Last Updated on November 27, 2025 by Bilal Hasdemir
Spinal cord injuries are a big health problem worldwide. They affect between 250,000 and 500,000 people every year. We know how important it is to give these injuries the right care.
The level and type of spinal cord injury greatly affect symptoms, recovery, and daily life. At Liv Hospital, we focus on each patient to help them recover as much as possible.
It’s important to know the different types of spinal cord injury and how they affect the body. We aim to give top-notch healthcare to all our patients, including those from abroad.
Key Takeaways
- Spinal cord injuries affect 250,000 to 500,000 people worldwide each year.
- The level of injury significantly impacts symptoms and recovery.
- A patient-centered approach is crucial for maximizing rehabilitation outcomes.
- Understanding the type and level of injury is key to effective treatment.
- Liv Hospital provides comprehensive care for international patients.
Understanding Spinal Cord Injuries: An Overview

It’s important to understand spinal cord injuries to help those affected. These injuries are a big health issue worldwide. They can happen from accidents, falls, or sports injuries.
Global Impact and Statistics
Every year, between 250,000 and 500,000 people get spinal cord injuries globally. This shows how hard it is to track these cases.
These injuries have a big impact on people, families, and healthcare systems. The World Health Organization says we need better ways to prevent and treat these injuries.
“The global burden of spinal cord injury is substantial, and there is a need for improved prevention and treatment strategies to address this growing concern.”
| Region | Estimated Annual Incidence |
|---|---|
| North America | 40 per million |
| Europe | 30 per million |
| Global Average | Between 250,000 and 500,000 |
Anatomy of the Spinal Cord
The spinal cord runs from the brain to the lower back. It controls many body functions. It’s protected by the spinal column, which has different parts.
Knowing the anatomy of the spinal cord helps us understand spinal injuries. The cord’s structure and function affect the injury’s level and severity.
Complete vs. Incomplete Injuries
Spinal cord injuries are either complete or incomplete. Complete injuries mean no function below the injury. Incomplete injuries mean some function is left.
- Complete injuries: Total loss of sensory and motor functions below the injury level.
- Incomplete injuries: Partial loss of sensory and motor functions, with varying degrees of impairment.
Knowing if an injury is complete or incomplete is key. It helps doctors plan the best treatment and rehabilitation for each patient.
How Spinal Cord Injury Levels Are Classified
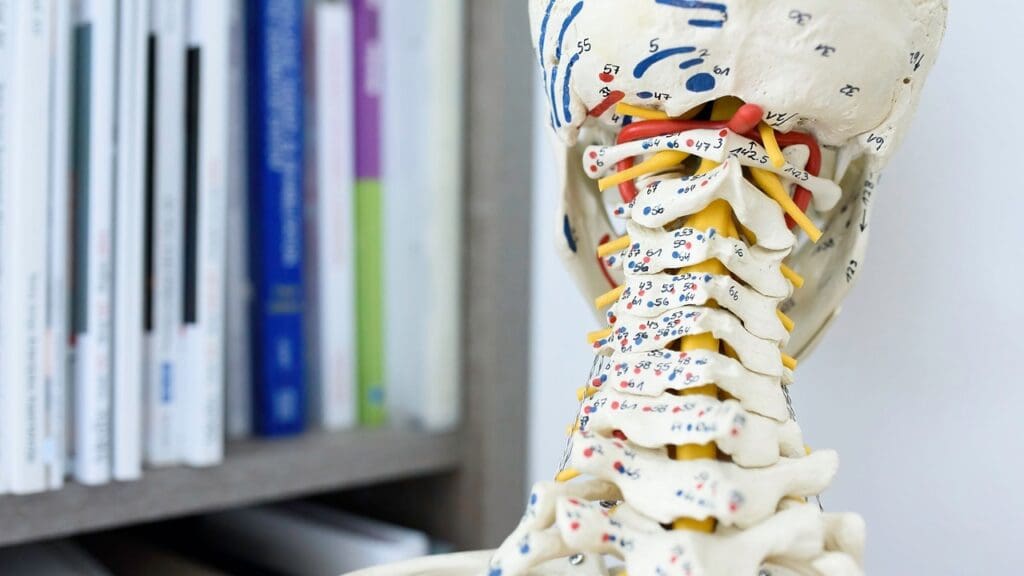
The spine is divided into several regions, and injuries are classified accordingly. Knowing how spinal cord injury levels are classified is key. It helps us understand the damage’s extent and plan the right treatment.
Cervical, Thoracic, Lumbar, and Sacral Regions
The human spine is divided into four main parts: cervical, thoracic, lumbar, and sacral. Each part has its own role and is linked to different injury levels.
- Cervical Region: The cervical spine is in the neck and has seven vertebrae (C1-C7). Injuries here can affect breathing and limb movement.
- Thoracic Region: The thoracic spine is in the mid-back and has twelve vertebrae (T1-T12). Injuries here can affect trunk stability and autonomic functions.
- Lumbar Region: The lumbar spine is in the lower back and has five vertebrae (L1-L5). Injuries here can affect lower limb function and control.
- Sacral Region: The sacral spine is at the base of the spine and has five fused vertebrae (S1-S5). Injuries here can impact bowel, bladder, and sexual functions.
Functional Impact Assessment
Assessing the functional impact of a spinal cord injury involves evaluating the injury level and damage extent. This helps us understand the individual’s potential limitations and capabilities.
We use various scales and assessments to determine the functional impact. These include:
- The American Spinal Injury Association (ASIA) Impairment Scale
- Muscle strength testing
- Sensory evaluation
Types of Spinal Injuries
Spinal cord injuries can be categorized into two main types: complete and incomplete.
- Complete Injuries: Result in total loss of sensory and motor function below the level of injury.
- Incomplete Injuries: Result in partial loss of sensory and motor function, with some degree of function preserved below the level of injury.
Understanding the type and level of injury is crucial. It helps us develop an effective rehabilitation plan and improve outcomes for individuals with spinal cord injuries.
Cervical Injuries (C1-C4): High Cervical Injuries
High cervical injuries at C1-C4 levels are very serious. They affect the top of the spinal cord. This impacts many bodily functions.
Functions Affected at C1-C4 Levels
Injuries at C1-C4 can harm many important functions. Respiratory function is often affected, as the diaphragm and other muscles are impacted. These injuries can also cause quadriplegia, leading to loss of motor function in all limbs.
The ability to control bladder and bowel functions may also be impaired. Patients with these injuries often need help with daily tasks due to their physical limitations.
Common Symptoms and Complications
Symptoms of high cervical injuries vary but often include respiratory distress, pain, and loss of motor function. Complications like autonomic dysreflexia can be life-threatening and need immediate medical care.
Other complications include pressure sores, deep vein thrombosis, and osteoporosis from prolonged immobility. Managing these complications is key to patient care.
Treatment Approaches for High Cervical Injuries
Treatment for high cervical injuries is complex. Acute stabilization is crucial, often needing surgery to secure the spine. Rehabilitation is vital to help patients regain independence.
Advanced respiratory care is needed for those with respiratory issues. Pain management strategies are also used to manage chronic pain from these injuries.
Cervical Injuries (C5-C7): Lower Cervical Injuries
Lower cervical injuries, like those at C5-C7, are tough for patients and doctors. They can make everyday life hard. These injuries limit how people can move and do things.
C5 Vertebrae Injury Symptoms
Injuries at C5 can cause muscle weakness, loss of feeling, and trouble moving. People might find it hard to move their arms. They may struggle with simple tasks. Quick action is key to help manage these issues.
Common signs of a C5 injury include:
- Weakness or paralysis in the arms or hands
- Numbness or tingling sensations
- Loss of bladder or bowel control
- Respiratory complications
C5-C6 SCI: Functions and Limitations
A spinal cord injury at C5-C6 can greatly affect how people function. Some may still have some movement, but others face big challenges. We tailor plans to meet each patient’s needs.
The effects of a C5-C6 SCI vary. Some common issues are:
- Reduced arm and hand function
- Difficulty with daily activities like dressing or eating
- Potential for respiratory problems
C5-C7 Spinal Injury: Wrist and Hand Function
Injuries at C5-C7 can severely impact wrist and hand use. Patients might feel weak, numb, or unable to move their hands. We use various treatments to help regain function and improve life quality.
Methods to manage wrist and hand issues after a C5-C7 injury include:
- Physical therapy to improve movement and strength
- Occupational therapy to learn new ways to do daily tasks
- Potential surgery to help restore function or ease pain
T1 Spinal Cord Injury: Functions, Symptoms, and Outlook
T1 spinal cord injuries have specific effects and symptoms that need careful medical care. We’ll explore how these injuries impact the body and discuss treatment options.
How T1 Injuries Affect Upper Body Function
T1 spinal cord injuries mainly affect the upper body less than cervical injuries. They happen lower in the spine. Yet, they can still impact hand and finger dexterity a lot.
People with T1 injuries usually keep full arm function. But, they might face some challenges with hand function.
Mobility and Independence with T1 Injuries
Mobility and independence are key in recovering from T1 spinal cord injuries. Even with T1 injuries, many people can become quite independent with the right rehab.
“Rehabilitation plays a vital role in helping individuals with spinal cord injuries to regain their independence and adapt to their new circumstances.”
Treatment and Rehabilitation Strategies
Treatment for T1 spinal cord injuries involves many steps. It includes acute care, surgery if needed, and a lot of rehab. Rehab aims to improve function and independence.
| Treatment Component | Description |
|---|---|
| Acute Care | Initial medical management to stabilize the patient and address immediate health concerns. |
| Surgical Intervention | Surgery may be required to realign vertebrae, relieve pressure on the spinal cord, or stabilize the spine. |
| Rehabilitation | A comprehensive program including physical therapy, occupational therapy, and other interventions to maximize functional recovery and independence. |
In conclusion, T1 spinal cord injuries bring their own set of challenges and chances for recovery. Knowing about their effects, symptoms, and treatment is key to giving the right care and support.
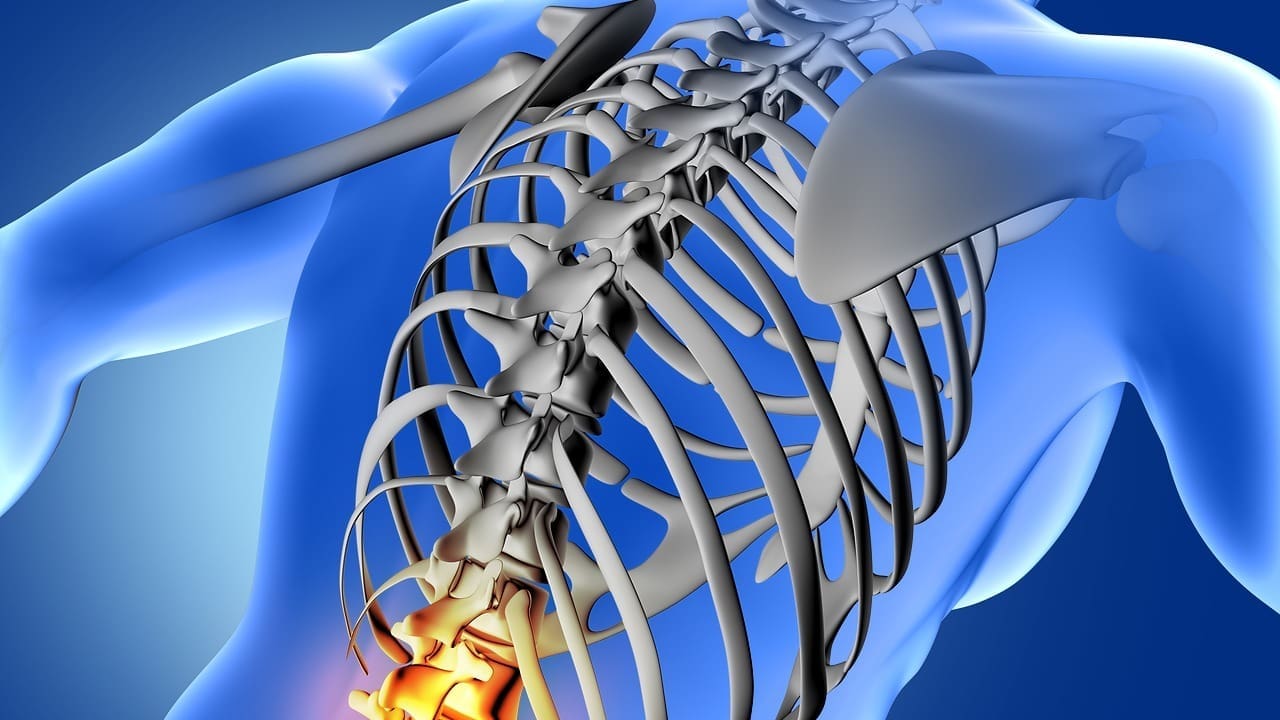
Thoracic Injuries (T2-T5): Upper Thoracic Region
The upper thoracic region, from T2 to T5, is very important. Injuries here can cause big problems. They can affect how our bodies work, leading to many symptoms and challenges.
T3 Paraplegia: Characteristics and Challenges
T3 paraplegia happens when the third thoracic vertebra is injured. People with T3 paraplegia lose control and feeling below the injury. They face challenges like unstable trunk, breathing problems, and trouble with body temperature.
- Loss of motor control below the T3 level
- Sensory impairments, including pain and temperature sensation
- Potential for autonomic dysreflexia, a life-threatening medical emergency
T5 Paraplegia: Functions and Limitations
T5 paraplegia occurs at the fifth thoracic vertebra. While some functions may be kept, T5 paraplegia causes a lot of paralysis and loss of feeling below the injury. How independent someone can be varies a lot, depending on their health and injury.
Common limitations include:
- Reduced mobility and reliance on wheelchairs
- Bowel and bladder dysfunction
- Potential for orthostatic hypotension and other cardiovascular issues
Treatment Approaches for Upper Thoracic Injuries
Dealing with upper thoracic injuries needs a team effort. This includes quick care, rehab, and ongoing management. Each treatment plan is made just for the person, and might include surgery, physical therapy, and medicine.
| Treatment Component | Description | Benefits |
|---|---|---|
| Surgical Stabilization | Surgery to stabilize the spine | Prevents further injury, promotes healing |
| Physical Therapy | Rehabilitation exercises | Improves mobility, strength, and function |
| Pain Management | Medications and interventions for pain | Enhances quality of life, reduces discomfort |
Thoracic Injuries (T6-T12): Lower Thoracic Region
The T6-T12 area of the thoracic spine is key for many body functions. Injuries here can deeply affect us. We’ll look at how these injuries impact trunk stability, breathing, and the risk of autonomic dysreflexia.
Impact on Trunk Stability and Balance
Injuries in the lower thoracic area can really mess with our balance and stability. The thoracic spine is essential for supporting our torso and keeping us upright. When T6 to T12 gets hurt, people might see:
- Less muscle power in the belly and lower back
- Bad proprioception (knowing where our body parts are)
- Trouble staying balanced, especially when sitting or standing
Rehab programs aim to strengthen spine muscles and improve proprioception. This helps with stability and balance.
Respiratory Function in Lower Thoracic Injuries
The thoracic spine is connected to breathing because it supports the rib cage. Injuries between T6 and T12 can mess with breathing, but not as much as higher injuries. Important points include:
- Diaphragm or accessory muscles might get weaker
- Lung capacity might drop because of less chest room
- There’s a higher chance of breathing problems like pneumonia
Respiratory therapy is key in rehab for lower thoracic injury patients.
Autonomic Dysreflexia and Management
Autonomic dysreflexia (AD) is a serious condition that can happen in people with spinal cord injuries at or above T6. It causes very high blood pressure suddenly. To manage it, we do:
- Quickly find and fix what’s causing the problem (like a full bladder)
- Put the head of the bed up to lower blood pressure
- Give antihypertensive meds if blood pressure is too high
Learning to spot AD signs and how to act is vital for those with T6-T12 injuries and their caregivers.
Lumbar and Sacral Injuries: Lower Spinal Cord
The lumbar and sacral parts of the spine are key to many body functions. Injuries here can cause big problems. We’ll look at how these injuries affect the body, including symptoms and how they impact different functions.
Lumbar Injuries: Functions and Symptoms
Lumbar injuries happen in the lower back. They can cause a variety of symptoms, based on the injury’s severity and location. Common symptoms include pain, numbness, and weakness in the legs. We’ll dive into the functions affected by lumbar injuries and the symptoms people often face.
Lumbar injuries can affect many bodily functions, including:
- Motor control: Lumbar injuries can make it hard to walk or move the legs.
- Sensation: Patients might feel numbness or tingling in the legs.
- Reflexes: Lumbar injuries can mess with reflexes, causing odd responses.
| Lumbar Injury Level | Functions Affected | Common Symptoms |
|---|---|---|
| L1-L2 | Hip flexion, knee extension | Pain, numbness in the legs |
| L3-L4 | Knee extension, ankle dorsiflexion | Weakness, tingling sensations |
| L5-S1 | Ankle dorsiflexion, toe movement | Numbness, difficulty walking |
Sacral Injuries: Bowel, Bladder, and Sexual Function
Sacral injuries can seriously affect bowel, bladder, and sexual functions. We’ll talk about how sacral injuries impact these important functions and look at management options.
Sacral injuries can lead to:
- Bowel dysfunction: Patients might have trouble with constipation, fecal incontinence, or bowel movements.
- Bladder dysfunction: Sacral injuries can cause urinary retention, incontinence, or trouble with urination.
- Sexual dysfunction: Patients may face erectile dysfunction or a decrease in libido.
Cauda Equina Syndrome
Cauda equina syndrome is a serious condition where nerves in the spinal canal get compressed. This leads to significant symptoms. We’ll cover the causes, symptoms, and treatment options for cauda equina syndrome.
Cauda equina syndrome can be caused by:
- Herniated discs
- Spinal stenosis
- Trauma or injury
Quick medical attention is key to managing cauda equina syndrome and preventing long-term damage.
Advanced Treatment Approaches for Spinal Cord Injuries
We’ve looked at how spinal cord injuries affect people. Now, let’s talk about new treatments that are changing how we care for these patients.
Acute Care and Surgical Interventions
Quick care and surgery are key in treating spinal cord injuries. Surgery can fix the spine, ease pressure, and keep vertebrae stable. We use advanced methods like spinal fusion and decompression to help patients recover.
Rehabilitation and Functional Electrical Stimulation
Rehabilitation helps patients get back to living independently. Functional electrical stimulation (FES) is used to make muscles work and improve movement. FES is part of our rehab to help patients recover and adapt.
Effective Pain Management
Managing pain is vital for spinal cord injury patients. We use neurostimulation and other methods to control pain and improve life quality. Our goal is to support patients in their recovery journey and help them reach their best outcomes.
FAQ
What are the different levels of spinal cord injuries?
Spinal cord injuries can happen at different levels. These include cervical (C1-C7), thoracic (T1-T12), lumbar (L1-L5), and sacral (S1-S5) regions. Each level affects different parts of the body.
What is the difference between complete and incomplete spinal cord injuries?
Complete spinal cord injuries mean no function below the injury site. Incomplete injuries, however, cause partial loss of function. Some sensation or movement is still possible.
What are the symptoms of a C5 vertebrae injury?
A C5 vertebrae injury can limit arm and shoulder function. It may also affect breathing. Arms and legs might experience paralysis or weakness.
How do T1 spinal cord injuries affect upper body function?
T1 spinal cord injuries impact the upper thoracic region. They can affect hand function and dexterity. But they usually preserve arm and shoulder function.
What is T3 paraplegia, and what are its characteristics?
T3 paraplegia is paralysis or weakness below the T3 level. It can limit or remove control over abdominal muscles. This affects trunk stability and balance.
How do lumbar and sacral injuries impact bowel, bladder, and sexual function?
Lumbar and sacral injuries can harm bowel, bladder, and sexual function. They might cause incontinence, constipation, or erectile dysfunction.
What is cauda equina syndrome, and how is it related to spinal cord injuries?
Cauda equina syndrome is caused by nerve compression or damage in the lower spine. It can lead to pain, numbness, or weakness in the legs. It also affects bowel and bladder function.
What are the treatment approaches for high cervical injuries?
High cervical injuries are treated with stabilization, surgery, and rehabilitation. The focus is on keeping respiratory function and managing complications.
How do advanced treatment approaches, such as functional electrical stimulation, help spinal cord injury patients?
Treatments like functional electrical stimulation can restore muscle function. They improve mobility and enhance quality of life for spinal cord injury patients.
What is the impact of spinal cord injury levels on functional ability?
The level of spinal cord injury greatly affects functional ability. Higher injuries usually result in more extensive paralysis or weakness.
How do lower thoracic injuries affect trunk stability and balance?
Lower thoracic injuries can weaken abdominal muscles. This affects trunk stability and balance. It impacts posture, mobility, and overall function.
What is autonomic dysreflexia, and how is it managed in spinal cord injury patients?
Autonomic dysreflexia is a serious condition in spinal cord injury patients, especially those with injuries above T6. It’s managed by quickly recognizing and treating triggers, like pain or pressure sores.