Last Updated on November 27, 2025 by Bilal Hasdemir
At Liv Hospital, we know how serious aortic thrombus is. It’s a blood clot in the aorta, the biggest artery in the body. This rare condition can cause big health problems if not treated right away.
We see how fast you need to get diagnosed and treated. Aortic thrombosis can show up in different ways, like mural or intramural thrombus. It needs a detailed care plan.
Our team is dedicated to top-notch healthcare for patients from all over. Knowing about aortic thrombus is key to managing it well.
It’s key to know about aortic thrombus to spot and treat it early. This serious issue happens when a blood clot forms in the aorta, the biggest artery in our body.
A blood clot forms in the aorta’s space, known as aortic thrombus. This can happen in different parts of the aorta. The abdominal aorta is a common spot, mainly because of atherosclerosis.
Aortic thrombus is not rare, and it’s serious because of its risks. These risks include embolization and damage to organs. It’s vital to diagnose and treat it quickly to avoid big health problems.
| Location | Prevalence | Common Complications |
|---|---|---|
| Abdominal Aorta | More common | Embolization, ischemia |
| Thoracic Aorta | Less common | Embolization, aortic dissection |
Understanding aortic thrombus is critical. It helps us give the right medical care and stop serious issues.
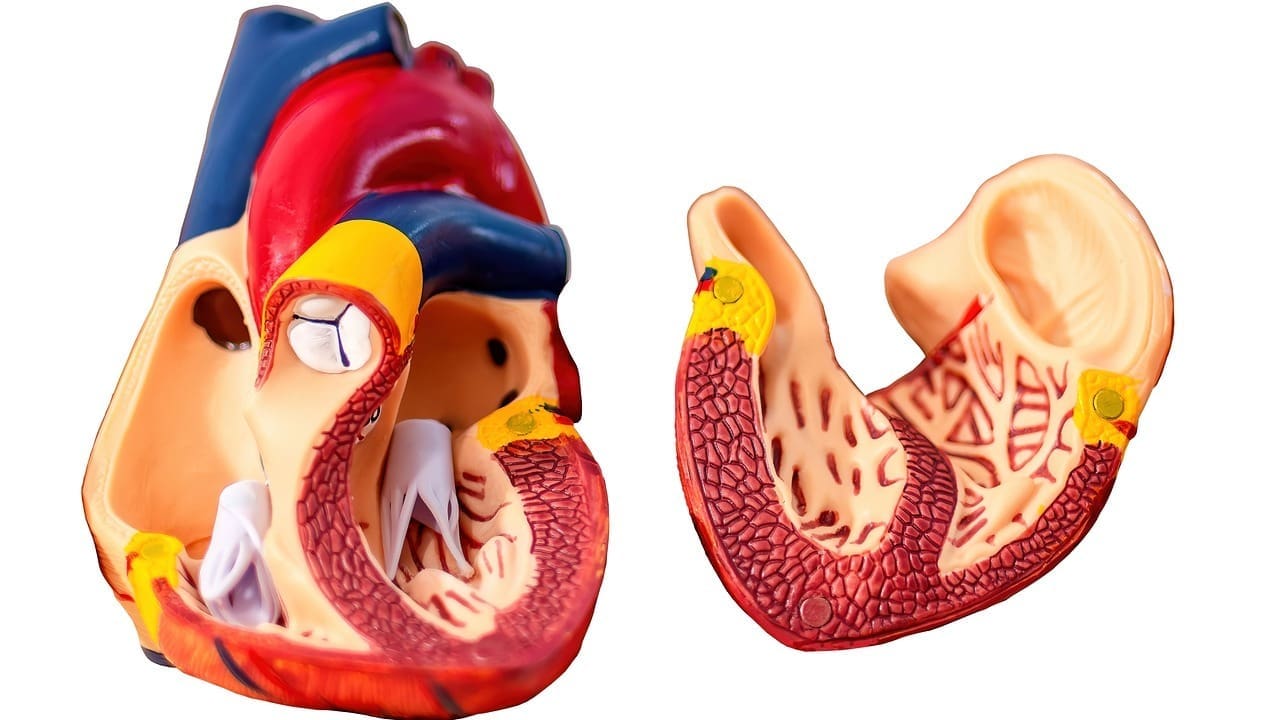
The aorta’s complex structure is key to understanding aortic mural thrombus formation. It’s the largest artery, carrying oxygenated blood to the body. It has different parts, each with its own role.
The aorta’s wall has three layers: the intima, media, and adventitia. The intima faces the blood. Damage here can start clotting. The media has smooth muscle and elastic fibers for flexibility. The adventitia supports the aorta and has nerves and blood vessels.
Knowing the structure and function of the aorta helps us see how clots can form. Its strength and elasticity are vital. But, high blood pressure, atherosclerosis, and trauma can harm it, leading to clots.
The formation of a mural thrombus aorta is complex. It starts with damage to the aorta’s lining. This damage can be from plaque, inflammation, or injury. When the lining is damaged, collagen is exposed, starting the clotting process.
Thrombus development in the aorta involves many factors. It’s not just about the aorta but also the body’s overall health. Knowing this helps us find ways to prevent and treat aorta mural thrombus.
It’s important to know about the different types and places where aortic thrombus can occur. This knowledge helps doctors diagnose and treat it better. Each part of the aorta has its own set of problems and solutions.
An abdominal aortic thrombus is a blood clot in the belly part of the aorta. It’s often linked to atherosclerosis, where arteries get clogged with plaque. This can lead to serious issues if not treated.
Thoracic aortic thrombus happens in the chest part of the aorta. It can be caused by injury, hypercoagulable states, or other factors that make blood clot more easily.
A mural thrombus sticks to the aorta’s wall. It’s a big worry, mainly when there’s an abdominal aortic aneurysm (AAA). It makes treatment harder.
Intramural thrombus forms inside the aorta’s wall. It’s often seen with aortic dissection or other problems that weaken the aorta’s wall.
Doctors need to know about the various types and locations of aortic thrombus. This knowledge helps them find the best treatments and improve patient care.
It’s important to know what causes an aortic thrombus to treat it well. Several main factors lead to the formation of an aortic clot.
Atherosclerosis is a big risk for an aortic thrombus. Plaque buildup in the aorta walls can cause clots. This happens when lipids, inflammatory cells, and fibrous elements gather, making it easy for clots to form.
Being in a hypercoagulable state raises the risk of aortic thrombosis. This can be due to genetic disorders, cancer, or certain medicines.
Damage to the aorta, from injury or medical procedures, can cause thrombus formation. Damage to the aorta’s lining starts the clotting process.
Cancer can make blood clotting more likely. It does this by making substances that help clots form and by pressing on or invading blood vessels.
The main reasons for aortic thrombus are complex and often linked. Knowing these causes is key to preventing and treating this condition.
Knowing the risk factors for aortic thrombus is key to catching it early and preventing it. We’ll look at how different factors raise the chance of getting this condition.
Age is a big risk factor for aortic thrombus, with older people more at risk. Research shows men are more likely than women, but women’s risk goes up after menopause. We need to think about these factors when we look at risk.
Chronic inflammatory conditions, like atherosclerosis, raise the risk of aortic thrombus. These conditions cause plaques and inflammation in the aortic walls. This makes it easier for clots to form.
Autoimmune disorders can also up the risk of aortic thrombosis. Conditions like antiphospholipid syndrome make it more likely for clots to form because of a hypercoagulable state.
Lifestyle choices, like smoking, obesity, and being inactive, increase the risk of aortic thrombus. These factors can make underlying conditions worse and raise the risk of vascular events.
It’s important to know the symptoms of aortic thrombus to get help quickly. The symptoms can change based on where and how big the clot is.
People with aortic thrombus might feel abdominal pain, back pain, and leg pain because of less blood flow. Sometimes, it can cause acute limb ischemia. This is when you have pain, look pale, have no pulse, feel cold, have numbness, and can’t move.
Some symptoms need help right away. Look out for sudden severe pain, loss of pulse in your limbs, or signs of organ failure. These signs mean you might have serious problems like embolization or a blocked aorta.
The spot where the thrombus is in the aorta affects the symptoms. For example, a clot in the abdominal aorta might cause belly pain and affect blood flow to your legs. On the other hand, a thoracic aortic thrombus could lead to chest or back pain.
At times, aortic thrombus doesn’t show symptoms and is found by accident during tests for other issues. We’ll look at how mural thrombus in AAA or intramural thrombus can be hard to spot, making diagnosis tricky.
Untreated aortic thrombus can cause severe and life-threatening problems. A thrombus in the aorta can block blood flow, leading to serious health issues.
One major risk of aortic thrombus is embolization. When a part of the thrombus breaks off, it can travel and block a smaller vessel. This can damage or even fail an organ, depending on where it lodges. For example, an embolus in a kidney vessel can cause kidney injury.
Aortic thrombus can also block the aorta, causing severe ischemia. This reduced blood flow can lead to tissue death and organ failure. The extent of ischemia depends on the thrombus’s size and location.
Untreated aortic thrombus can lead to long-term vascular problems. Chronic or recurring thrombi can cause the vessel wall to change. This can result in stenosis or weaken the vessel, increasing the risk of future heart problems.
Understanding the severe complications of aortic thrombus is key. Quick medical care is essential to prevent these issues and manage the condition well.
We use many tools to find aortic thrombus. These include imaging and lab tests. Finding it right is key for good treatment.
Imaging is key in finding aortic mural thrombus. We use different methods to see the aorta and find thrombi.
CT angiography is great for finding aortic thrombus. It shows the aorta and its branches well. This helps us know how big and where the thrombus is.
MRI and MRA give clear images of the aorta. They don’t use harmful radiation. These are good for people who can’t have CT scans.
Ultrasound is safe and easy to use. It’s good for finding aortic thrombus, mainly in the belly aorta. It’s often the first test because it’s safe and easy.
We also use laboratory tests and biomarkers to help find aortic thrombus. These tests help find problems that might cause the thrombus.
A full clinical evaluation is needed to find aortic thrombus. This includes looking at medical history, doing a physical check, and checking for risk factors.
Treatment for aortic thrombus is a mix of medical care, interventional procedures, and surgery. We choose the best treatment for each patient. This depends on the thrombus’s location, size, and the patient’s health.
Medical management is often the first step for aortic thrombus treatment. It aims to stop new clots from forming and lower the risk of problems.
Anticoagulation therapy uses medicines to stop new clots and prevent existing ones from getting bigger. Heparin and warfarin are common anticoagulants used.
Antiplatelet medicines, like aspirin and clopidogrel, stop platelets from sticking together. This helps prevent thrombus formation.
When medical management isn’t enough or the thrombus is risky, interventional procedures are needed.
Thrombolysis uses drugs to dissolve clots. It’s used in emergencies where the thrombus causes severe symptoms.
Endovascular procedures are minimally invasive to remove or bypass the thrombus. They’re good for patients at high risk for surgery.
Surgery is sometimes needed to remove the thrombus or fix the aorta.
Thrombectomy is surgery to remove the thrombus. It can be done through open surgery or endovascular methods.
Bypass surgery makes a detour around the blocked aorta segment. Grafts are used to restore blood flow.
| Treatment Approach | Description | Indications |
|---|---|---|
| Anticoagulation Therapy | Prevents new clot formation and enlargement of existing clots | Primary treatment for aortic thrombus |
| Thrombolysis | Dissolves the clot | Emergency situations with severe symptoms |
| Endovascular Procedures | Minimally invasive removal or bypass of thrombus | High-risk patients for surgery |
| Thrombectomy | Surgical removal of thrombus | Significant thrombus burden or failure of other treatments |
| Bypass Surgery | Creates a detour around the occluded aorta segment | Complex cases or when other treatments are not feasible |
Mural thrombus in abdominal aortic aneurysms (AAAs) is a complex issue. We will look at how AAA and mural thrombus are connected. We’ll also talk about the challenges in treating this condition and the options available.
Mural thrombus often occurs in abdominal aortic aneurysms. The presence of thrombus can make the aneurysm grow faster and increase the risk of rupture. The interaction between the thrombus and the aneurysm wall can lead to inflammation and weakening of the wall, potentially increasing the risk of rupture.
Managing AAA with mural thrombus is tough. The presence of thrombus can complicate surgical or endovascular interventions, as it may embolize during the procedure or affect the durability of the repair. Also, the risk of rupture and the need for close monitoring must be balanced against the risks associated with intervention.
Treatment for AAA with mural thrombus needs a team effort. Endovascular aneurysm repair (EVAR) is often preferred because it’s less invasive. But, the choice between EVAR and open surgery depends on the patient’s health and the aneurysm and thrombus details.
Personalized treatment plans are key for patients with AAA and mural thrombus. We focus on using the latest evidence and guidelines for each patient.
To prevent aortic thrombus in high-risk groups, we need a mix of lifestyle changes and medical steps. People with certain risk factors are more likely to get an aortic clot. So, it’s key to have specific prevention plans.
Making lifestyle changes is important in stopping aortic thrombosis. Quitting smoking is a big step, as smoking increases the risk of thrombus in the aorta. Also, exercising regularly and eating well can help keep your blood vessels healthy.
For those at high risk, medical prevention might be needed to stop aortic clot formation. Doctors often suggest anticoagulant therapy for those at high risk of abdominal aorta thrombus. The right anticoagulant and how long to take it depend on your risk factors and health history.
It’s important to regularly check and screen for aortic thrombosis. People with a history of vascular disease or other risk factors should see their doctor often. They should follow their healthcare provider’s advice on check-ups and screenings.
By following these prevention steps, high-risk individuals can lower their chance of getting an aortic thrombus. This can help avoid serious complications.
Understanding aortic thrombus is key for good diagnosis and treatment. We’ve looked into the aorta thrombus and thrombus in aorta, showing what causes them.
Aortic thrombosis can lead to serious problems if not treated. This includes embolization and damage to organs. So, finding and helping those at high risk is very important.
By learning more about aortic thrombus, we can get better at diagnosing and treating it. This will help improve how patients do. We need to keep researching and teaching about this condition.
It’s important to keep up with new info on aortic thrombus diagnosis and treatment. This way, we can give the best care to those with this condition.
An aortic thrombus is a blood clot in the aorta, the biggest artery in the body. It can cause serious health problems if not treated right.
Aortic thrombus is mainly caused by atherosclerosis and plaque buildup. It can also be due to hypercoagulable states, vascular injury, and cancer-related factors.
Symptoms of aortic thrombus vary based on where the clot is. They can include common symptoms, emergency signs, or silent findings.
Doctors use CT angiography, MRI, and ultrasound to find aortic thrombus. They also check lab tests and do clinical evaluations.
Treatments include medicine to prevent clotting and procedures like thrombolysis. Surgery like thrombectomy and bypass may also be needed.
Mural thrombus can form in an abdominal aortic aneurysm (AAA). It poses challenges and needs specific treatments.
To prevent it, high-risk people should quit smoking and exercise. Medical prevention and regular checks are also key.
Untreated aortic thrombus can cause embolism and organ damage. It can also lead to aortic occlusion and long-term vascular issues.
Knowing about aortic thrombus is vital for good medical care and better patient results. It shows the need for ongoing research and education.
Mural thrombus is a clot on the aorta’s wall. It’s linked to conditions like abdominal aortic aneurysm.
Yes, aortic thrombus can happen in various spots, like the abdominal and thoracic aortas. Each has its own traits.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!