Aortic stenosis is a serious heart condition. If not treated, it can lead to severe complications. Early detection is key to manage the condition and prevent further damage.
At Liv Hospital, our trusted specialists focus on patient-centered cardiac care. We follow the latest medical guidelines to protect your heart and well-being. It’s important to recognize the signs of heart valve disease for timely diagnosis and management.
We know how critical it is to spot aortic stenosis symptoms early. Our cardiac services are designed to support international patients seeking advanced medical treatments.
Key Takeaways
- Early detection of aortic stenosis is vital for effective management.
- Liv Hospital offers complete cardiac care services.
- Recognizing symptoms of heart valve disease is essential.
- Patient-centered care is our main focus at Liv Hospital.
- Advanced medical treatments are available for international patients.
What is Aortic Stenosis?
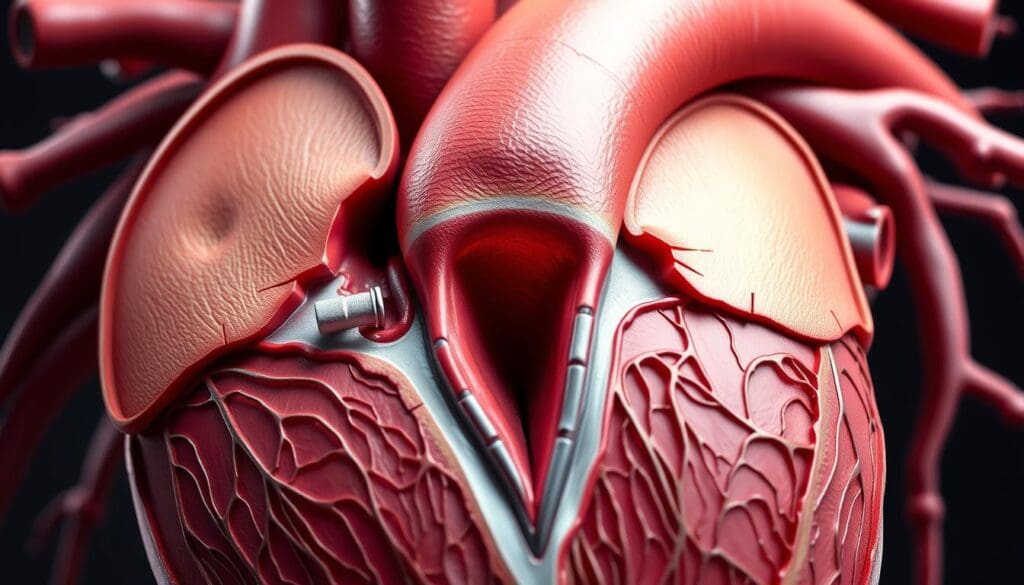
Aortic stenosis is when the aortic valve gets narrower. This blocks blood flow from the heart’s left ventricle to the aorta. It’s a serious heart disease that needs treatment.
The Narrowing of the Aortic Valve
The aortic valve is key for blood flow to the body. In aortic stenosis, it narrows, often because of calcium buildup or birth defects. This narrowing stops blood from flowing right, making the heart work harder.
How Aortic Stenosis Affects Heart Function
Aortic stenosis makes the heart’s left ventricle work too hard. The narrowing forces the heart to pump blood with more pressure. This can make the ventricle walls thicken over time.
This can lead to less blood being pumped and symptoms like chest pain, shortness of breath, and tiredness. Knowing how aortic stenosis affects the heart is key to finding the right treatment.
Types and Stages of Aortic Stenosis
It’s important to know the different stages and types of aortic stenosis. This condition makes the aortic valve narrow, affecting the heart and overall health.
Mild, Moderate, and Severe Classifications
Aortic stenosis is divided into mild, moderate, and severe based on its severity. The severity is measured by the valve area and the pressure gradient. Mild aortic stenosis has a valve area over 1.5 cm² and a low pressure gradient. On the other hand, severe aortic stenosis has a valve area under 1.0 cm² and a high pressure gradient, showing a serious blockage.
The severity of aortic stenosis determines the treatment. Mild cases might need just monitoring. But severe cases often require surgery or a new valve.
Different Types Based on Cause and Onset
Aortic stenosis can also be classified by its cause and when it starts. The main types are:
- Calcific aortic stenosis: This is common in older adults, caused by calcium deposits on the valve.
- Congenital aortic stenosis: It’s present at birth due to valve structure issues.
- Rheumatic aortic stenosis: It’s caused by rheumatic fever, leading to valve scarring and narrowing.
Knowing the specific type and cause of aortic stenosis helps tailor treatments. Recognizing heart valve disease signs and understanding aortic stenosis stages is key for better care.
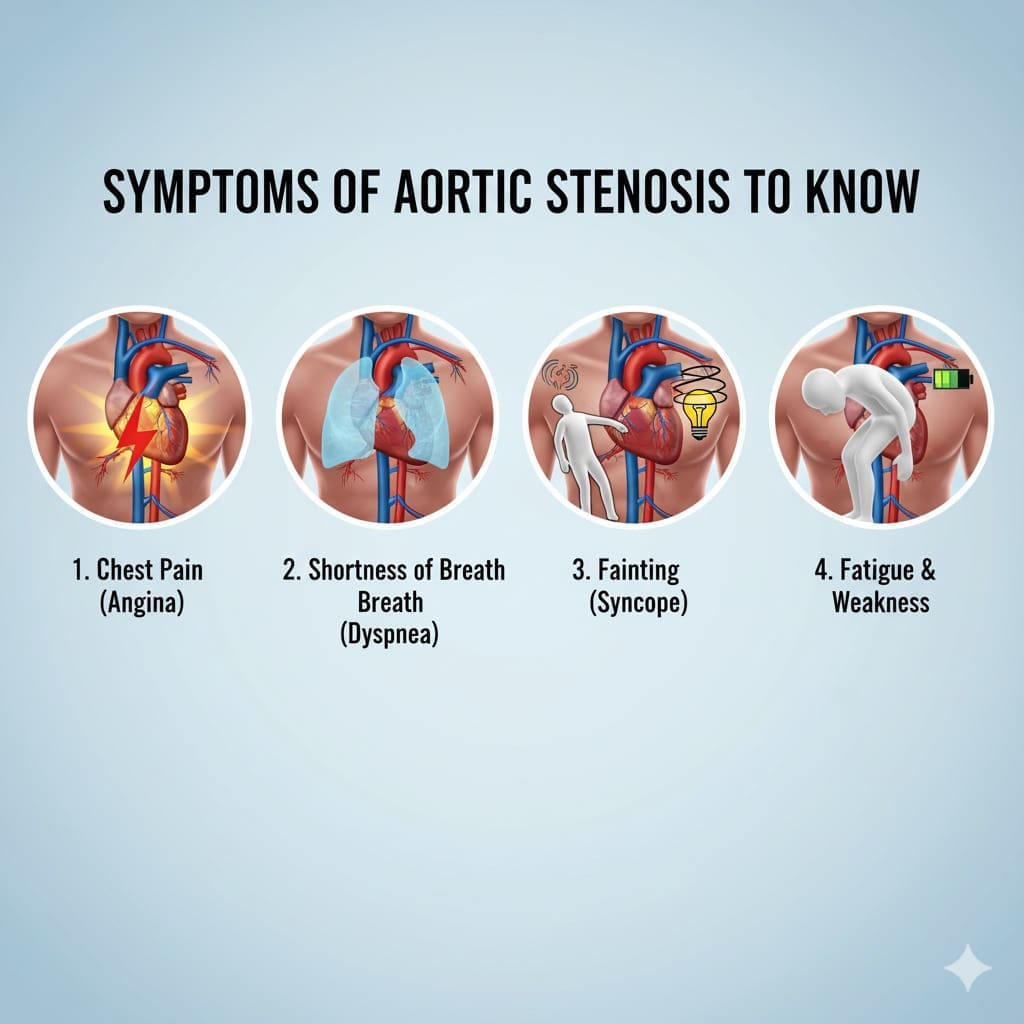
Recognizing Aortic Stenosis Symptoms: What to Watch For
Spotting aortic stenosis symptoms early can greatly help treatment. Aortic stenosis happens when the aortic valve gets narrower. This blocks blood flow from the heart to the rest of the body. We’ll talk about common symptoms and why they often show up late.
Why Symptoms Often Appear Late
Aortic stenosis can grow slowly. The heart tries to work harder to get around the narrowed valve. This means symptoms like chest pain and shortness of breath might show up later.
Because aortic stenosis gets worse slowly, people might not notice it until it’s serious. Regular health checks are key to catching heart problems early.
The Importance of Early Detection
Finding aortic stenosis early is key to managing it well. If symptoms are caught early, doctors can start treatment. This can really improve life quality and outcomes.
Now, let’s look at common symptoms of aortic stenosis and what they mean:
| Symptom | Description | Implication |
|---|---|---|
| Chest Pain | Pain or discomfort in the chest due to reduced blood flow | May indicate severe aortic stenosis |
| Shortness of Breath | Difficulty breathing, specially during activity | Can signify advanced disease |
| Fatigue | Feeling tired or weak due to reduced cardiac output | Can impact daily activities |
Spotting these symptoms early can lead to quick medical help and treatment. We urge people to know these signs and get medical help if they notice them.
Symptom 1: Chest Pain and Angina
Chest pain is a key symptom of aortic stenosis, often linked to angina. This pain happens because the aortic valve narrows, blocking blood flow. The heart muscle then doesn’t get enough oxygen, mainly when you’re active or stressed.
The pain from aortic stenosis feels like pressure or tightness in the chest. It can spread to the arms, back, neck, jaw, or stomach. Remember, this pain is not just uncomfortable. It’s a warning sign of a serious issue that needs a doctor’s check-up.
The Mechanism Behind Stenosis-Related Chest Pain
The reason for chest pain in aortic stenosis is complex. Reduced valve area and increased resistance to blood flow cause high pressure in the left ventricle. This pressure and the heart’s need for oxygen can lead to angina or chest pain, more so when you’re active.
Also, the narrowed valve can cause left ventricular hypertrophy. This is when the left ventricle’s muscle wall gets thicker. This thickening makes it harder for the heart to pump blood to the coronary arteries, adding to the angina.
When to Seek Medical Attention
If you’re feeling chest pain or discomfort, get medical help right away. Not all chest pain is from aortic stenosis, but any new or worsening pain needs a doctor’s check. They can find out what’s causing it and how to treat it.
- Seek immediate medical help if you experience sudden, severe, or prolonged chest pain.
- If your chest pain is accompanied by other symptoms such as shortness of breath, dizziness, or fainting.
- If you have a history of heart disease or risk factors for cardiovascular disease.
Getting a diagnosis and treatment early can greatly improve your chances of recovery from aortic stenosis. If you’re feeling symptoms or worried about your heart, talk to your doctor without delay.
Symptom 2: Shortness of Breath During Activity
Many people with aortic stenosis struggle with shortness of breath when they’re active. This is because their heart isn’t working as well as it should. The aortic valve getting narrower means the heart has to work harder to push blood through.
This extra effort can make it harder for the heart to keep up with the body’s needs when we’re moving around. It’s like trying to run a marathon with a heavy backpack.
How Valve Narrowing Affects Breathing
The aortic valve getting smaller blocks the normal flow of blood. This forces the heart to work even harder to get blood to the rest of the body. Over time, this can make the heart muscle thicker and even lead to heart failure if not treated.
When the heart can’t pump well, fluid can build up in the lungs. This makes it hard to breathe and can cause shortness of breath.
Progressive Nature of Breathing Difficulties
At first, shortness of breath might only happen when you’re really exerting yourself. But as aortic stenosis gets worse, it can happen even when you’re just sitting or lying down. It’s important for people to watch their symptoms and tell their doctor if anything changes.
Getting help early can really improve life for those with heart valve disease. It helps manage symptoms and can even save lives.
Understanding the progression of symptoms like shortness of breath is key to managing aortic stenosis. By catching signs early and getting medical help, patients can find relief and live healthier lives.
Symptom 3: Fatigue and Weakness
Fatigue is a common symptom in people with aortic stenosis. It happens because the heart can’t pump enough blood. This makes it hard to do everyday things.
Reduced Cardiac Output and Energy Levels
The aortic valve gets narrower in aortic stenosis. This blocks blood flow from the heart. The heart then works harder, leading to reduced cardiac output.
This means the body’s tissues and muscles don’t get enough oxygen and nutrients. This causes fatigue and weakness.
A cardiologist, says, “Fatigue in aortic stenosis shows the heart is struggling.” It affects not just the body but also mental health.
Distinguishing from Other Causes of Fatigue
Fatigue is common in many conditions. But in aortic stenosis, it’s a big warning sign. We look for other symptoms like chest pain or shortness of breath to confirm it.
Fatigue in aortic stenosis is not just feeling tired. It’s a constant lack of energy that doesn’t get better with rest.
If you’re always tired and have other symptoms like dizziness, see a doctor. They can check if it’s aortic stenosis or something else.
- Knowing the signs of aortic stenosis, like fatigue, is key for early treatment.
- Understanding how reduced cardiac output affects energy levels helps manage the condition better.
Symptom 4: Fainting or Near-Fainting Episodes (Syncope)
Fainting or near-fainting, known as syncope, is a worrying sign of aortic stenosis. It happens when blood flow to the brain drops, often due to hard work in those with severe aortic stenosis. We’ll look into why syncope happens in aortic stenosis and the risks involved.
Syncope in aortic stenosis is linked to a narrowed aortic valve. This valve blockage makes it hard for blood to flow from the heart. When you exert yourself, your body needs more blood, but the valve can’t keep up. This leads to low blood pressure and might cause you to faint.
Why Aortic Stenosis Causes Syncope
Syncope in aortic stenosis is caused by the heart’s inability to pump more blood during effort. This is because the valve is blocked. The heart’s output doesn’t rise, causing blood pressure to drop. This can lead to fainting. Knowing this helps identify who’s at risk.
Risk Factors for Syncope in Valve Disease
Several factors make syncope more likely in aortic stenosis. These include:
- Severe aortic stenosis
- History of syncope or near-syncope episodes
- Presence of other cardiovascular diseases
- Low blood pressure
- Dehydration or conditions leading to decreased blood volume
It’s key to spot these risk factors to manage aortic stenosis well. By knowing the causes and risks of syncope, doctors can take steps to prevent fainting. This helps improve patient care and outcomes.
Symptom 5: Heart Palpitations and Irregular Heartbeats
Heart palpitations are symptoms of aortic stenosis. They make you feel your heartbeat, which might seem irregular or too strong. These feelings can be due to arrhythmias, caused by the heart’s strain from the condition.
Arrhythmias Associated with Aortic Stenosis
Aortic stenosis puts extra work on the heart. This can make the heart muscle thicken. This thickening can mess up the heart’s electrical signals, causing arrhythmias.
Some common arrhythmias include:
- Atrial fibrillation: an irregular and often rapid heart rhythm
- Ventricular tachycardia: a fast heart rate that originates in the lower chambers of the heart
- Other arrhythmias that may cause symptoms like palpitations, dizziness, or shortness of breath
Monitoring and Managing Palpitations
Managing heart palpitations means watching symptoms and treating the cause. Patients should keep a diary of when and how long palpitations last. This helps track any triggers.
Monitoring strategies include:
- Regular check-ups with a healthcare provider to monitor the progression of aortic stenosis and the occurrence of arrhythmias.
- Electrocardiogram (ECG) tests to assess the heart’s electrical activity.
- Holter monitoring or event monitoring to capture arrhythmias over a longer period.
Management of palpitations may involve treating the underlying aortic stenosis, as well as specific treatments for arrhythmias. This can include medications to control heart rate or rhythm, or procedures like cardioversion to restore a normal heart rhythm.
Understanding and managing heart palpitations can greatly improve life for those with aortic stenosis.
Symptom 6: Heart Murmur – A Diagnostic Clue
Heart murmurs are abnormal sounds heard during a heartbeat. They are key in diagnosing aortic stenosis. These sounds come from turbulent blood flow or vibrations in the heart.
A heart murmur linked to aortic stenosis is a harsh sound. It’s heard at the right second intercostal space. The sound’s intensity can change, often getting louder with actions that boost heart output.
Characteristics of Aortic Stenosis Murmurs
The murmur of aortic stenosis has unique traits that help doctors diagnose it. It’s a systolic murmur, happening when the heart contracts and pumps blood out.
Key Features:
- Typically harsh and of ejection quality
- Best heard at the right upper sternal border
- May radiate to the carotids or apex
- Intensity can vary with different maneuvers
How Physicians Evaluate Heart Sounds
Doctors listen to heart sounds with a stethoscope. They look for any irregularities. The presence, timing, and details of a murmur give important clues about the heart’s condition.
Clinical evaluation involves:
- Careful listening to the heart sounds
- Assessing the timing and characteristics of the murmur
- Correlating findings with other clinical data
Understanding heart murmurs linked to aortic stenosis helps us see how doctors diagnose this condition. It shows the importance of listening to heart sounds in medical diagnosis.
Symptom 7: Declining Exercise Tolerance and Quality of Life
Aortic stenosis makes it hard to do daily activities. It affects how well you can exercise and live your life. Patients struggle with tasks they used to do easily.
Impact on Daily Activities
The aortic valve gets narrower, making the heart work harder. This leads to fatigue and shortness of breath. Simple tasks like walking or doing chores become hard.
Patients may have to change their lifestyle a lot. They might reduce physical activities and avoid hard tasks. They might even need help with daily things.
Psychological Effects of Physical Limitations
Physical limits from aortic stenosis can really affect your mind. Patients might feel frustration, anxiety, and depression. They miss being independent and doing things they love.
Doctors should help with these mental issues too. They can offer counseling, support groups, and ways to stay mentally strong. This helps patients feel better, not just physically.
It’s key to understand all symptoms of aortic stenosis, like not being able to exercise well. By treating both body and mind, we can help patients live better lives.
Diagnosis and Treatment Options for Aortic Stenosis
Diagnosing and treating aortic stenosis needs a detailed plan. We use many tools and strategies to manage this condition.
Modern Diagnostic Techniques
Modern tools are key in finding and checking aortic stenosis. Echocardiography is the main tool, showing the heart’s details. It helps us decide the best treatment.
Cardiac MRI and CT scans might also be used. They give more info on the heart’s shape and how it works. This helps us understand the stenosis’s impact.
Medical Management Approaches
For mild or no symptoms, we start with medicine. We watch the condition closely and treat symptoms. Medicines help with high blood pressure or heart failure.
We also talk about lifestyle changes. Eating right and exercising help the heart. Regular check-ups are key to keep track of the disease and adjust treatment.
Surgical and Minimally Invasive Interventions
For severe cases, surgery or less invasive methods are needed. Aortic valve replacement (AVR) is a common surgery. It replaces the bad valve with a new one, improving life and survival.
Transcatheter aortic valve replacement (TAVR) is another option. It’s good for those at high risk for surgery. TAVR is done through small cuts, making recovery faster and risks lower.
We look at each patient’s situation to pick the best treatment. We consider symptoms, health, and what the patient wants.
Conclusion: Taking Action for Better Outcomes
It’s important to know the signs of aortic stenosis early. We talked about symptoms like chest pain, shortness of breath, and feeling tired. These signs can help improve treatment results.
At Liv Hospital, we focus on top-notch heart care. Our team uses the newest treatments for aortic stenosis. Early action can make a big difference in a patient’s life.
If you’re feeling these symptoms, don’t wait to see a doctor. Taking action early can lead to better health and a better life. Liv Hospital is ready to help, with world-class care for international patients.
What are the common symptoms of aortic stenosis?
Symptoms include chest pain, shortness of breath, and fatigue. Fainting or near-fainting episodes, heart palpitations, and heart murmurs are also common. Declining exercise tolerance is another symptom.
Why do symptoms of aortic stenosis often appear late?
Symptoms appear late because the heart tries to compensate for the narrowed valve. It takes time for the condition to progress to a point where symptoms are noticeable.
What is the significance of chest pain in aortic stenosis?
Chest pain in aortic stenosis is related to angina. It happens when the heart muscle doesn’t get enough oxygen-rich blood. This often occurs during physical activity or stress.
How does aortic stenosis cause shortness of breath?
The narrowing of the aortic valve reduces blood flow. This leads to increased pressure in the heart. Fluid buildup in the lungs results in shortness of breath during activity.
What is the relationship between aortic stenosis and fatigue?
Reduced cardiac output in aortic stenosis causes fatigue and weakness. The heart can’t pump enough blood to meet the body’s needs, making it hard to stay active.
Why does aortic stenosis cause fainting or near-fainting episodes?
Aortic stenosis can cause fainting or near-fainting episodes. This is due to reduced blood flow to the brain. It’s often triggered by physical activity or changes in posture.
What is a heart murmur, and how is it related to aortic stenosis?
A heart murmur is an abnormal sound heard when listening to the heart with a stethoscope. In aortic stenosis, it’s a systolic ejection murmur. It’s caused by turbulent blood flow across the narrowed valve.
How is aortic stenosis diagnosed?
Aortic stenosis is diagnosed with tests like echocardiography and electrocardiogram (ECG). Cardiac catheterization and imaging modalities like CT or MRI scans are also used.
What are the treatment options for aortic stenosis?
Treatment options include medical management and surgical aortic valve replacement. Minimally invasive procedures like transcatheter aortic valve replacement (TAVR) are also available. The choice depends on the severity and individual patient needs.
Can aortic stenosis be managed without surgery?
In some cases, aortic stenosis can be managed with medical therapy. But severe cases often require surgical intervention, like aortic valve replacement, to improve outcomes and quality of life.
What is the role of Liv Hospital in treating aortic stenosis?
Liv Hospital provides complete cardiac care for aortic stenosis. They have experienced cardiologists and cardiac surgeons. They offer personalized care to international patients.
References
American Academy of Family Physicians (AAFP) (Journal/Publication): Article on Aortic Stenosis (Specific Issue)
PubMed Central (NCBI): Management of Aortic Valve Stenosis (Specific PMC ID)
PubMed (NCBI): Review on Severe Aortic Stenosis (Specific PubMed ID)


































