Aortic stenosis is a life-threatening heart condition. It happens when the aortic valve gets narrower, often because of calcium buildup or birth defects. At Liv Hospital, we’ve seen how untreated aortic stenosis can cause serious problems and even death.
Understanding the risks and prognosis of aortic stenosis is key. We aim to offer top-notch heart care. It’s important to teach patients about the dangers of this condition and why they should see a doctor if they notice symptoms.
Key Takeaways
- Aortic stenosis is a progressive condition that can lead to fatal complications if left untreated.
- Recognizing the risks and prognosis is critical for timely medical intervention.
- Liv Hospital is dedicated to providing internationally recognized, patient-focused cardiac care.
- Understanding the condition and its impact on patients is essential for effective management.
- Timely intervention can significantly improve patient outcomes.
Understanding Aortic Stenosis: A Progressive Valve Disease
It’s key to know about aortic stenosis to handle its growth and risks. This condition makes the aortic valve narrow, blocking blood flow. It can cause heart failure and even sudden death.
Definition and Basic Pathophysiology
Aortic stenosis narrows the aortic valve opening, blocking blood flow. It’s often caused by thickened and calcified valve leaflets. This makes it hard for blood to flow.
The disease’s causes are complex, involving genetics, environment, and blood flow. As the valve narrows, the heart works harder. This can lead to thickening of the left ventricle and heart failure if not treated.
Key factors contributing to the pathophysiology include:
- Valve calcification and thickening
- Increased resistance to blood flow
- Left ventricular hypertrophy
- Potential progression to heart failure
Types of Aortic Stenosis
Aortic stenosis can be classified by its cause and severity. The main types are:
- Calcific Aortic Stenosis: Common in adults, linked to aging and valve calcification.
- Congenital Aortic Stenosis: Present at birth, caused by valve malformations like a bicuspid valve.
- Rheumatic Aortic Stenosis: Caused by rheumatic fever, leading to scarring and narrowing.
Knowing the type and severity of aortic stenosis is vital. It helps choose the right treatment and manage symptoms well.
Causes and Risk Factors of Aortic Stenosis
It’s important to know the causes and risk factors of aortic stenosis. This helps in early detection and managing the disease. Aortic stenosis is caused by a mix of genetic, environmental, and lifestyle factors.
Age-Related Calcification
Age is a big factor in aortic stenosis. As we get older, calcium builds up on the aortic valve. This makes the valve stiff and narrow. It’s like the buildup in coronary arteries.
Research shows that this buildup is a major cause of aortic stenosis. It’s more common in people over 65.
Congenital Malformations
Born with a bicuspid aortic valve is another risk factor. This is when the valve has only two cusps instead of three. It can lead to valve problems, including stenosis, over time.
People with a bicuspid valve are more likely to get aortic stenosis younger. This is compared to those with a normal tricuspid valve.
Other Contributing Factors
Other factors also play a role in aortic stenosis. These include:
- High blood pressure: It can make the heart work harder, damaging the valve.
- Abnormal lipids: High levels of certain lipids, like LDL cholesterol, can contribute to aortic stenosis.
- Diabetes: It increases the risk of aortic stenosis. This might be because of its effects on inflammation and blood vessels.
- Chronic kidney disease: People with this condition are at higher risk. It could be due to kidney disease’s impact on heart health.
Knowing these causes and risk factors is key. It helps identify those at high risk. This way, we can take steps to prevent and treat the disease.
The Progression from Aortic Valve Sclerosis to Stenosis
It’s important to know how aortic valve sclerosis turns into stenosis. This knowledge helps in early treatment. Aortic valve sclerosis makes the valve thick and hard, leading to stenosis.
Early Stage: Aortic Valve Sclerosis
Aortic valve sclerosis is a step before stenosis. In this stage, the valve gets thick and might have calcium. But, the valve opening is not too small yet. We’ll look at how it gets worse and what affects it.
This early stage might not show symptoms, so watching it closely is key. As it gets worse, the chance of getting stenosis goes up.
Transition to Stenosis
Going from sclerosis to stenosis means more calcium and scarring on the valve. This makes the valve opening smaller. It blocks blood flow, causing chest pain, shortness of breath, and fainting.
Things like age, high blood pressure, and family history can make it worse. Knowing these risks helps manage the condition better.
Why Natural Reversal Is Impossible
Once sclerosis turns into stenosis, it can’t go back on its own. The damage from calcium and scarring can’t be undone without help. We’ll talk about the treatments available and what they mean.
Doctors can help manage symptoms and slow the disease. But, surgery or a new valve might be needed to fix the valve.
| Stage | Characteristics | Symptoms | Treatment Options |
|---|---|---|---|
| Aortic Valve Sclerosis | Thickening and calcification of valve leaflets | Often asymptomatic | Monitoring, risk factor management |
| Aortic Stenosis | Narrowing of the valve opening due to calcification and fibrosis | Chest pain, shortness of breath, fainting | Surgical or transcatheter valve replacement |
Recognizing Symptoms of Aortic Stenosis
It’s important to know the symptoms of aortic stenosis early. This can help get the right treatment quickly. Knowing these symptoms can make a big difference in how well the disease is managed.
Classic Symptom Triad
The main symptoms of aortic stenosis are chest pain (angina), shortness of breath (dyspnea), and fainting (syncope). These signs show the disease is there and getting worse.
- Chest Pain (Angina): This happens when the heart muscle doesn’t get enough oxygen-rich blood, usually when you’re active.
- Shortness of Breath (Dyspnea): At first, it happens when you’re active. But as the disease gets worse, it can happen even when you’re sitting or lying down.
- Fainting (Syncope): Fainting can happen when there’s a drop in blood flow to the brain, often when you’re doing something active or excited.
Additional Warning Signs
There are other symptoms to watch for too. These include:
- Fatigue and weakness
- Palpitations or irregular heartbeats
- Swollen ankles and feet due to fluid buildup (edema)
When Symptoms Indicate Severity
The symptoms you have can tell you how serious aortic stenosis is. As it gets worse, symptoms get stronger and harder to handle.
| Symptom | Indication |
|---|---|
| Chest Pain | Increased demand for oxygen, reduced supply |
| Shortness of Breath | Reduced cardiac output, possible heart failure |
| Fainting | Reduced blood flow to the brain, critical stenosis |
It’s key for both patients and doctors to understand these symptoms. Spotting them early and treating them right can change the disease’s path.
How Does Aortic Stenosis Kill You: The Deadly Mechanisms
It’s important to know how aortic stenosis can be deadly. This valve disease can cause serious problems if not treated right.
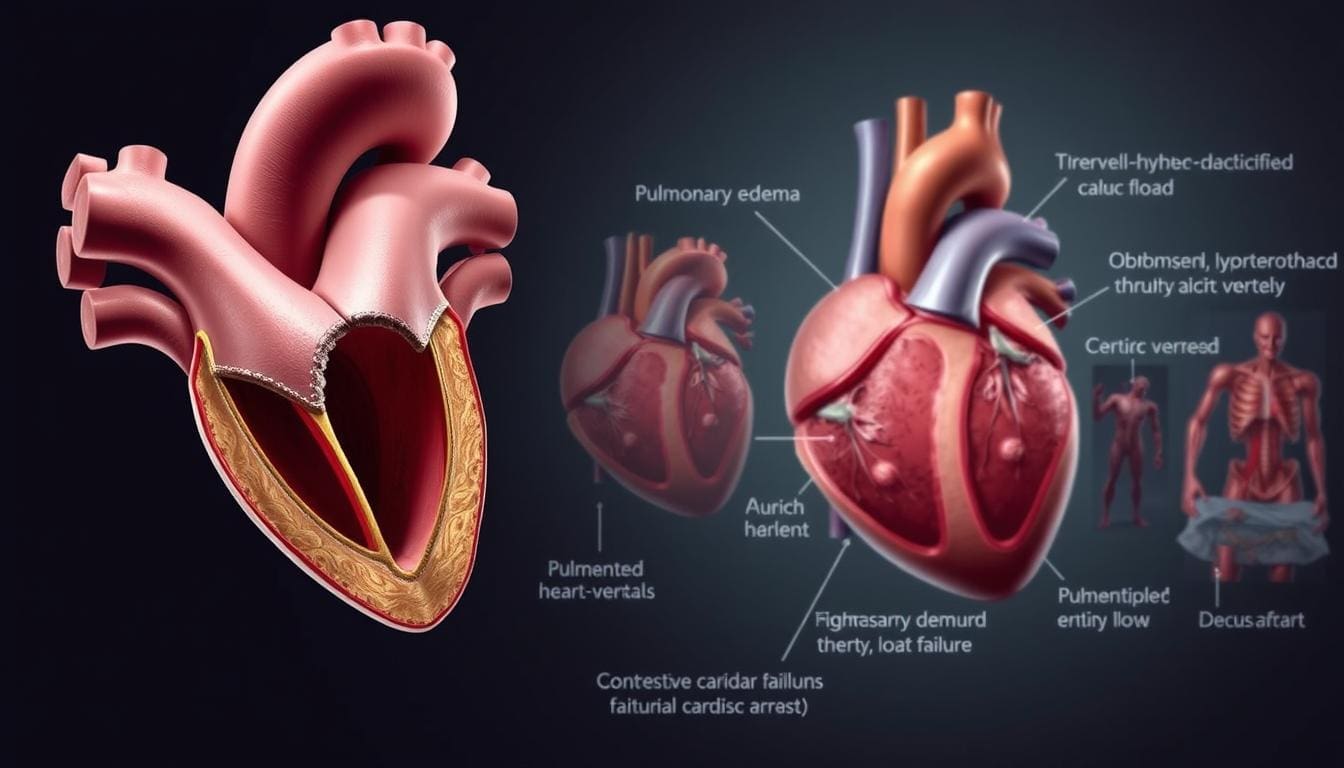
Sudden Cardiac Death
Patients with severe aortic stenosis face a big risk of sudden cardiac death. The narrowed valve can block blood flow, causing fatal heart problems.
Heart Failure Progression
As aortic stenosis gets worse, it can lead to heart failure. This means the heart can’t pump enough blood, making things worse for the patient.
Fatal Arrhythmias
Fatal arrhythmias are another danger of aortic stenosis. The disease can mess with the heart’s electrical system, causing dangerous heart rhythms.
Hemodynamic Collapse
In advanced stages, aortic stenosis can cause a sudden drop in blood pressure. This can lead to a lack of blood flow to important organs, which can be fatal.
The table below shows the deadly ways aortic stenosis can harm patients.
| Deadly Mechanism | Description | Impact on Patient Outcomes |
|---|---|---|
| Sudden Cardiac Death | Obstruction of blood flow leading to cardiac arrest | High risk of mortality |
| Heart Failure Progression | Inability of the heart to pump enough blood | Worsening prognosis |
| Fatal Arrhythmias | Disruption of the heart’s electrical system | Life-threatening irregular heartbeats |
| Hemodynamic Collapse | Sudden drop in blood pressure | Inadequate blood flow to vital organs |
A cardiologist, once said,
“The key to managing aortic stenosis is early detection and timely intervention to prevent these deadly mechanisms from occurring.”
We stress the need to understand these risks. This helps us give the right care and support to patients with aortic stenosis.
The Aortic Stenosis Death Spiral Explained
The term “aortic stenosis death spiral” refers to a dangerous sequence of complications in advanced valve disease. It’s important to grasp the mechanisms and their impact on patient outcomes.
Initiating Factors
The death spiral starts with valve narrowing, putting strain on the heart. This strain comes from several factors, including:
- Severe valve calcification
- Progressive valve obstruction
- Inadequate compensatory mechanisms
As the valve narrows, the heart works harder to pump blood. This sets the stage for more problems.
Cascade of Complications
The death spiral leads to a series of complications, including:
- Heart Failure: The heart’s increased workload can lead to failure, as it can’t keep up with the obstruction.
- Arrhythmias: The heart strain can cause dangerous arrhythmias, worsening heart function.
- Hemodynamic Instability: Decreased cardiac output can lead to instability, causing low blood pressure and poor organ perfusion.
These complications can worsen cardiac function and overall health in complex ways.
Point of No Return
There’s a point where complications become irreversible, marking a critical turning point. At this stage, even with treatment, the patient’s outlook worsens significantly.
Understanding the aortic stenosis death spiral is key for both clinicians and patients. It stresses the need for early intervention and close monitoring of disease progression.
Heart Failure: The Primary Killer in Aortic Stenosis
Heart failure is a major problem in aortic stenosis, affecting how well patients do. It’s important to know how heart failure happens and what it means for patients.
Pressure Overload and Ventricular Remodeling
The aortic valve gets narrower in aortic stenosis. This blocks the left ventricle’s outflow, causing pressure overload. The ventricle tries to adapt by changing its shape, known as ventricular remodeling.
At first, this helps the heart keep pumping. But over time, it can make the ventricle work less well.
Diastolic and Systolic Dysfunction
Aortic stenosis can also cause diastolic and systolic dysfunction. Diastolic dysfunction makes it hard for the ventricle to relax and fill. Systolic dysfunction means the ventricle can’t contract well to push blood out.
This makes it hard for the heart to meet the body’s needs. Symptoms like shortness of breath and swelling show the disease is getting worse.
Signs of Developing Heart Failure
It’s important to spot signs of heart failure early. Look for:
- Shortness of breath on exertion or at rest
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Persistent cough or wheezing
- Rapid weight gain due to fluid retention
As
“Heart failure is a complex clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood.”
, catching it early and treating it right is key to better outcomes.
Understanding heart failure in aortic stenosis helps doctors manage it better. This can improve patients’ lives and outcomes.
Left Ventricular Hypertrophy: Why the Heart Enlarges
As aortic stenosis gets worse, the heart grows thicker. This is called left ventricular hypertrophy. It helps the heart work harder but can also harm it.
Compensatory Mechanism
Left ventricular hypertrophy helps the heart deal with high pressure. The heart gets thicker to push blood through the narrowed valve. This helps keep the heart working well and prevents symptoms early on.
When Compensation Becomes Detrimental
But, left ventricular hypertrophy can hurt the heart over time. The thick walls make it harder for the heart to fill with blood. This can cause symptoms like shortness of breath and chest pain. These symptoms can really affect a person’s life.
- Reduced chamber size can limit ventricular filling.
- Impaired diastolic function can lead to heart failure symptoms.
- Increased myocardial oxygen demand can cause angina.
Relationship to Sudden Death
Left ventricular hypertrophy also raises the risk of sudden death in aortic stenosis patients. The thick heart is more likely to have dangerous heart rhythms. It’s important to watch and manage left ventricular hypertrophy to avoid such risks.
We must remember that left ventricular hypertrophy is a response to help the heart. But, we need to manage it carefully to avoid serious problems.
Dangerous Arrhythmias in Aortic Stenosis
Arrhythmias are a common and serious problem in aortic stenosis. They can be deadly if not managed well. It’s important to know how arrhythmias affect patient outcomes.
Types of Arrhythmias
Aortic stenosis can cause different arrhythmias. These include atrial fibrillation, ventricular tachycardia, and bradyarrhythmias. These issues can greatly affect a patient’s life and future.
- Atrial fibrillation: A common arrhythmia that can lead to decreased cardiac output.
- Ventricular tachycardia: A potentially life-threatening condition requiring immediate attention.
- Bradyarrhythmias: Abnormally slow heart rhythms that can necessitate pacemaker implantation.
Mechanisms Behind Electrical Disturbances
Arrhythmias in aortic stenosis come from changes in the heart. These changes include:
- Left ventricular hypertrophy, which can alter electrical conduction pathways.
- Increased myocardial fibrosis, leading to areas of electrical scar tissue.
- Changes in ion channel function, affecting the heart’s electrical activity.
Risk Assessment
Figuring out who might get arrhythmias involves looking at several things. These include how bad the valve stenosis is, if symptoms are present, and how well the left ventricle works. Finding out who’s at high risk helps with early treatment.
Key risk factors include:
- Severe aortic stenosis
- Symptoms such as syncope or heart failure
- Reduced left ventricular ejection fraction
Diagnosing Aortic Stenosis: From Symptoms to Confirmation
To diagnose aortic stenosis, we use a detailed approach. This includes physical exams, imaging, and tests. We’ll walk you through how we confirm this condition.
Physical Examination Findings
The physical exam is key in diagnosing aortic stenosis. We look for specific signs. These include:
- A harsh systolic murmur best heard at the right second intercostal space
- Delayed or diminished carotid pulses
- Evidence of heart failure, such as peripheral edema or jugular venous distension
These signs lead us to use more tests to confirm the diagnosis.
Imaging and Diagnostic Tests
We use several tests to confirm aortic stenosis and its severity. These include:
- Echocardiography: The main tool, showing valve details, stenosis level, and heart function.
- Electrocardiogram (ECG): Looks for heart rhythm issues or left ventricular hypertrophy.
- Cardiac Catheterization: An invasive test for coronary anatomy and valve function.
- Computed Tomography (CT) Scan: Helps see valve calcification and plan treatments.
Severity Classification
We classify aortic stenosis severity based on certain criteria. These include:
- Peak aortic jet velocity
- Mean pressure gradient across the aortic valve
- Aortic valve area
Knowing the severity helps us choose the right treatment and predict outcomes.
By combining physical exams with advanced tests, we accurately diagnose and assess aortic stenosis. This guides us in managing the condition effectively.
Treatment Options and Their Impact on Survival
Managing aortic stenosis requires different treatment strategies. Each option has its own effect on patient outcomes. It’s important to know their benefits and limits in improving survival rates.
Limitations of Medical Management
Medical management is often the first step for patients with aortic stenosis. This is true for those who are asymptomatic or have mild symptoms. But, it’s key to remember that medical therapy alone can’t stop the disease from getting worse or fix valve damage.
We mainly focus on managing symptoms and related conditions like high blood pressure and heart failure. Medications like diuretics, ACE inhibitors, and beta-blockers can help ease symptoms and improve life quality. Yet, these treatments can’t fix the valve stenosis in severe cases.
Surgical Valve Replacement
Surgical aortic valve replacement (SAVR) is the main treatment for severe aortic stenosis. It involves replacing the diseased valve with a prosthetic one through open-heart surgery. SAVR greatly improves survival and life quality for patients with severe symptoms.
The choice between mechanical and bioprosthetic valves depends on several factors. These include patient age, lifestyle, and the risk of anticoagulation therapy. Mechanical valves last longer but need lifelong anticoagulation. Bioprosthetic valves have a shorter lifespan but usually don’t need long-term anticoagulation.
Transcatheter Aortic Valve Replacement (TAVR)
TAVR is a new treatment for aortic stenosis, mainly for high-risk or inoperable patients. It involves placing a bioprosthetic valve in the native aortic valve via a catheter.
TAVR has been shown to lower mortality and improve symptoms in high-risk patients. Advances in TAVR technology and techniques are making it suitable for more patients.
Choosing the Right Intervention
Choosing the best treatment for aortic stenosis depends on several factors. These include symptom severity, valve anatomy, patient health, and overall health status. A heart team approach is essential in deciding the best treatment for each patient.
We must consider the immediate risks and benefits of each treatment. We also need to think about their long-term effects on survival and quality of life. The following table summarizes the key aspects of the treatment options discussed:
| Treatment Option | Key Benefits | Major Limitations |
|---|---|---|
| Medical Management | Symptom alleviation, manageable for mild cases | Cannot halt disease progression, limited in severe cases |
| Surgical Valve Replacement (SAVR) | Significantly improves survival, durable | Requires open-heart surgery, risk of complications |
| Transcatheter Aortic Valve Replacement (TAVR) | Minimally invasive, reduces mortality in high-risk patients | Limited durability data, possible vascular complications |
Understanding the strengths and limitations of each treatment helps tailor our approach to individual needs. This improves survival and quality of life for those with aortic stenosis.
Conclusion: Understanding Prognosis and Improving Outcomes
Knowing about aortic stenosis prognosis and treatment is key to better patient care. Almost 10% of adults over 80 have it, with a 50% death rate in two years without treatment. Symptoms like chest pain, heart failure, and fainting usually start after 50.
When symptoms appear, the outlook for severe aortic stenosis is grim. Survival rates at five years vary from 15-50%. Certain factors like clinical signs, echocardiography, and exercise tests predict outcomes. High levels of natriuretic peptides also signal worse results. For more on managing aortic stenosis, check out aortic stenosis prognosis.
After a successful aortic valve replacement, patients often see big improvements in symptoms and life quality. Long-term survival can be similar to the general population for older patients. A thorough approach, including early diagnosis and proper treatment, is essential for better outcomes.
What is aortic stenosis?
Aortic stenosis is a disease where the aortic valve gets narrower. This blocks blood flow from the heart to the body.
How does aortic stenosis progress?
It starts with the valve becoming stiff and calcified. Then, the opening gets so narrow that blood flow is severely blocked.
What are the symptoms of aortic stenosis?
Symptoms include chest pain, shortness of breath, and fainting. Other signs are fatigue, palpitations, and trouble exercising.
How does aortic stenosis lead to death?
It can cause sudden death, heart failure, fatal arrhythmias, and hemodynamic collapse. These are serious complications.
What is the aortic stenosis death spiral?
It’s a series of complications that worsen as the disease progresses. Eventually, it becomes too late to reverse the damage.
How is aortic stenosis diagnosed?
Doctors use physical exams, imaging, and tests like echocardiography and cardiac catheterization. These help diagnose the condition.
What are the treatment options for aortic stenosis?
Treatments include medication, surgery, and TAVR. The best option depends on the severity and the patient’s health.
Can aortic stenosis be reversed?
No, it can’t be reversed naturally. Treatments can help symptoms and survival, but the condition itself is permanent.
What is the role of heart failure in aortic stenosis?
Heart failure is a major complication. It happens when the heart works too hard due to the valve problem. This leads to heart damage.
How does left ventricular hypertrophy relate to aortic stenosis?
It’s a response to high pressure on the heart. But, too much of it can be harmful and increase the risk of sudden death.
What are the arrhythmias associated with aortic stenosis?
Aortic stenosis can cause arrhythmias like atrial fibrillation and ventricular tachycardia. These increase the risk of sudden cardiac death.
What is the prognosis for patients with aortic stenosis?
The outlook depends on the severity, symptoms, and treatment. Knowing this helps improve patient outcomes.
References
PubMed (NCBI): Unspecified Article on Cardiology (Specific PubMed ID)
Clinical Medicine Journals: International Journal of Clinical Cardiology Article (Specific Journal/Page)