Last Updated on November 26, 2025 by Bilal Hasdemir
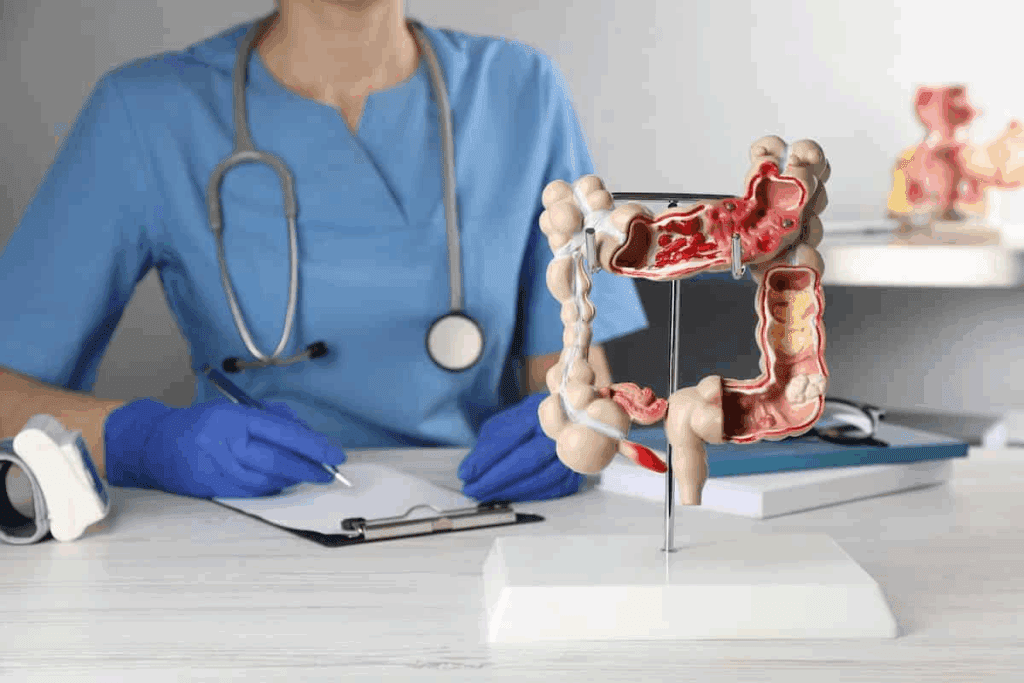
Choosing the right colon cancer surgery is key to effective treatment. At Liv Hospital, our team focuses on the patient. We use the latest protocols and approaches in our care. Learn key bowel tumor surgery types and how they remove colon and rectal cancer tumors.
The type of surgery for colorectal cancer varies based on the cancer’s location and size. Different bowel operations are used, like colectomy and local resection. These are often done with minimally invasive techniques.
Patients need to understand different surgical options. This helps them make informed decisions about their care.
Colorectal cancer is a common cancer worldwide. It needs a deep understanding of its treatments, like surgery. “The treatment of colorectal cancer is multifaceted, involving various modalities including surgery, chemotherapy, and radiation therapy,” say top oncologists.
Colorectal cancer is a big health problem globally. Its rates of occurrence and death vary by region. It’s a major cause of cancer deaths, showing the need for good treatments.
Risk factors like diet, lifestyle, and genes play a part in colorectal cancer. Early detection through screening can help, but many are diagnosed late.
Surgery is key to treating colorectal cancer, mainly for early-stage tumors. The decision to have surgery depends on the cancer’s stage, the patient’s health, and the tumor’s details.
For early-stage cancers, less invasive surgeries might be used. But, more complex cases might need bigger surgeries.
Choosing the right surgery depends on several things. These include the tumor’s location, size, and stage, and the patient’s health and wishes. New surgical methods, like robotic-assisted surgery and transanal approaches, offer more options for treating colorectal cancer.
A surgical oncologist says, “Using advanced surgical techniques can greatly improve patient outcomes. It can lead to faster recovery and fewer complications.”
Healthcare providers can tailor treatments based on these factors. This helps ensure the best possible results for patients with colorectal cancer.

To tailor the surgical strategy to the individual, a detailed pre-operative assessment is conducted, including cancer staging. This critical step in the management of bowel cancer influences both the surgical approach and patient outcomes.
Diagnostic procedures play a vital role in the pre-surgical assessment of colon cancer. These include colonoscopy, which allows for the visualization of the tumor, and biopsy, which confirms the presence of cancer cells. Imaging tests such as CT scans and MRI are also critical for assessing the extent of the disease.
The TNM staging system is used to define colon cancer, providing a standardized way to describe the extent of the disease. This system considers the size and extent of the main tumor (T), the degree to which nearby lymph nodes (N) are affected, and whether the cancer has metastasized (M). Accurate staging is essential for determining the most appropriate colon cancer operation procedure and predicting patient prognosis.
In addition to the TNM staging, imaging, and pre-operative evaluation are critical for planning bowel resection for cancer. Techniques such as ultrasound and PET scans provide valuable information on the tumor’s characteristics and possible spread. This thorough assessment enables surgeons to choose the most effective surgery to remove colon cancer, whether it’s a minimally invasive procedure or a more traditional open surgery.
By combining these diagnostic and staging tools, healthcare providers can develop a personalized treatment plan. This plan addresses the unique needs of each patient, ultimately improving outcomes for those undergoing colon cancer operation procedures.
Bowel tumor surgery includes many procedures for patients with colorectal cancer. The surgery type depends on the tumor’s stage, location, and size. It also depends on the patient’s health.
The way we treat bowel tumors has changed a lot. Now, there are many options for different needs. It’s important for patients and doctors to know about these surgeries.
Polypectomy removes polyps during a colonoscopy. It’s used for cancers or polyps that might become cancerous. Tools are used to cut or burn the polyp, and then it’s taken out.
Indications: Early-stage cancer or precancerous polyps.
Local excision removes the tumor and some tissue around it through the anus. It’s for small, early-stage tumors. This method is less invasive and can lead to fewer complications and a quicker recovery.
Benefits: Less invasive, potentially fewer complications, and quicker recovery.
Right hemicolectomy removes the right colon, including the tumor, and connects the rest of the colon. It’s for tumors in the ascending colon.
Left hemicolectomy is similar but removes the left colon. It’s for tumors in the descending colon. The goal is to remove the tumor, some healthy tissue, and lymph nodes.
Choosing the right surgery depends on many factors. These include the tumor’s location and the patient’s health. Other surgeries, like total colectomy, anterior resection, and abdominoperineal resection, also have their uses and benefits.
It’s key for patients to understand the different surgeries for bowel tumors. Each procedure has its own considerations and outcomes.
There are many ways to surgically treat colon cancer. The right method depends on the tumor’s size, location, and the patient’s health.
Open surgery for colon cancer means a big cut in the belly to reach the colon. It lets surgeons take out the tumor and nearby tissue directly. It’s used for bigger tumors or complex cases. Though it takes longer to heal than other methods, it’s a good choice for many.
Laparoscopic surgery, or keyhole surgery, uses small cuts in the belly. A thin tube with a camera and tools is used to remove the tumor. This method is less invasive, leading to faster healing and less pain. It’s as good as open surgery for early-stage colon cancer.
Robotic surgery is a minimally invasive method that uses a robotic system. It offers better 3D views and precise tools, making complex surgeries easier. It can lead to better results and faster recovery for some.
The results and healing times differ based on the surgery type. Minimally invasive methods like laparoscopic and robotic surgery have shorter stays and quicker healing. Here’s a quick comparison:
Choosing the right surgery should be a team decision. It depends on the patient’s needs and the tumor’s specifics.
Specialized techniques have changed how we remove bowel tumors. They offer better results for patients. These new methods aim to be more precise, cut down on recovery time, and make surgeries more effective for colon cancer.
Transanal Endoscopic Microsurgery (TEM) is a new way to remove early-stage rectal tumors. It uses a special endoscope inserted through the anus. This lets surgeons remove tumors with great accuracy.
Transanal Total Mesorectal Excision (TaTME) is an advanced technique. It combines transanal and laparoscopic methods to remove rectal tumors. This method allows for precise dissection around the rectum, potentially improving outcomes for patients with rectal cancer.
Key advantages of TaTME include better visualization and access to the rectal area. This is hard with traditional laparoscopic techniques. It leads to a more complete removal of the tumor and surrounding tissue.
Combined Endoscopic-Laparoscopic Surgery is a hybrid approach. It uses both endoscopic and laparoscopic techniques to remove colon tumors. This method combines the strengths of both, making the procedure more precise and safe.
These specialized techniques in bowel tumor removal are always getting better. Ongoing research aims to improve their effectiveness and safety. So, patients having colon tumor removal surgery can expect better results and a quicker return to normal life.
It’s important for patients with colorectal cancer to know about ostomy creation. An ostomy, or stoma, is a surgical opening in the abdomen for waste. It’s needed when part of the colon or rectum must be removed due to cancer.
There are two main types of ostomies: temporary and permanent. Knowing the difference helps patients understand their recovery and future.
Temporary ostomies help the bowel heal after surgery. They can be closed once healing is done. Permanent ostomies are needed when a lot of the colon or rectum must be removed.
Some patients find managing a stoma easier than pre-surgery bowel issues. They might choose a permanent stoma with their healthcare team’s advice.
There are two main types of ostomies: colostomy and ileostomy. A colostomy opens the colon, while an ileostomy opens the ileum (the small intestine’s end).
Good ostomy care is key to a good quality of life. This includes:
Patients with ostomies can live active lives with proper care. Knowing about ostomy creation during surgery helps them make informed treatment choices.
Bowel surgery is a key cancer treatment but comes with risks. It’s important for patients and doctors to know these risks. This helps in making the right choices for bowel cancer surgery treatment.
Right after bowel surgery, patients might face infections, bleeding, or bad reactions to anesthesia. These are common with any surgery. But they can be lessened with good care before and after surgery.
| Complication | Description | Mitigation Strategy |
| Infection | Bacterial infection at the surgical site | Prophylactic antibiotics, wound care |
| Bleeding | Hemorrhage during or after surgery | Careful surgical technique, monitoring |
| Adverse Reaction to Anesthesia | Reaction to anesthesia used during surgery | Pre-operative assessment, anesthesia monitoring |
After surgery for bowel cancer, patients might face bowel changes like diarrhea or constipation. They could also have nutritional issues. These can really affect their loyalty.
Having an ostomy, either temporary or permanent, is another long-term issue. Patients need to learn about ostomy care and management to adjust to these changes.
To lower the risks of complications of bowel surgery, several steps can be taken. Choosing the right patient and preparing them well before surgery is key. This includes improving their nutrition, managing health issues, and making sure they understand the surgery’s risks and benefits.
Using advanced surgical methods, like minimally invasive surgery, can also help. It can make recovery faster and might reduce complication risks. A team approach to care, involving surgeons, oncologists, and others, is vital for the best results.
Recovering from colon cancer surgery is a key part of the healing process. It needs careful attention and following the doctor’s advice. Thanks to new ways of managing bowel surgery, removing tumors is now more effective, and recovery times are shorter.
The first steps of recovery happen in the hospital. Doctors watch over patients closely. How long you stay in the hospital depends on the surgery type and your health.
Right after surgery, care focuses on managing pain, watching for complications, and starting with liquids and then solid foods. “The quality of post-operative care can significantly influence the patient’s recovery trajectory,” say experts.
What you eat is very important after bowel surgery. At first, you might only have liquids, then move to solid foods as your body heals.
Eating a balanced diet full of nutrients helps your body heal. It’s also key to drink plenty of water and avoid foods that could upset your stomach or cause problems.
Moving around is also vital for recovery. Rest is needed right after surgery, but slowly starting to move helps prevent problems and speeds up healing.
Start with simple activities like walking and gradually do more as you get stronger and more energetic.
Regular check-ups with doctors are a big part of getting better. These visits help watch for any signs of cancer coming back and solve any issues or worries.
Tests and exams are part of follow-up care to make sure the cancer hasn’t come back and you’re healing properly. “Follow-up care is not just about monitoring; it’s also about supporting the patient’s overall well-being and quality of life,” says a doctor.
In summary, recovery after bowel surgery needs a team effort. It includes good hospital care, eating right, slowly getting back to physical activities, and regular doctor visits. Knowing these steps helps patients on their road to recovery.
Personalized bowel surgery is a big change in treating colon cancer. It fits each patient’s needs. It looks at the disease stage, patient health, and what they want for surgery.
Choosing the right surgery for bowel cancer involves many factors. These include how far the cancer has spread, the patient’s health, and surgery risks.
What the doctor and patient want also matters. Shared decision-making helps make sure the treatment fits the patient’s needs and hopes.
A team of doctors is key in planning personalized bowel surgery. This team includes surgeons, oncologists, and radiologists. They work together to create the best treatment plans.
With their skills, they can handle complex cases. This team provides optimal care for patients having colon cancer surgery.
Personalized bowel surgery often mixes surgery with other treatments like chemotherapy and radiation. This mix can make treatment better and help patients recover faster. For example, chemotherapy before surgery can make tumors smaller.
Putting together different treatments needs careful planning. This way, doctors can make surgery more effective for each patient.
Recent improvements in bowel surgery have made it possible to remove tumors effectively. This has also led to shorter recovery times. Procedures like polypectomy, local excision, and hemicolectomy have greatly improved patient results.
New methods like laparoscopic and robotic-assisted surgeries have changed the game. These techniques have cut down on complications and sped up recovery. This is a big win for patients facing bowel tumor surgery.
The future of bowel tumor surgery looks bright. We can expect even more advanced technology and techniques. Personalized surgery plans, combining different treatments, will be key to better patient care.
Developing new surgical methods and tools is vital for colon cancer treatment. By expanding on current advancements, doctors can offer better care for those with bowel tumors.
Bowel tumor surgery is a procedure to remove tumors in the colon or rectum. It’s also known as colon cancer surgery.
There are several types of bowel tumor surgery. These include polypectomy, local excision, and right and left hemicolectomy. Other procedures like TEM and TaTME are also used.
A colectomy is a surgery to remove part of the colon. It’s often done to treat colon cancer or other colon issues.
Open surgery uses a big incision to access the colon. Minimally invasive surgery uses small incisions and special tools. It usually means a quicker recovery.
Robotic-assisted surgery is a minimally invasive method. It uses a robotic system to help the surgeon. This improves precision and visualization.
An ostomy creates an opening in the abdomen to divert stool or urine. It’s needed when part of the colon or rectum is removed or needs to be bypassed.
Complications can include infection, bleeding, and bowel obstruction. Long-term issues like changes in bowel habits or urinary function are also possible.
Recovery time varies based on the surgery type and individual factors. It usually takes several weeks to months.
After surgery, a specific diet is often recommended. This may include a liquid diet or low-fiber foods to manage bowel movements and comfort.
Yes, most patients can resume normal activities after surgery. Recovery time varies based on the surgery and individual factors.
A multidisciplinary team is key in cancer surgery. They include surgeons, oncologists, and radiologists. They work together to create a treatment plan for each patient.
Bowel resection is a surgery to remove the part with cancer. It’s often done to treat colon or rectal cancer.
The TNM system classifies colorectal cancer. It looks at the tumor size, lymph node involvement, and metastasis. It helps guide treatment.
This surgery combines endoscopy and laparoscopy. It’s used for early-stage cancers or polyps. It’s a specialized technique.
National Cancer Institute. (2025). Colorectal cancer treatment (PDQ®)–Health professional version. https://www.cancer.gov/types/colorectal/hp/colon-treatment-pdq
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!