatment: it can shrink tumors before surgery, kill cancer cells after surgery, or be the main treatment for some cancers.
The 7 Main Types of Chemotherapy and Their Differences
There are many types of chemotherapy, each working in its own way. The main types include:
- Alkylating agents, which damage the DNA of cancer cells to stop them from reproducing.
- Antimetabolites, which block the making of DNA and RNA.
- Anthracyclines, a type of antibiotic that stops DNA and RNA making by getting in between DNA strands.
- Plant alkaloids, made from plants, which stop cancer cells from growing.
- Topoisomerase inhibitors, which mess with enzymes needed for DNA replication.
- Corticosteroids, used for certain lymphoma and leukemia types.
- Miscellaneous chemotherapy agents, including drugs that don’t fit into other categories but are effective against cancer.
Cancer experts say, “The choice of chemotherapy depends on the cancer type, its stage, and the patient’s health.”
“Chemotherapy is a highly personalized treatment, and what works for one patient may not work for another.”
Medical Contraindications for Chemotherapy
It’s key to know when chemotherapy isn’t right for everyone. This treatment uses drugs to fight cancer cells. But, it’s not safe for all due to health risks.
Pre-existing Health Conditions That Prevent Chemo
Some health issues make chemotherapy too dangerous. For example, severe heart disease, kidney problems, and liver issues. Some drugs can make heart problems worse, leading to heart failure.
| Health Condition | Potential Chemotherapy Risk |
| Severe Heart Disease | Increased risk of heart failure or cardiac complications |
| Kidney Dysfunction | Reduced ability to filter and eliminate chemotherapy drugs, potentially leading to increased toxicity |
| Liver Disease | Impaired metabolism of chemotherapy drugs, potentially leading to increased toxicity or reduced efficacy |
Oncologists say, “The presence of significant comorbidities can complicate the administration of chemotherapy, requiring careful consideration of the risk-benefit ratio.” (
This quote highlights the importance of assessing overall health before starting chemotherapy.
)
Age-Related Considerations for Chemotherapy
Age is a big factor in deciding if chemotherapy is right. Older adults might face more risks because their bodies can’t handle it as well. They also might have other health issues that make treatment harder.
Key age-related considerations include:
- Decreased renal function
- Increased risk of myelosuppression
- Potential for increased toxicity due to reduced drug clearance
When Poor Health Status Makes Chemo Too Risky
Those in poor health might not be good candidates for chemotherapy. This includes people who have lost a lot of weight, have a low performance status, or have widespread cancer. In these cases, the risks might be too high.
We look at each patient’s health, cancer type, and stage to choose the best treatment. This way, we offer care that fights cancer while keeping risks and side effects low.
When Cancer Types Are Resistant to Chemotherapy
Chemotherapy is a common cancer treatment, but some cancers don’t respond well. This can happen for many reasons. The type of cancer, genetic changes, and the cancer’s biology all play a part.
Cancer Types Known to Respond Poorly to Chemo
Some cancers don’t react well to chemotherapy. For example, triple-negative breast cancer doesn’t have certain receptors. This makes it hard to treat with some therapies, leaving chemotherapy as a main option.
Other cancers that might not respond to chemotherapy include:
- Pancreatic cancer, often found late and hard to treat
- Liver cancer, like hepatocellular carcinoma, can resist treatment
- Certain sarcomas, rare and tough to manage
Genetic Factors in Chemotherapy Resistance
Genetics are key in making some cancers resistant to chemotherapy. Changes in genes can affect how cancer cells react to treatment. For example, a TP53 gene mutation can make cancer resistant.
Knowing the genetic reasons for resistance helps in finding new treatments. These treatments can target specific weaknesses in cancer cells.
| Genetic Factor | Description | Impact on Chemotherapy |
| TP53 mutation | Mutation in the TP53 tumor suppressor gene | Leads to resistance to chemotherapy |
| BRCA1 and BRCA2 mutations | Mutations in genes involved in DNA repair | Affects response to certain chemotherapies |
Treatment Alternatives for Chemo-Resistant Cancers
For cancers that don’t respond to chemotherapy, new treatments are being looked into. These include targeted therapies, immunotherapies, and other innovative methods.
Targeted therapies, for example, aim at specific genetic changes in cancer cells. This approach is more personalized and can be more effective.
Signs Chemo is Killing You: Recognizing Dangerous Reactions
Chemotherapy can have tough side effects, some serious enough to be life-threatening. It’s a strong tool against cancer, but knowing the difference between normal and dangerous side effects is key. Patients and caregivers need to be aware of this.
Life-Threatening Side Effects vs. Normal Reactions
Chemotherapy impacts people differently. Some may face mild side effects, while others deal with severe ones. Normal side effects include fatigue, hair loss, and nausea. These are usually manageable.
But, life-threatening side effects need quick medical help. They can include:
- Severe neutropenia (low white blood cell count), which can lead to serious infections
- Severe anemia (low red blood cell count), causing extreme fatigue and shortness of breath
- Thrombocytopenia (low platelet count), which can result in excessive bleeding
- Severe allergic reactions, such as anaphylaxis
Emergency Symptoms That Require Immediate Medical Attention
Some symptoms during or after chemotherapy are urgent. If you have any of these, get medical help fast:
| Symptom | Description |
| Fever | Temperature above 100.4 °F (38 °C), indicating a possible infection |
| Severe Pain | Pain that can’t be controlled with the medicine you’re taking |
| Shortness of Breath | Difficulty breathing or feeling like you can’t catch your breath |
| Severe Bleeding | Excessive bleeding or bruising, including nosebleeds or bleeding gums |
If you’re experiencing any of these emergency symptoms, don’t wait. Contact your healthcare provider or seek emergency care.
When to Call Your Oncologist About Side Effects
It’s not always clear when to contact your oncologist. But it’s better to be safe than sorry. If you’re worried about side effects or if they’re getting worse, reach out to your healthcare team.
Keep a record of your side effects, including when they happen and how bad they are. This will help you talk to your oncologist. They can offer advice on managing side effects and if any changes to your treatment are needed. We’re here to support you through your cancer journey, and quick communication is key to the best outcomes.
Heart Damage from Chemotherapy: Cardiac Warning Signs
It’s important for patients and to know about heart risks from chemotherapy. Chemotherapy is a key part of cancer treatment but can harm the heart. This part talks about how some chemotherapy drugs can hurt the heart, the signs of heart problems from chemo, and why it’s key to watch heart health during treatment.
Cardiotoxic Chemotherapy Drugs
Some chemotherapy drugs can harm the heart. These include:
- Anthracyclines (e.g., doxorubicin and epirubicin), used for many cancers but can cause lasting heart damage.
- Trastuzumab, for HER2-positive breast cancer, can lead to heart failure in some.
- Fluorouracil (5-FU), which can cause heart problems like ischemia or heart attack in rare cases.
Patients should talk to their oncologist about their treatment to know about heart risks.
Symptoms of Chemotherapy-Induced Heart Problems
It’s key to know the signs of heart problems from chemo to act early. Common signs are:
- Shortness of breath, even when resting.
- Fatigue or feeling very tired.
- Swelling in the legs, ankles, and feet from fluid buildup.
- Rapid or irregular heartbeat.
If you notice these signs, tell your healthcare provider right away.
Monitoring Heart Health During Cancer Treatment
Keeping an eye on heart health during chemo is vital to avoid and manage heart damage. This includes:
- Regular echocardiograms or MUGA scans to check heart function.
- Biomarker tests, like troponin levels, to spot heart damage.
- Regular checks by to catch early signs of heart issues.
By watching heart health closely, can adjust treatments to lower heart risks. This helps ensure the best results for cancer patients.
Immune System Collapse: When Chemo Compromises Survival
Chemotherapy is a strong weapon against cancer but can weaken the immune system. This makes patients more likely to get serious infections and diseases. The immune system is key in fighting off these threats.
Dangerous Levels of Immunosuppression
Immunosuppression happens when the immune system can’t fight infections and diseases well. Chemotherapy can harm not just cancer cells but also the cells in the bone marrow. These cells are important for a strong immune system. Severe immunosuppression can cause serious infections and health problems.
We keep a close eye on patients getting chemotherapy for signs of immunosuppression. This includes checking their white blood cell counts. If counts get too low, we adjust their treatment to lower risks.
Infection Risks and Warning Signs
People with weak immune systems are more likely to get infections. Some common infections include:
- Febrile neutropenia, a condition with fever and low neutrophil counts
- Pneumonia and other respiratory infections
- Skin infections and cellulitis
It’s important for patients to know the signs of infection. These include fever, chills, persistent cough, or severe pain. They should seek medical help right away if they notice these signs.
Strategies to Support Immune Function During Treatment
While chemotherapy is needed to fight cancer, we can help support the immune system. Here are some ways:
- Prophylactic antibiotics: We might give antibiotics to prevent infections in patients with very weak immune systems.
- Growth factors: Medications that help the bone marrow make more white blood cells can lower infection risks.
- Nutritional support: Good nutrition is key for a strong immune system. We often suggest dietary changes or supplements.
- Infection control measures: Patients are taught how to avoid infections. This includes staying away from crowded places and practicing good hygiene.
By understanding the risks of chemotherapy and using strategies to reduce them, we can protect patients’ immune systems. This helps improve their chances of recovery.
Neurological Complications of Chemotherapy
Chemotherapy can affect the brain and nerves in many ways. It can change how we think and feel. Understanding these effects is key.
Cognitive Impairment and “Chemo Brain”
“Chemo brain” is a big worry. It makes it hard to remember things and focus. It can make everyday life tough.
“Chemo brain” is not just a minor side effect; it can be a debilitating condition that affects a patient’s ability to return to work or engage in daily activities. A patient once said, “It’s like my brain is foggy, and I struggle to remember simple things. It’s frustrating and scary.”
Peripheral Neuropathy and Nerve Damage
Peripheral neuropathy is another big problem. It damages nerves, causing numbness, tingling, and pain in hands and feet. Some chemo drugs are more likely to cause this.
- Numbness or tingling sensations in extremities
- Pain or burning feelings in hands and feet
- Muscle weakness or cramping
Dealing with peripheral neuropathy needs a lot of effort. This includes medicine, physical therapy, and changing how we live.
When Neurological Side Effects Become Debilitating
For some, chemo side effects are too much. They can really hurt how well you live. It’s important to think about other treatments that might not hurt as much.
“The hardest part is not knowing what’s going to happen next. One day I’m fine, and the next, I’m struggling to walk or remember my name. It’s a constant battle to stay ahead of these side effects.”
and patients work together to keep an eye on these side effects. They might change treatments to make things better. This could mean using different chemo drugs, taking less of it, or adding special therapies.
Quality of Life Considerations: When Treatment Becomes Unbearable
As cancer treatment goes on, how it affects a patient’s life is key. The goal is to live longer and better. We must find a balance between treatment benefits and its side effects.
Balancing Treatment Benefits Against Side Effects
Patients often face many side effects during treatment. It’s important to weigh these against the treatment’s benefits. This helps decide if continuing therapy is right.
Healthcare providers use tools to help make these decisions. They look at pain, fatigue, nutrition, and daily activities. This helps understand how treatment affects a patient’s life.
| Assessment Criteria | Description | Impact on Quality of Life |
| Pain Levels | Evaluation of pain intensity and its effect on daily activities | High pain levels can significantly reduce quality of life |
| Fatigue | Assessment of tiredness and its impact on physical and mental functions | Severe fatigue can limit a patient’s ability to engage in daily activities |
| Nutritional Status | Evaluation of dietary intake and nutritional deficiencies | Poor nutrition can exacerbate treatment side effects and reduce overall well-being |
Quality of Life Assessments During Cancer Treatment
Quality of life assessments are key in cancer care. They help understand treatment’s broader impact. These assessments are done through surveys or questionnaires.
Regular assessments help adjust treatment plans. This can reduce side effects or find better treatments for quality of life.
Patient Perspectives on Treatment Decisions
Patient views are vital in treatment choices. They add personal values and preferences. This helps tailor treatment plans to meet patient needs.
Open talks about treatment goals and side effects are important. Patients and healthcare providers can then make informed decisions together. This balances treatment benefits with its challenges.
When Oncologists Recommend Stopping Chemotherapy
Oncologists stop chemotherapy for specific reasons. This choice is made after a detailed look at the patient’s health, how well the treatment is working, and their quality of life.
Medical Criteria for Discontinuing Treatment
Several factors guide oncologists in stopping chemotherapy. These include cancer that keeps growing, severe side effects, and a big drop in the patient’s health. The main goal is to weigh the treatment’s benefits against its risks and how it affects the patient’s life.
“Stopping chemotherapy is a complex decision,” says a top oncologist. “It’s not just about the cancer. It’s about the patient’s overall health and what they want for their care.”
The Difficult Conversation About Ending Chemotherapy
Talking about stopping chemotherapy is tough. It needs empathy, clear explanations, and support. Oncologists must explain the reasons in a kind way, while also guiding on what to do next and where to find help.
- Explaining the medical reasons for discontinuing chemotherapy
- Discussing alternative treatment options or palliative care
- Addressing patient concerns and fears about stopping treatment
Second Opinions and Treatment Reassessment
Patients can ask for second opinions, which is their right. This can offer new insights and reassurance. Oncologists often suggest second opinions to confirm the diagnosis and treatment, or to find other helpful options.
Getting a second opinion is key to making sure patients get the best care. It’s a choice that healthcare providers should support, as it can greatly affect patient outcomes and satisfaction.
Cancer-Specific Guidelines: When to Stop Chemotherapy
Different cancers react differently to chemotherapy. It’s key to have guidelines specific to each cancer. These guidelines help patients and decide when to keep or stop treatment.
When to Stop Chemo for Colon Cancer
Chemotherapy is often used after surgery for colon cancer. It aims to kill any remaining cancer cells. The decision to stop depends on the cancer’s stage, the patient’s health, and how well the treatment works.
Typically, chemotherapy stops if the disease gets worse or side effects become too much. We use treatments like FOLFOX or CAPOX for colon cancer. These have been shown to improve survival rates. Treatment usually lasts 3 to 6 months if the response is good.
When to Stop Chemo for Pancreatic Cancer
Pancreatic cancer is often diagnosed late, making treatment tough. Chemotherapy is used to control symptoms and slow disease growth. The decision to stop depends on the patient’s health, if the cancer has spread, and how well it responds to treatment.
For pancreatic cancer, treatments like FOLFIRINOX or gemcitabine plus nab-paclitaxel are common. Treatment stops if the disease gets worse or if side effects are severe.
Treatment Limitations for Other Cancer Types
Chemotherapy works differently for various cancers. For some, like certain leukemia or lymphoma, it’s very effective. For others, like glioblastoma or advanced pancreatic cancer, options are limited.
| Cancer Type | Common Chemotherapy Regimens | When to Stop Treatment |
| Colon Cancer | FOLFOX, CAPOX | After 3-6 months or with significant disease progression |
| Pancreatic Cancer | FOLFIRINOX, Gemcitabine + nab-paclitaxel | With significant disease progression or severe side effects |
| Breast Cancer | AC-T, TCHP | After completion of planned cycles or with disease progression |
Knowing when to stop chemotherapy is key. It helps balance treatment benefits and side effects. By following cancer-specific guidelines, patients and can make better care decisions.
Measuring Effectiveness: Signs Chemo Isn’t Working
Oncologists look at several key signs to see if chemotherapy is working. It’s important to check if treatment is effective. This helps us make changes to improve patient outcomes.
How Oncologists Evaluate Treatment Response
We check treatment response through exams, lab tests, and imaging. Tumor markers and imaging results are key. They tell us if chemotherapy is working as planned.
Oncologists watch for signs that cancer is shrinking or symptoms are getting better. Regular checks help us spot problems early. Then, we can adjust the treatment plan.
Tumor Markers and Imaging Results
Tumor markers are substances made by cancer cells. Blood tests track these markers. A drop in levels means treatment is likely working.
Imaging tests like CT scans or MRIs show how tumors are responding. They help us see if tumors are getting smaller or spreading.
When Cancer Progresses Despite Treatment
Sometimes, cancer keeps growing even with chemotherapy. This can happen if the cancer becomes resistant to drugs or is very aggressive.
If cancer keeps growing, we look for other treatments. This might include targeted therapies or trials. Our aim is to find the best treatment while keeping the patient’s quality of life good.
It’s important to know when chemotherapy isn’t working. By watching how treatment is going and making changes, we can give each patient the best care.
Alternative Approaches When Chemo is Not an Option
When chemotherapy is not an option, patients and look for other ways to manage cancer. This change is key to keeping patients comfortable and treating the disease well.
Targeted Therapies and Immunotherapies
Targeted therapies and immunotherapies are big steps forward in cancer treatment. They don’t harm healthy cells like old chemotherapy did. Instead, they target cancer’s growth and the immune system to fight cancer cells.
Examples of targeted therapies include:
- Tyrosine kinase inhibitors, which block enzymes that promote cancer cell growth.
- Monoclonal antibodies that target specific proteins on cancer cells.
Immunotherapies are very promising. Treatments like checkpoint inhibitors help the immune system attack cancer cells better.
| Therapy Type | Description | Examples |
| Targeted Therapy | Focuses on specific molecules involved in cancer growth | Tyrosine kinase inhibitors, Monoclonal antibodies |
| Immunotherapy | Harnesses the immune system to fight cancer | Checkpoint inhibitors, CAR-T cell therapy |
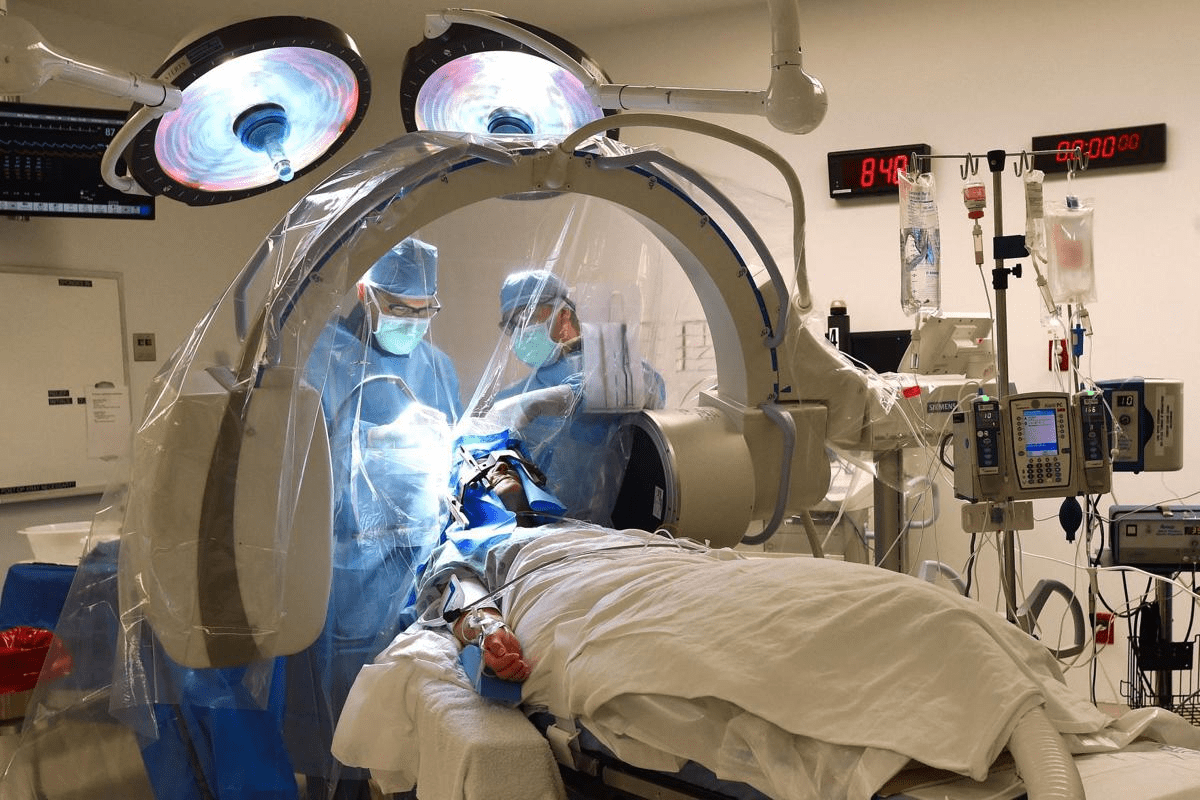
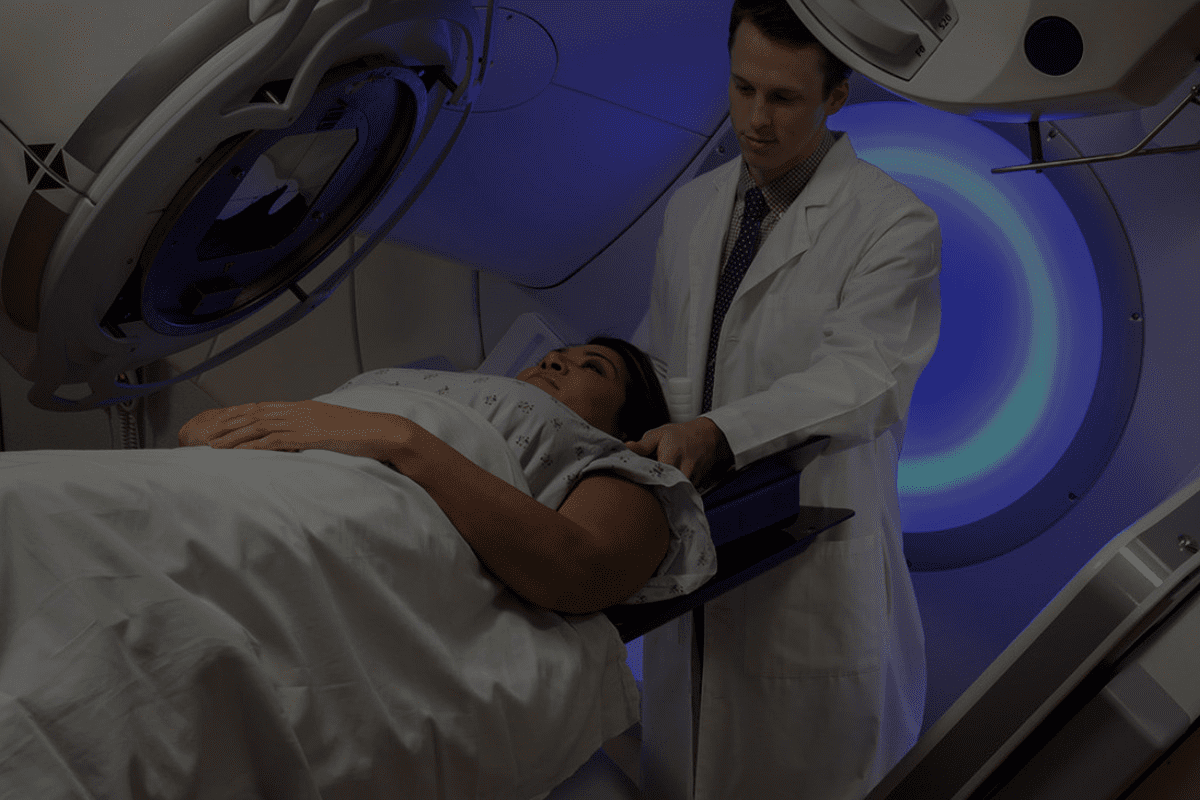
Radiation and Surgical Alternatives
Radiation therapy and surgery are important when chemotherapy isn’t an option. Radiation uses high-energy to kill cancer cells. Surgery removes tumors.
Advances in radiation therapy make it more precise, protecting healthy tissue. Techniques like SBRT and IMRT have improved patient outcomes.
Surgery has also improved, with less invasive methods. This reduces recovery time and improves comfort. Sometimes, surgery can even cure cancer if it’s caught early.
Palliative Care Approaches for Symptom Management
Palliative care helps with symptoms and stress of serious illnesses like cancer. It’s not about curing but improving life quality for patients and their families.
“Palliative care is about understanding the patient’s needs and providing complete support for their physical, emotional, and social well-being.” -Palliative Care Specialist
Palliative care teams manage pain, nausea, and other symptoms. They ensure patients live as comfortably as possible.
Making Informed Decisions About Refusing Chemotherapy
Deciding to refuse chemotherapy is a big choice. It involves knowing your rights, the possible outcomes, and other treatment options. You need to think about many things to make a choice that fits your values and health situation.
Patient Rights in Treatment Decisions
Patients have the right to decide on their cancer treatment, including saying no to chemotherapy. This right is key to patient freedom and is backed by health guidelines and laws.
- Informed Consent: Patients must know all about their diagnosis, treatment choices, and the risks and benefits of each option.
- Right to Refuse: Patients can say no to any treatment, including chemotherapy, at any time.
- Alternative Options: should talk about other treatments or palliative care with patients who don’t want chemotherapy.
What to Expect if You Decline Chemotherapy
Choosing not to have chemotherapy can affect your health and life quality. It’s important to understand these effects to make a good choice.
Potential Outcomes:
- The cancer might grow faster without chemotherapy.
- Worsening symptoms could lower your quality of life.
- might suggest other treatments or palliative care to help manage symptoms and improve life quality.
Talking to your healthcare team about your worries and hopes is key. This way, you can understand what refusing chemotherapy might mean for you.
Communicating Your Wishes to Healthcare Providers
Talking openly with your healthcare team is vital when deciding about chemotherapy. Share your concerns, preferences, and values with them.
Tips for Communicating:
- Write down questions for appointments to cover all your concerns.
- Bring a family member or friend for support during appointments.
- Be straightforward about your wishes regarding chemotherapy and other treatments.
Good communication helps ensure your healthcare team gets and respects your decisions about chemotherapy.
Rebuilding Health After Stopping Chemotherapy
Recovering from chemotherapy is a complex process. It involves getting stronger, rebuilding your immune system, and improving your overall health.
Rebuilding Your Immune System After Chemo
Chemotherapy weakens your immune system, making you more likely to get sick. To strengthen your immune system, you should:
- Maintain good hygiene practices, such as frequent handwashing
- Avoid close contact with people who are sick
- Get enough sleep to help your body recover
- Stay physically active, as recommended by your healthcare provider
Nutritional Support for Recovery
Eating well is key to recovering from chemotherapy. Nutritional support boosts your energy and strengthens your immune system. Eat:
- A variety of fruits and vegetables rich in antioxidants
- Lean proteins to help repair tissues
- Whole grains for fiber and essential nutrients
- Adequate hydration through water and other fluids
Avoid foods that are hard to digest or cause discomfort. Talking to a registered dietitian or healthcare provider can help with meal planning.
Physical and Emotional Healing Strategies
Recovering from chemotherapy is not just about physical health. It’s also about emotional healing. Physical healing strategies include:
- Gradually increasing physical activity
- Engaging in rehabilitation programs if recommended
- Managing pain and other symptoms with the help of your healthcare team
For emotional healing, consider:
- Seeking support from family, friends, or support groups
- Engaging in activities that bring joy and relaxation
- Practicing mindfulness or other stress-reduction techniques
Recovering from chemotherapy is a journey that needs patience, support, and a holistic approach. By focusing on immune system recovery, nutrition, and both physical and emotional healing, you can regain your strength and improve your life quality.
Supporting a Loved One Through Difficult Treatment Decisions
Supporting a family member or friend with cancer is more than just being there. It’s about talking well and understanding. As a caregiver or loved one, knowing and being supportive is key during cancer treatment.
Communication Strategies with Cancer Patients
Good communication is key in supporting a loved one with cancer. This means:
- Active Listening: Really listen to what the patient says, both in words and body language.
- Open-Ended Questions: Ask questions that let the patient share their feelings and worries.
- Clear Information Sharing: Make sure the patient has all the info they need to make care choices.
Respecting Patient Autonomy While Providing Support
It’s vital to support while also respecting the patient’s choices. This means:
- Understanding and respecting the patient’s treatment wishes.
- Not pushing your own views or feelings on the patient.
- Being ready to help when asked, but not too much.
Resources for Caregivers and Family Members
Caregivers and family members need support too. There are many resources available:
- Support Groups: Joining a group can offer a sense of community and understanding.
- Counseling Services: Professional counseling can help with the emotional challenges of caregiving.
- Educational Materials: There are many resources to learn about the patient’s condition and how to care for them best.
By using these strategies and resources, loved ones can offer real support to cancer patients facing tough treatment choices.
Conclusion: Balancing Hope and Reality in Cancer Treatment
It’s key to balance hope and reality when making cancer treatment choices. Knowing what chemotherapy can and can’t do helps patients and families make smart decisions about their care.
We’ve looked into the complex world of chemotherapy. We’ve seen when treatment might not work or could be harmful. It’s important to spot these signs early to decide if to keep going or stop.
Every person’s cancer is different, and what works for one might not work for another. By knowing the good and bad of chemotherapy, patients can work with their. Together, they can create a treatment plan that fits the patient’s needs and goals.
In the end, finding the right balance in cancer treatment means understanding all options. It also means caring for patients in a way that respects their unique situation and goals. This way, we help patients make choices that are right for them.
FAQ
Can chemotherapy cure cancer?
Chemotherapy can cure some cancers, but it depends on the cancer type, stage, and individual factors. It’s not effective for all cancers.
What are the long-term side effects of chemotherapy?
Long-term side effects can include heart damage, neurological problems, and a higher risk of secondary cancers. These effects can be serious.
Is chemotherapy always the best option for cancer treatment?
No, chemotherapy isn’t always the best choice. The decision depends on the cancer type, stage, overall health, and what the patient prefers.
How can caregivers support loved ones through difficult treatment decisions?
Caregivers can offer emotional support and help with communication with healthcare providers. They should also respect the patient’s wishes while providing resources for themselves.
What are the signs that chemotherapy is not working?
Signs that chemotherapy isn’t working include cancer growing, tumors getting bigger, and symptoms getting worse. This means it’s time to look at other treatment options.
How do oncologists evaluate the effectiveness of chemotherapy?
Oncologists check how well treatment is working by looking at tumor markers and imaging results. They assess if chemotherapy is effective or if other options are needed.
What are the cancer-specific guidelines for stopping chemotherapy?
Guidelines for stopping chemotherapy vary by cancer type. They are based on medical criteria and how well the treatment is working.
How can patients rebuild their health after stopping chemotherapy?
Rebuilding health involves strengthening the immune system and getting nutritional support. It also means finding ways to heal physically and emotionally.
Can patients refuse chemotherapy?
Yes, patients can choose not to have chemotherapy. It’s important to talk about this with healthcare providers and understand the consequences.
What are the alternatives to chemotherapy?
Alternatives include targeted therapies, immunotherapies, radiation, and surgery. Palliative care is also an option for managing symptoms when chemotherapy isn’t suitable.
When is it recommended to stop chemotherapy?
Stopping chemotherapy depends on several factors. These include how well the treatment is working, the severity of side effects, and the patient’s health.
What are the neurological complications associated with chemotherapy?
Chemotherapy can cause brain problems, nerve damage, and other neurological issues. These can be very debilitating and affect daily life.
How does chemotherapy affect the immune system?
Chemotherapy can weaken the immune system. This makes it harder to fight off infections and can lead to serious complications. It’s key to support immune function during treatment.
Can chemotherapy damage the heart?
Yes, some chemotherapy drugs can harm the heart. This can lead to heart failure, arrhythmias, and cardiac ischemia. It’s important to watch heart health during treatment.
What are the signs that chemotherapy is causing harm?
Signs of harm from chemotherapy include severe side effects and allergic reactions. Look out for trouble breathing, chest pain, or severe bleeding.