Last Updated on November 26, 2025 by Bilal Hasdemir
For those dealing with anal fistula surgery, knowing about modern treatments can offer comfort. Seton placement is a key method for managing fistulas well.
Liv Hospital leads in advanced care, following international standards and using a team approach. They focus on new ways to treat fistulas, making them a top choice in the field.
Recovery means learning about different treatments, from old methods to new ones like seton suture. These options are part of anal fistula treatment.

It’s important to know the causes and symptoms of anal fistulas for early treatment. These are abnormal connections between the anus and the skin around it. They usually come from an infection or inflammation.
Anal fistulas often start with a blocked anal gland. This can cause an abscess that turns into a fistula. Other reasons include trauma to the anal area, Crohn’s disease, and past surgeries.
Several factors can lead to an anal fistula, including:
Symptoms of an anal fistula can be painful and include discharge or pus, and swelling. It’s key to notice these signs early to get medical help and avoid more problems.
Some symptoms that need a doctor’s check-up are:
If you’re showing any of these signs, seeing a healthcare professional is vital. They can give you the right diagnosis and treatment plan.

It’s important for patients to know about the different treatment options for anal fistula surgery. This surgery is not the same for everyone. It depends on the patient’s condition and how complex the fistula is.
Before surgery, patients go through several tests to figure out the best treatment. These tests help doctors understand the fistula’s complexity. They may include:
Surgery is needed when other treatments don’t work or if the fistula is severe. Doctors decide on surgery after checking the patient’s health and the fistula’s details.
The main goals of anal fistula surgery are to get rid of the fistula, stop it from coming back, and keep the anus working right. It’s all about removing the fistula without harming the anus.
| Treatment Goal | Description | Importance |
| Eliminating the Fistula | Removing the fistula tract to prevent further infection | High |
| Preventing Recurrence | Ensuring that the fistula does not return | High |
| Preserving Anal Function | Maintaining the normal functioning of the anal sphincter | Critical |
Knowing about these goals and tests helps patients understand anal fistula surgery better. It helps them make better choices for their care.
Traditional surgical methods are key in treating anal fistulas. They have improved over time. Now, they aim to fix the problem while keeping the sphincter working well.
Fistulotomy is a common method that opens the fistula tract surgically. It works well for simple fistulas and has a good success rate. But, it’s important to avoid harming the anal sphincter.
The surgery involves cutting along the fistula to let it drain and heal. It’s important to treat the problem well without risking incontinence. Doctors often choose this for fistulas close to the sphincter, where the risk is lower.
The LIFT procedure is a traditional method that focuses on saving the sphincter. It ties off the fistula tract at a specific point, closing it without harming the sphincter muscles.
This method is great for complex fistulas where keeping the sphincter intact is critical. The LIFT procedure has shown good results in healing and reducing complications.
One big challenge in treating anal fistulas is finding a balance. Surgeons need to fix the problem without harming the sphincter. Techniques like fistulotomy and LIFT aim to solve this problem.
Understanding the strengths and weaknesses of these traditional methods helps surgeons make better choices. This leads to the best results for patients.
Sphincter-sparing methods bring new hope to those with complex anal fistulas. These modern methods aim to keep the anal sphincter working while treating the fistula.
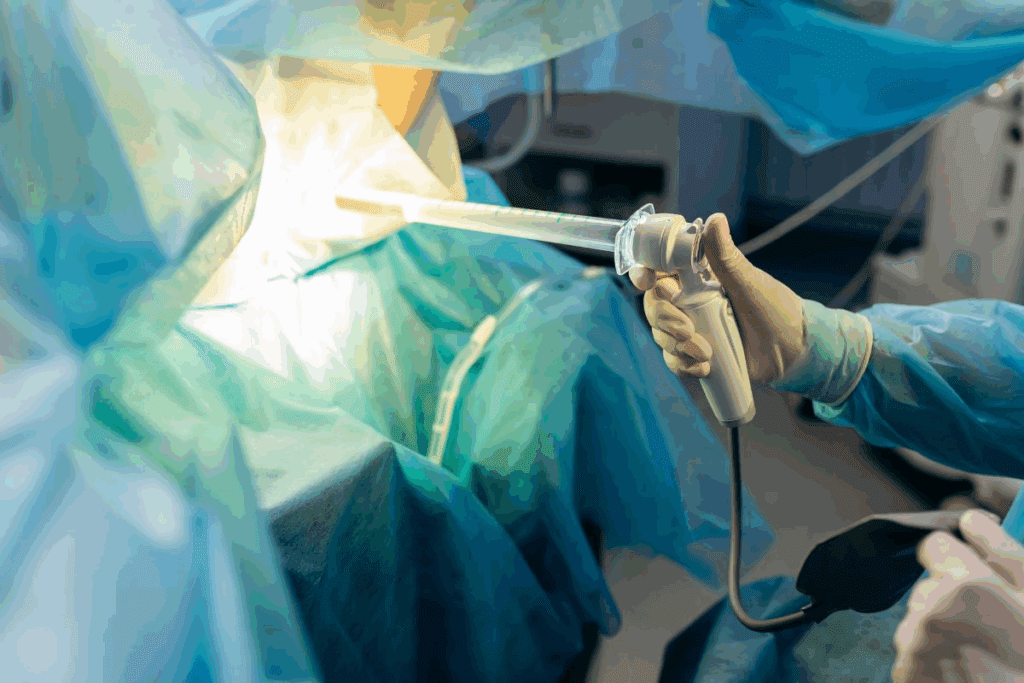
The FiLaC technique uses laser energy to close the fistula tract. It’s a minimally invasive method that heals by destroying the fistula’s lining. The procedure is done with direct vision, ensuring it’s accurate and safe for the surrounding tissues.
Benefits of FiLaC include:
Advancement flap procedures use healthy tissue to cover the fistula’s internal opening. This method is great for complex or high fistulas where other methods might not work.
The process involves:
Modern sphincter-sparing techniques greatly lower the risk of complications from traditional fistula surgery. These include incontinence and recurrence. By keeping the anal sphincter intact, these methods improve patient outcomes and quality of life.
Key advantages include:
By using these advanced techniques, surgeons can treat complex anal fistulas effectively. This minimizes complications and promotes long-term healing.
Seton placement is key in managing anal fistulas. It involves putting a band or suture into the fistula to help it drain and heal. This method is great for complex fistulas because it avoids damaging the anal sphincter.
A seton drain is a material in the fistula to keep it draining. It lets the healing start from the inside. This way, the fistula can close slowly, reducing the chance of abscesses.
Having a seton drain lowers the bacteria in the fistula. This makes healing easier. It’s a treatment that can be used alone or before surgery.
There are different seton materials like bands, tubes, and sutures. Each has its own benefits. Silk or rubber bands are popular for their durability. Silastic or latex tubes are used for their flexibility.
Setons keep the fistula open, letting it drain. This is key to stop pus buildup and abscesses. Over time, the seton helps the fistula close slowly.
This slow healing reduces the risk of problems like fecal incontinence. Seton placement leads to a more stable and lasting result.
Seton suture procedures are used for many types of anal fistulas. They are a safe and effective way to treat complex cases. This method is key for managing various types of fistulas.
Complex and high anal fistulas are hard to treat because of their location and complexity. Seton suture procedures are very helpful in these cases. They help the fistula heal slowly and reduce the chance of complications.
Seton sutures are great for:
Chronic anal fistulas need treatment in stages, with several procedures to heal fully. Seton suture procedures are essential in managing these cases.
| Stage | Treatment | Objective |
| 1 | Seton placement | Drainage and initial healing |
| 2 | Fistula tract assessment | Evaluate healing progress |
| 3 | Further treatment | Complete closure of the fistula tract |
Patients with inflammatory bowel disease (IBD) need special care with seton suture procedures. IBD can make treatment harder because of ongoing inflammation and the chance of more fistulas.
Careful management of IBD is key when using seton suture procedures. This includes:
Knowing how seton surgery works is key for those thinking about it for anal fistulas. It covers everything from getting ready before surgery to caring for yourself after.
Before seton surgery, patients go through a detailed prep. This includes checking their health and the fistula’s details.
Getting ready before surgery is key to avoiding problems and making the surgery work.
The steps for placing a seton are precise:
The type of seton and how it’s placed can change based on the surgeon and patient needs.
Good care after surgery is important for healing and avoiding problems.
| Aspect of Care | Description |
| Wound Care | Keeping the surgery area clean and watching for infection signs. |
| Pain Management | Using the right meds for pain after surgery. |
| Follow-Up | Seeing the doctor to check healing and adjust the seton if needed. |
Good care after surgery can really help the seton surgery work and make recovery better.
Medical practices have evolved, leading to better recovery rates for anal fistula surgery patients. New techniques have been added to improve patient results. This makes the recovery smoother and more effective.
Studies show that healing rates differ with each surgical method for anal fistulas. Fistulotomy, a traditional method, has healing rates between 57% to 87%. Newer methods like FiLaC and LIFT have shown even better results, with healing rates from 60% to over 90% in some cases.
| Surgical Technique | Healing Rate Range |
| Fistulotomy | 57% – 87% |
| FiLaC | 60% – 90% |
| LIFT | 70% – 95% |
The recovery timeline for anal fistula surgery can vary. It depends on the fistula’s complexity, the patient’s health, and the surgery type. Patients with health issues or complex fistulas may need more time to recover.
A healed fistulotomy scar has no pain, discharge, or swelling. The scar should be flat and not tender. Regular check-ups with a healthcare provider are key to monitor healing and handle any issues quickly.
In conclusion, knowing the recovery and success rates of modern treatments for anal fistulas is vital. By looking at healing rates and recovery factors, patients can make better choices. This helps them achieve the best possible results.
New technologies in seton devices have made anal fistula treatments better. These advancements have greatly improved patient care. They have reduced complications and helped wounds heal faster.
Seton devices have changed a lot over time. They used to be made from simple materials like rubber or silk. Now, they use silicone and synthetic fibers.
Modern seton materials are stronger and less likely to cause infections. The design of setons has also improved. Now, there are knotless setons and customized tubes for different needs.
New seton tubes and bands have made treating anal fistulas better. Seton tubes help with drainage and cause less damage. They come in different sizes and materials for better care.
Seton bands offer a more comfortable and effective option. They are designed to be less irritating and help wounds heal better.
New technologies in seton devices have greatly improved patient care. They reduce complications and help wounds heal faster. This has made treatment better for patients.
Using advanced materials and designs has also reduced discomfort after surgery. It has also improved long-term results. As technology keeps improving, seton devices will likely get even better.
It’s key for patients to know the treatment options for anal fistulas. This knowledge helps them make informed decisions about their care. Understanding anal fistula surgery and seton placement is vital for choosing the right fistula treatment.
Patients should look at both old and new ways of treating anal fistulas. Seton placement is a modern method that helps manage complex fistulas. It promotes drainage and healing over time.
To make informed decisions about fistula treatment, patients need to know all the treatment options. They should talk to their healthcare providers. This way, they can find the best treatment for their condition.
A seton drain is a medical tool used to treat anal fistulas. It helps by keeping the fistula open for drainage. This method aids in healing and prevents abscesses.
Seton suture procedures are used for complex and high anal fistulas. They are also for chronic fistulas and those with inflammatory bowel disease. This method is more detailed to manage the fistula and avoid complications.
The seton placement involves preparation and evaluation before surgery. The surgeon then places the seton through the fistula tract. Proper care after surgery is key for success.
Using a seton helps by promoting drainage and reducing abscess risk. It also allows for slow healing. This is very helpful for complex or chronic cases.
Seton materials can be bands, tubes, or sutures. The choice depends on the case and the surgeon’s preference.
Modern approaches like FiLaC and advancement flap are less invasive than traditional methods. They aim to reduce complications and promote healing.
Modern treatments show promising results. Healing rates vary based on the fistula’s complexity, the surgery, and post-care.
A healed fistulotomy scar is closed with little inflammation or discharge. The scar’s appearance varies by individual and surgery.
Seton materials and design have seen big improvements. New technologies aim to enhance drainage and healing for better patient outcomes.
Seton placement is key for complex anal fistulas. It promotes drainage, reduces complications, and aids in gradual healing. This is very beneficial for high or chronic fistulas.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!