Last Updated on November 26, 2025 by Bilal Hasdemir
It’s important to know how blood clot symptoms can change. At Liv Hospital, we focus on your safety and use proven treatments. This helps you understand and act on these important health signs. Understand can pain from a blood clot come and go and how to recognize DVT warning signs early.
Deep Vein Thrombosis (DVT) pain does not always follow a predictable pattern. Sometimes, it stays the same, and other times, it changes with how you move or what you do. It’s key to know the signs and when to get medical help.

It’s important to know about blood clots to spot their signs early. Blood clots are like gel clumps in veins or arteries. They can be deadly if not treated fast.
Blood clots form when the body tries to stop bleeding. This happens when it gets injured. Platelets, clotting factors, and other blood parts work together to make clots. Clots can form in different places, like the legs, arms, and lungs.
Two major types of blood clots are Deep Vein Thrombosis (DVT) and pulmonary embolism. DVT happens when a clot forms in deep leg veins. If a piece of this clot breaks off, it can go to the lungs. This can cause a pulmonary embolism, which is very dangerous. DVT and pulmonary embolism are serious conditions that require immediate medical attention.

Blood clot pain can be tricky because it sometimes seems to come and go. This makes it hard to diagnose because the pain isn’t always there. It’s important for both patients and doctors to understand why this happens.
The pain from blood clots, like Deep Vein Thrombosis (DVT), can change. It might not always be there. There are many reasons for this.
Several things can make blood clot pain change. These include:
Knowing these factors can help manage the condition better.
Research has given us important information about blood clot pain. Studies have found that DVT pain can be on and off. A study in the Journal of Thrombosis and Haemostasis showed that pain levels can change with activity and limb position.
By understanding these patterns and factors, doctors can give better diagnoses and treatments. This is key to improving patient care and reducing blood clot risks.
DVT pain has unique features that help doctors diagnose it. This pain is a key sign of a blood clot in the deep veins, usually in the legs.
DVT pain feels like a dull ache or cramping. It mainly occurs in the calf or thigh. Sometimes, it can spread across the whole limb. You might also see swelling, redness, or warmth in the affected area.
DVT pain can stay the same or change. Some people feel a constant ache. Others have pain that comes and goes. Many things can change how often you feel pain, like moving or changing positions.
A blood clot doesn’t always hurt. The pain can change, getting worse or better with activity. Some people might not feel much pain at all. It’s important to watch for other signs of DVT too.
Key characteristics of DVT pain include:
Knowing how position and movement affect blood clot pain is key to managing symptoms. Blood clots, like those in Deep Vein Thrombosis (DVT), can cause a lot of discomfort. This discomfort can change based on body position and how active you are.
When someone with DVT stands or walks, the pain from the blood clot can shift. Movement can sometimes make the pain worse by putting more pressure on the vein. But, some people find relief when they raise their legs or don’t put weight on the affected limb.
Finding the right way to sit or move can help ease blood clot pain. Some good ways include:
It’s important to talk to a healthcare professional. They can help find the best ways to manage blood clot pain for you.
It’s important to know the difference between blood clot pain and other conditions. This is because blood clot pain can be confused with many other issues. It’s hard to figure out what’s causing the pain.
Many conditions can look like blood clot pain in the legs. These include:
Each of these has its own signs that are different from blood clot pain.
Muscle cramps are sudden, intense pains that might seem like blood clot pain. But muscle cramps are usually:
Blood clot pain, on the other hand, lasts longer and doesn’t get better with simple stretches.
Chronic conditions like peripheral artery disease and chronic venous insufficiency can seem like blood clot pain. They often have:
But these symptoms start slowly and may come with other signs like skin changes or ulcers.
Blood clots can cause many symptoms that are important to notice. Pain is a big sign, but other symptoms can also help doctors diagnose.
Blood clots can make the affected limb look and feel different. You might see redness or color changes, feel warmth, and notice swelling. The skin might look tight and shiny, and the area could feel heavy or sore.
Some people think blood clots make the skin itch. But, itching is not usually a sign of a blood clot. If you itch, it might be because of swelling or inflammation, not the clot itself.
In serious cases, like with pulmonary embolism, you might feel symptoms all over. These can include shortness of breath, rapid heart rate, and lightheadedness. These signs need quick medical help because they can be very dangerous.
It’s key to know these extra symptoms for quick diagnosis and treatment. If you or someone else has these signs, getting medical help right away is vital.
A blood clot moving to the lungs is a serious emergency. It happens when a clot from the legs breaks loose and goes to the lungs. There, it blocks blood flow.
Symptoms of pulmonary embolism include sudden shortness of breath and chest pain. This pain gets worse when you breathe deeply. Coughing is another symptom. These signs need quick medical help.
Symptoms of pulmonary embolism can stay the same or change. This depends on the clot’s size and how much of the lung is affected.
The pain from pulmonary embolism is often sharp and stabbing. It might feel constant, but its intensity can change. Yet, any chest pain or trouble breathing is a sign to see a doctor right away.
Knowing the symptoms of pulmonary embolism and how they can change is key. If you think someone has it, call for emergency help.
Blood clot risk comes from medical, lifestyle, and genetic factors. Knowing these factors helps spot who’s at higher risk. It also guides how to prevent blood clots.
Some medical conditions raise blood clot risk. These include:
Lifestyle and environment also affect blood clot risk. These include:
| Factor | Description | Risk Level |
| Prolonged Immobility | Long periods of not moving, like on flights or in bed | High |
| Smoking | Smoking damages blood vessels and raises clot risk | High |
| Obesity | Being overweight puts more pressure on veins in legs and pelvis | Moderate to High |
Genetics can also increase blood clot risk. These include:
Knowing these risk factors helps take steps to avoid blood clots. If you’re worried, talk to your doctor.
Knowing when to get medical help for blood clots is key. Blood clots can cause serious problems like deep vein thrombosis (DVT) or pulmonary embolism. These need quick medical care.
Some symptoms mean you need to get help right away. Sudden shortness of breath, severe chest pain, or leg pain with swelling are signs. Doctors say, “Quick action can save lives.”
“Time is of the essence when dealing with possible blood clots; don’t delay seeking help.”
If you have symptoms that aren’t life-threatening but worry you, like mild leg pain or swelling, see a doctor. Your doctor can check you out and suggest the right treatment.
When you see a doctor, tell them about your symptoms. Say when they started and what makes them better or worse. Also, share any past health issues, like blood clots or surgeries. This helps your doctor figure out what’s wrong and how to fix it.
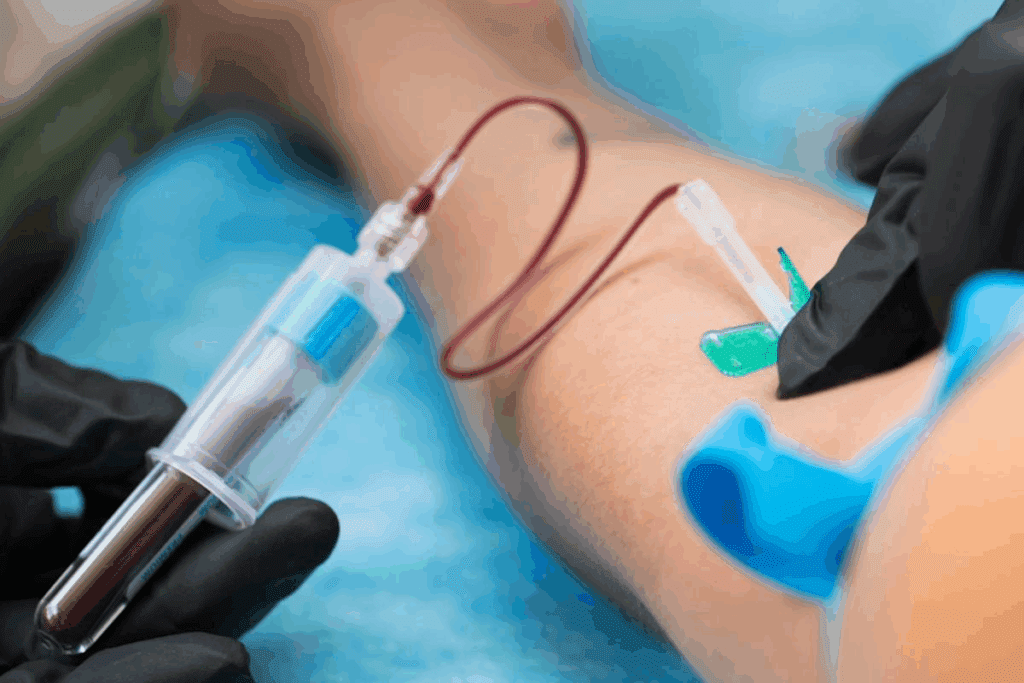
To find out if someone has a blood clot, doctors use many tests. They look at symptoms, do imaging tests, and run lab tests. This helps them see if there’s a clot and how big it is.
The first step is talking to the patient and doing a physical check. Doctors look for signs like pain, swelling, and redness. They also check for things that might make blood clots more likely.
Imaging tests are key in finding blood clots. Here are the main ones:
Laboratory tests help with imaging studies by checking blood and clotting factors. The main tests are:
By using all these tests together, doctors get a full picture of what’s going on. This helps them make a good plan to treat the patient.
There are many ways to treat blood clots, including medicine and procedures. Pain management is also key. These steps help avoid serious problems and ease pain.
Anticoagulant medicines stop clots from getting bigger and new ones from forming. Thrombolytics are for serious cases to break down clots. These are vital for treating deep vein thrombosis (DVT) and pulmonary embolism.
For very serious cases, doctors might use special procedures. These include using a catheter to send medicine to the clot or removing it mechanically.
Managing pain is very important. Doctors use medicines, elevate the limb, and use compression stockings. These help reduce swelling and pain.
Special centers offer cutting-edge treatments. They use new medicines and advanced procedures. These centers give complete care from start to finish, aiming for the best results.
Knowing about treatment and pain relief helps patients. It makes it easier to get through their care and recover.
Blood clot pain can be tricky to understand. It’s important to know about it to get help fast. The pain from blood clots, like deep vein thrombosis (DVT), can change. It depends on how you move and your position.
Knowing the signs of blood clots is key. These include pain, redness, warmth, and swelling. Tests like ultrasound and CT scans help find blood clots. Treatment can be medicines or procedures.
It’s important to know who’s at risk for blood clot pain. This includes medical conditions, lifestyle choices, and genetics. By knowing these risks and getting medical help when needed, you can lower your risk of problems from blood clots. Being aware and acting quickly is the best way to handle blood clot pain and related issues.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!