It’s important for patients and doctors to understand spinal procedures well. A kyphoplasty surgery video helps by showing the key steps in treating vertebral compression fractures. Watch our kyphoplasty surgery video. We explain the 7 essential steps of this powerful procedure for spine compression fractures.
Liv Hospital focuses on patient education in medical procedures. They break down the video kyphoplasty procedure into seven key steps. This helps patients understand the minimally invasive technique better, leading to safer care.
Key Takeaways
- Understanding the kyphoplasty procedure is key for patients and doctors.
- A kyphoplasty surgery video offers a clear guide to treating vertebral compression fractures.
- Liv Hospital puts patient education and safety first.
- The video kyphoplasty procedure is divided into seven essential steps.
- This technique is a safer option for treatment.
- Patient-centered care is promoted through educational resources.
Understanding Vertebral Compression Fractures
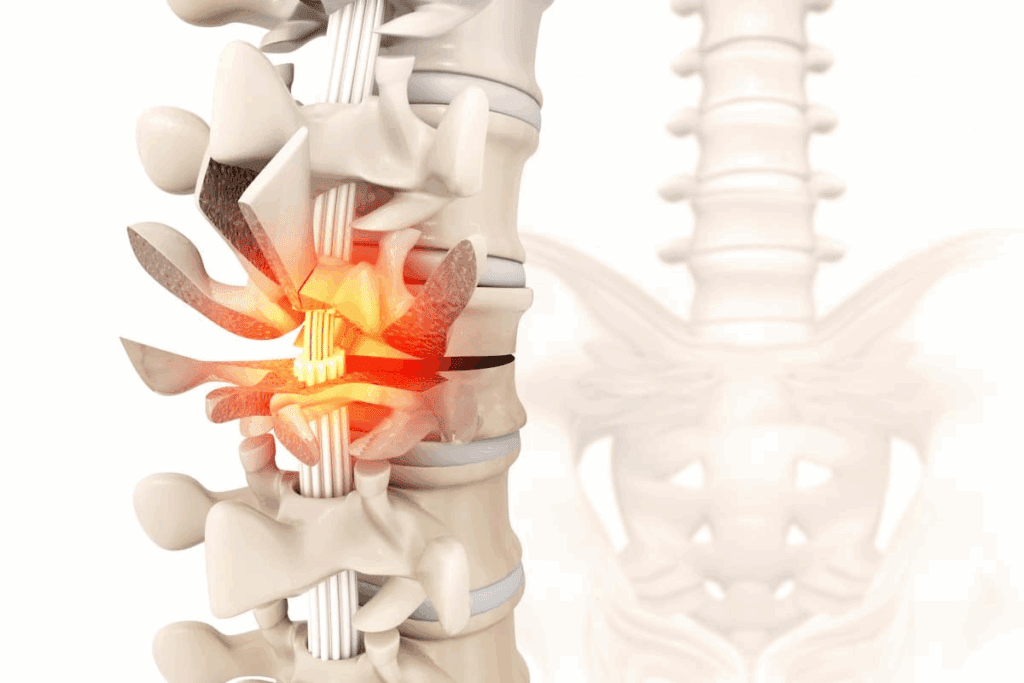
Vertebral compression fractures can really change a person’s life. They happen when a vertebra collapses. This can happen suddenly or slowly over time.
Common Causes of Vertebral Compression Fractures
The main reasons for these fractures are:
- Osteoporosis: This is when bones get weak, making them break easily.
- Trauma: Falls or accidents can cause these fractures.
- Cancer: Spinal tumors can weaken bones, leading to fractures.
Symptoms and Diagnostic Approaches
The signs of vertebral compression fractures vary. They often include:
- Severe back pain
- Loss of height
- Stooped posture or kyphosis
To diagnose these fractures, doctors use:
- X-rays
- MRI (Magnetic Resonance Imaging)
- CT (Computed Tomography) scans
Knowing the causes and symptoms early is key. It helps in managing and treating these fractures. This can lead to better results for patients, like those who get kyphoplasty.
What is Kyphoplasty Surgery?
Kyphoplasty surgery is a treatment for vertebral compression fractures. This happens when bones in the spine weaken, often due to osteoporosis or cancer. It causes the spinal bones to compress or collapse.
The procedure involves injecting bone cement into the fractured vertebra. This stabilizes it and helps restore its height. It also relieves pain and improves the patient’s quality of life.
Definition and Purpose
Kyphoplasty is a minimally invasive spinal procedure. It aims to stabilize and strengthen compressed vertebrae. The main goal is to relieve pain from vertebral compression fractures and restore the spine’s structure.
A study in the Journal of Neurosurgery: Spine found kyphoplasty improves vertebral height and reduces pain. This is in patients with osteoporotic compression fractures.
“Kyphoplasty is a valuable treatment option for patients with painful vertebral compression fractures… It provides immediate pain relief and improves functional outcomes.”
— Journal of Neurosurgery: Spine
Benefits of Minimally Invasive Approach
The minimally invasive nature of kyphoplasty offers several benefits:
- Reduced recovery time compared to traditional open surgery
- Less tissue damage and trauma to the patient
- Smaller incisions, resulting in less scarring
- Lower risk of complications
These advantages make kyphoplasty an attractive option. It offers effective pain relief with minimal disruption to daily life.
| Benefits | Description |
| Reduced Recovery Time | Patients can return to normal activities sooner |
| Less Tissue Damage | Minimally invasive technique reduces trauma |
| Smaller Incisions | Less scarring and reduced risk of infection |
How to Pronounce Kyphoplasty Correctly
Pronouncing medical terms correctly can be challenging. The correct pronunciation of “kyphoplasty” is ki-FOP-luh-stee. “Kypho-” refers to the curvature of the spine, and “-plasty” means molding or shaping. So, kyphoplasty means shaping or molding the curved spine to restore its original form.
Understanding the correct pronunciation is essential. It ensures clear communication between healthcare providers and patients. This reduces confusion and enhances the patient-provider relationship.
Indications and Patient Selection for Kyphoplasty
Kyphoplasty is effective in treating vertebral compression fractures when the right patients are chosen. This procedure, often done by interventional radiology (IR), helps reduce pain and stabilize the spine.
Ideal Candidates for the Procedure
Patients with painful vertebral compression fractures that haven’t improved with other treatments are good candidates. These fractures can make life very hard, causing a lot of pain and making it hard to move. Kyphoplasty works best for fractures that are less than 3 months old, helping to quickly ease pain and improve how well patients can move.
A leading doctor says, “Kyphoplasty has changed how we treat vertebral compression fractures. It’s a less invasive option that really helps the right patients.” This shows how important it is to pick the right patients for kyphoplasty to get the best results.
Contraindications and Risk Factors
Even though kyphoplasty is a good option for many, there are times when it’s not right. This includes severe vertebral collapse, infection, or big neurological problems. If a patient has these issues, they might not be a good fit for kyphoplasty, and other treatments should be looked into.
The use of percutaneous vertebral augmentation, including kyphoplasty, is also important. This method helps fix fractured vertebrae without a big surgery. Knowing when to use these treatments is key to giving patients the best care.
Pre-Procedure Preparation and Planning
Getting ready for kyphoplasty is key to its success. This step makes sure the procedure is done right and safely. It helps ensure the patient gets the best results.
Required Imaging Studies
Before starting kyphoplasty, doctors need to see the spine’s condition. They use X-rays, CT scans, or MRI scans for this. These tests show where the fracture is, how bad it is, and if there are other problems.
Choosing the right test depends on the patient’s needs and the doctor’s choice. A CT scan is great for bones, while an MRI scan looks at soft tissues and nerves.
Patient Preparation Guidelines
Getting ready for kyphoplasty is also important. Patients need to follow certain rules to stay safe and recover well. This includes stopping some medicines that might get in the way.
They also get advice on preoperative fasting and other steps. It’s vital for patients to listen to these tips and talk to their doctor about any worries.
For T12 kyphoplasty, planning is extra important. This is because the thoracolumbar area is complex and very important.
Kyphoplasty Surgery Video: Educational Resources
Kyphoplasty surgery videos are a great educational tool. They show the details of the procedure, from start to finish. They are very helpful for doctors and patients alike.
Benefits for Medical Professionals
Doctors find these videos very useful for learning and training. They let surgeons see the procedure up close. This helps them improve their skills and keep up with new methods.
Key benefits include:
- Enhanced understanding of the surgical technique
- Improved patient outcomes through better preoperative planning
- Continuing education for surgeons to stay updated with the latest techniques
Patient Education Through Video Content
Patients also gain a lot from these videos. They help patients understand what will happen during the procedure. This reduces worry and makes them more likely to follow their treatment plan.
Patient education videos can:
- Explain the kyphoplasty procedure in an easy-to-understand format
- Illustrate the expected outcomes and recovery process
- Address common questions and concerns
Finding Reliable Video Kyphoplasty Procedure Resources
It’s important to find trustworthy sources for kyphoplasty surgery videos. Doctors and patients should look for videos from well-known medical places or groups.
Tips for finding reliable resources:
- Check the credentials of the video producers
- Look for videos that are up-to-date with the latest techniques
- Verify the information against other credible medical sources
Kyphoplasty Anesthesia Options and Considerations
The choice of anesthesia in kyphoplasty is very important. It affects how comfortable the patient feels and how well the procedure goes. Kyphoplasty is used to fix compressed or fractured vertebrae. Choosing the right anesthesia is key to keeping the patient safe and comfortable.
Local Anesthesia Techniques
Local anesthesia is often used for kyphoplasty. It numbs the area where the procedure is done. This way, the patient can stay awake and alert. Local anesthesia techniques are safer and lead to quicker recovery times.
Using local anesthesia in kyphoplasty, like in L1 kyphoplasty, lets the patient give feedback in real-time. This can help avoid problems. But, it needs a patient who can cooperate and a skilled doctor.
General Anesthesia Applications
General anesthesia makes the patient unconscious during the procedure. It’s used for anxious patients or those who can’t stay in one place. General anesthesia helps the surgeon work more accurately.
But, general anesthesia has risks like breathing and heart problems. Choosing it should be based on the patient’s health and past medical history.
Patient-Specific Factors in Anesthesia Selection
Choosing the right anesthesia for kyphoplasty depends on several factors. These include the patient’s medical history, any health issues, and how anxious they are about the procedure.
| Factor | Consideration | Anesthesia Option |
| Medical History | Presence of comorbidities | Local or General |
| Anxiety Level | High anxiety | General |
| Procedure Complexity | Complex cases | General |
The table above shows important factors in choosing anesthesia for kyphoplasty. By looking at these factors, doctors can make the best choice for their patients. This helps ensure the best care and results.
The 7 Essential Steps of Kyphoplasty Procedure Explained
Knowing the steps of kyphoplasty is key for doctors and patients with vertebral compression fractures. This procedure is complex but aims to be less invasive than old surgical methods. It offers a big improvement for those needing relief.
Step 1: Patient Positioning and Preparation
The first step is getting the patient ready. They lie on a special table that lets doctors see inside with X-rays. Getting the patient right is important for safety and success.
Step 2: Access Point Identification
Next, doctors find the best spot to start the procedure. They use X-rays to guide them. The spot is chosen carefully to guide tools to the right vertebra.
Step 3: Needle Insertion Through Pedicle
Then, a needle goes through the vertebra’s pedicle. Doctors use X-rays to make sure it’s in the right place. Getting the needle right is key for the next steps.
Step 4: Guide Wire and Working Channel Placement
After the needle is in, a guide wire is put in, and the needle comes out. A channel is made for tools to follow the guide wire. This step is important for safe and effective bone cement placement.
The procedure keeps going with more steps that build on the first ones. Each step helps to make the vertebra stronger and more stable.
Understanding these steps helps doctors and patients know what to expect. Watching a kyphoplasty surgery video can help visualize these steps and learn more about the procedure.
Specific Techniques for Different Vertebral Levels
Kyphoplasty techniques change a lot depending on the vertebral level. This is because each part of the spine has its own challenges. Surgeons need to adjust their methods for the best results.
T12 Kyphoplasty Technique and Considerations
The T12 vertebra often gets compressed fractures. It’s at the edge of the thoracic and lumbar spine. The T12 kyphoplasty technique focuses on the pedicle size and where it is to avoid harming nearby nerves.
Knowing the T12 vertebra well is key for a successful kyphoplasty. The process includes:
- Placing the needle through the pedicle with precision
- Using a balloon to fix the fracture
- Adding cement to keep everything stable
L1 Kyphoplasty Approach and Challenges
L1 kyphoplasty is similar to T12 but has its own hurdles. The L1 vertebra faces a lot of stress because of its location. The L1 kyphoplasty method must consider the bigger size of the vertebra and the forces acting on it.
| Vertebral Level | Key Considerations | Technical Challenges |
| T12 | Transitional anatomy, pedicle size | Needle placement, cement leakage |
| L1 | Larger vertebral body, biomechanical stress | Fracture reduction, cement distribution |
Adaptations for Other Vertebral Segments
While T12 and L1 are common for kyphoplasty, other levels need special care. For example, the upper thoracic spine needs precise work because of small pedicles and nerves nearby. The lower lumbar spine has bigger vertebrae and different forces.
Success in kyphoplasty comes from knowing each spine segment’s unique features. By adjusting the technique for each level, surgeons can get better results and fewer problems.
Percutaneous Vertebral Augmentation: Technical Aspects
The technical side of percutaneous vertebral augmentation is key to kyphoplasty success. It uses advanced tools and precise imaging to get the best results.
Equipment and Specialized Tools
This procedure needs special tools like needles, guide wires, and systems for bone cement. The quality and accuracy of these tools are very important.
Key Equipment:
- Needles and cannulas for accessing the vertebral body
- Guide wires for precise placement
- Bone cement for vertebral augmentation
- Imaging equipment for real-time guidance
Imaging Guidance Methods
Imaging guidance is essential for percutaneous vertebral augmentation. Methods like fluoroscopy and CT guidance help doctors see the procedure live. This ensures the bone cement is placed correctly.
IR Kyphoplasty: Interventional Radiology Approach
Interventional radiology (IR) is very important in kyphoplasty, including percutaneous vertebral augmentation. IR specialists use their imaging skills for these precise, small procedures.
| Aspect | Description | Importance |
| Equipment | Specialized needles, guide wires, and bone cement | High |
| Imaging Guidance | Fluoroscopy, CT guidance for real-time visualization | Critical |
| IR Involvement | Expertise in minimally invasive interventions | Essential |
Kyphoplasty vs. Percutaneous Vertebroplasty
When looking at treatments for vertebral compression fractures, two options are often talked about: kyphoplasty and percutaneous vertebroplasty. Both help with pain and spine stability but work in different ways.
Procedural Distinctions and Techniques
Kyphoplasty uses a balloon to expand the fractured vertebra before cement is added. On the other hand, percutaneous vertebroplasty just injects cement directly into the vertebra without expanding it first. This difference in method can change how well each procedure works and what side effects might happen.
Key differences in technique:
- Kyphoplasty: Uses a balloon to expand the vertebra before adding cement.
- Percutaneous vertebroplasty: Just injects cement without expanding the vertebra first.
Comparative Clinical Outcomes
Both methods can greatly reduce pain. But kyphoplasty might do a better job of fixing the vertebra’s height and straightening it out. This choice can really affect how well a patient feels and their spine’s health over time.
Clinical outcomes to consider:
- Pain relief: Both are good at this.
- Vertebral height restoration: Kyphoplasty is better because of the balloon.
- Complication rates: Kyphoplasty might have fewer problems with cement leaking because of the balloon.
Selection Criteria for Each Procedure
Choosing between kyphoplasty and percutaneous vertebroplasty depends on several things. These include how bad the fracture is, if there’s a curve in the spine, and the patient’s overall health. Knowing these factors helps doctors make the best choice and helps patients understand their options.
| Criteria | Kyphoplasty | Percutaneous Vertebroplasty |
| Vertebral Height Restoration | Effective | Limited |
| Cement Leakage Risk | Lower | Higher |
| Procedure Time | Longer | Shorter |
In summary, both kyphoplasty and percutaneous vertebroplasty are good for treating vertebral compression fractures. But, their differences in how they work, their results, and who they’re best for need careful thought to give the best care.
International Perspectives and Success Rates
Globally, kyphoplasty is known for treating vertebral compression fractures well. It offers a lot of pain relief. This procedure is used all over the world, with changes to meet different needs and settings.
Kyphoplastie: International Applications and Variations
The term “Kyphoplastie” is another name for kyphoplasty in some places. The procedure has been changed in many countries to fit specific needs. For example, kyphoplasty anesthesia can vary, with some using local and others general anesthesia.
Studies worldwide show kyphoplasty works well for many patients. It’s flexible, allowing doctors to customize treatment for each patient.
Recent Research on Efficacy and Pain Relief
New studies back up kyphoplasty’s success in easing pain from vertebral compression fractures. They show it can greatly reduce pain and boost life quality. Video kyphoplasty procedure resources are helping teach doctors and patients about its benefits.
A key study in a top medical journal found kyphoplasty’s long-term benefits. It showed lasting pain relief and better mobility. This study highlights kyphoplasty’s role in managing vertebral compression fractures.
Long-term Outcome Studies
Long-term studies are key to understanding kyphoplasty’s lasting effects. They show the procedure’s benefits can last, with patients feeling less pain and moving better.
A detailed look at long-term data found kyphoplasty patients often have fewer complications and are happier. This supports using kyphoplasty for the right patients.
Conclusion: The Future of Kyphoplasty Procedures
Kyphoplasty has become a key treatment for vertebral compression fractures. It helps patients feel less pain and live better lives. A kyphoplasty surgery video shows how it’s done in a way that’s not too invasive.
Knowing how to say “kyphoplasty” is just the start. It’s also important to understand the details of the procedure. This is true for doctors and patients alike. As technology and techniques get better, kyphoplasty will likely become even more effective and safe.
Research and new methods are making kyphoplasty’s future look bright. Thanks to educational videos, both doctors and patients will keep benefiting from it. This makes kyphoplasty a vital part of treating vertebral compression fractures.
FAQ
What is kyphoplasty, and how does it differ from vertebroplasty?
Kyphoplasty is a procedure to fix and strengthen compressed vertebrae. It uses a balloon to lift the vertebra before adding cement. This is different from vertebroplasty, which just adds cement.
What are the benefits of watching a kyphoplasty surgery video?
Watching a kyphoplasty video can help you understand the procedure better. It shows the steps and techniques used in the surgery.
How is kyphoplasty pronounced?
Kyphoplasty is pronounced as “ky-foh-PLAS-tee.”
What are the indications for kyphoplasty?
Kyphoplasty is for people with painful fractures in their vertebrae. These fractures are often caused by osteoporosis or trauma.
What are the contraindications for kyphoplasty?
You shouldn’t have kyphoplasty if you have a vertebral infection or significant damage to your vertebrae. Certain types of fractures also make it unsuitable.
How is kyphoplasty performed under anesthesia?
Kyphoplasty can be done under local, general, or a mix of both anesthesia. The choice depends on the patient and the surgery’s complexity.
What is percutaneous vertebral augmentation?
Percutaneous vertebral augmentation includes procedures like kyphoplasty and vertebroplasty. They help stabilize and strengthen compressed vertebrae.
What is the role of interventional radiology in kyphoplasty?
Interventional radiology is key in kyphoplasty. It uses imaging to guide the placement of instruments and cement precisely.
How does kyphoplasty compare to percutaneous vertebroplasty in terms of clinical outcomes?
Both kyphoplasty and vertebroplasty can relieve pain. Kyphoplasty might also help restore vertebral height and reduce kyphosis.
What are the possible complications of kyphoplasty?
Kyphoplasty can lead to complications like cement leakage, infection, and nerve damage. But these are rare.
Can kyphoplasty be performed on different vertebral levels, such as T12 or L1?
Yes, kyphoplasty can be done on various levels, including T12 and L1. The technique is adjusted for each level’s anatomy and challenges.























