When the aortic valve gets calcified, it can cause serious heart problems. Getting a diagnosis and treatment quickly is very important. At Liv Hospital, we focus on building trust and providing top-notch care.
Calcification of the aortic valve means calcium builds up on the valve. This makes the valve thick and stiff. It stops the valve from working right, which can lead to aortic stenosis.
It’s key to know about the causes, signs, and ways to treat a calcified aortic valve. We’ll look at the newest research and treatments. This will give you a full picture of what’s available.
Key Takeaways
- Calcification of the aortic valve can lead to serious heart complications.
- Timely diagnosis and treatment are key to managing the condition.
- Calcium buildup on the valve makes it thick and stiff.
- Aortic stenosis is a possible problem with calcified aortic valves.
- Knowing the causes, signs, and treatments is vital for managing the condition.
Understanding the Aortic Valve and Its Function

It’s key to know how the aortic valve works to understand its role in heart health. This valve is vital for blood to flow from the heart to the body. It makes sure blood moves in one direction.
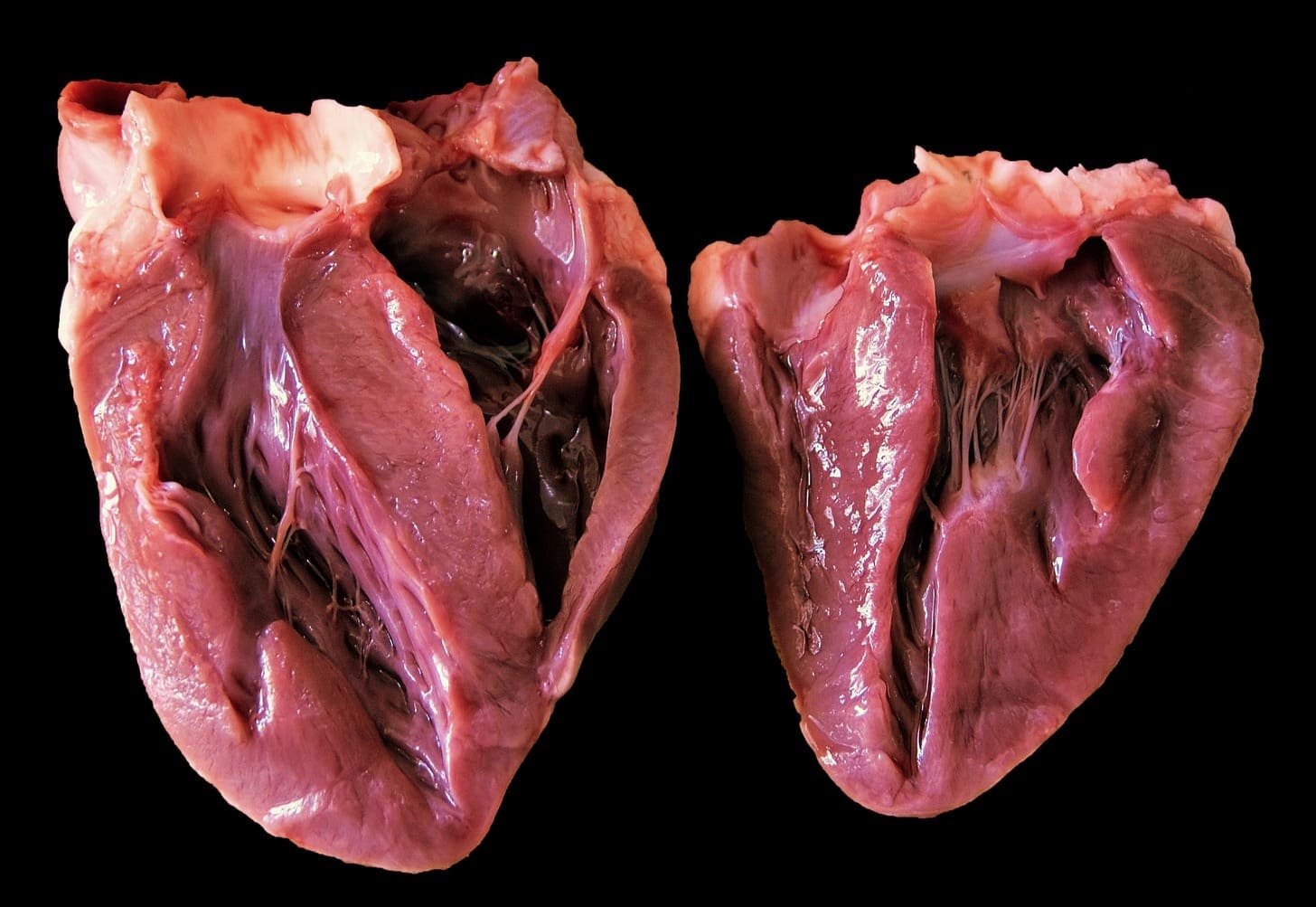
Normal Anatomy of the Aortic Valve
The aortic valve has three cusps that open to let blood flow into the aorta. The aorta is the biggest artery. Then, these cusps close to stop blood from flowing back. This process is essential for good blood flow.
Aortic valve calcification happens when calcium builds up on these cusps. This can cause problems.
Role in Blood Circulation
The aortic valve is key to the heart’s function. It makes sure blood flows only one way. This helps the heart pump blood well to the body’s parts.
For more on aortic stenosis, knowing how the valve works is important.
Aortic valve calcification can cause aortic stenosis. This is when the valve gets narrow, blocking blood flow. Knowing how the valve should work helps us understand the effects of calcification.
What Is Cardiac Valve Calcification?
Cardiac valve calcification is when calcium builds up on the heart valves. This makes the valves stiff and less able to work right.
Definition and Process
Calcification on the heart valves means calcium is deposited on them. It often happens on the aortic valve. Calcium builds up, making the valves thick and less mobile.
Types of Valve Calcification
There are several types of valve calcification, including:
- Calcific aortic valve disease
- Mitral annular calcification
Each type has its own features and health effects.
Difference Between Calcified Valve and Calcified Aorta
A calcified valve means calcium on the heart valve. A calcified aorta means calcium on the aortic wall. Both involve calcium, but they affect different parts and have different health impacts. Knowing the difference is key for correct diagnosis and treatment.
Prevalence and Epidemiology
As people get older, the chance of aortic valve calcification goes up a lot. This is a big worry for the elderly. We’ll look at how common it is, who’s at risk, and how it varies worldwide.
Age-Related Statistics
Aortic valvular calcification gets more common with age. About 2-4 percent of people over 65 get a serious case. This number goes up as more people get older, showing we need to keep an eye on it.
Risk Demographics
Some groups face a higher risk of severe aortic calcification. These include older adults, men, and those with heart disease history. Knowing who’s at risk helps us catch it early and treat it.
Global Prevalence Rates
The world’s aortic valve calcification rates differ. They’re affected by age, genes, and lifestyle. Here’s a look at rates in various places:
| Region | Prevalence Rate | Age Group |
|---|---|---|
| North America | 3.5% | 65+ |
| Europe | 4.2% | 65+ |
| Asia | 2.8% | 65+ |
Knowing about cardiac valve calcification helps us find who’s at risk. We keep studying it to help everyone’s health.
Causes and Risk Factors for Aortic Valve Calcification
It’s important to know what causes aortic valve calcification. This condition is influenced by many risk factors. Understanding these can help in early detection and management.
Age-Related Factors
Getting older increases the risk of aortic valve calcification. As we age, our aortic valve can degenerate and calcify. Studies show that more older people have this condition.
Medical Conditions
Some medical conditions raise the risk of a calcified aorta valve. High blood pressure, high cholesterol, and diabetes can increase this risk. People with kidney disease or on dialysis are also at higher risk.
Genetic Predisposition
Genetics also play a part in aortic valve calcification. If your family has a history of this condition, you’re more likely to get it. Research has found certain genetic variants that raise the risk.
Lifestyle Factors
Smoking and being inactive can also increase the risk. When the aorta is calcified, it affects the valve’s function. A healthy lifestyle, including a good diet and exercise, can help reduce these risks.
The Progression from Calcification to Aortic Stenosis
Aortic stenosis develops slowly from aortic valve calcification over years. It’s important to catch it early to treat it effectively.
Early Stages of Calcification
In the early stages, calcium builds up on the valve leaflets, making them thicker. This usually doesn’t cause symptoms, so it’s hard to spot without tests. As more calcium forms, the valve can’t open and close right.
Development of Stenosis
More calcium leads to aortic stenosis, where the valve opening gets smaller. This blocks blood flow, causing chest pain, shortness of breath, and tiredness.
Timeline of Progression
How fast calcification turns into stenosis varies. Age, health, and other conditions affect it. Regular check-ups with a doctor are key to managing it.
Watching calcification turn into stenosis is worrying and complex. Our team offers full care and support to those dealing with it.
Symptoms of a Calcified Aortic Valve
It’s important for patients and doctors to know the symptoms of a calcified aortic valve. This condition can cause various symptoms that affect how well a person lives. The symptoms can range from mild to severe.
Early Warning Signs
In the beginning, a calcified aortic valve might not show any symptoms. But as it gets worse, people might feel shortness of breath when they’re active. They might also feel fatigue. These signs mean the heart is working harder because the valve isn’t working right.
Advanced Symptoms
When the calcification gets worse, symptoms can get more serious. People might feel chest pain (angina), dizziness or fainting, and heart palpitations. In the worst cases, they might see signs of heart failure, like swelling in the legs and trouble breathing even when sitting or lying down.
When to Seek Medical Attention
If you or someone you know has symptoms like chest pain, severe shortness of breath, or fainting, get help right away. Catching it early and treating it can make a big difference for people with a calcified aortic valve.
Diagnosing Aortic Valve Calcification
Healthcare professionals use many tools to diagnose aortic valve calcification. They look at the patient’s symptoms and use advanced tests. This approach helps find the problem accurately.
Physical Examination
A physical exam is the first step. A doctor listens to the heart with a stethoscope. They look for heart sounds that might show valve problems.
A heart murmur can be a sign of aortic valve calcification.
Imaging Tests
Imaging tests are key to confirming the diagnosis. They show the heart and valves in detail. This helps doctors see how much calcification there is.
Echocardiogram
An echocardiogram uses sound waves to see the heart. It checks the aortic valve’s structure and function. Echocardiography is great for spotting calcification.
CT Scan
A CT scan gives detailed images of the heart. It helps measure how much calcification is there. It’s good for seeing how severe it is.
Cardiac MRI
Cardiac MRI shows the heart’s anatomy and function. It’s not the main tool for finding calcification. But it gives important info on how it affects the heart.
Laboratory Tests
Laboratory tests check for things that might cause valve calcification. High cholesterol or kidney disease are examples. These tests help understand the patient’s heart health.
Doctors use the results from exams, tests, and lab work to diagnose aortic valve calcification. Then, they create a treatment plan.
Understanding the Severity: Grading Aortic Valve Calcification
Doctors grade aortic valve calcification to see how it affects the heart. They look at how much calcium is there and how it changes the valve’s function. This helps them choose the best treatment.
Mild Calcification
In mild calcification, the valve has a small amount of calcium. It doesn’t really affect how the valve works. People with mild calcification might not feel any symptoms. It’s often found by accident during tests for other reasons.
Moderate Calcification
Moderate calcification means more calcium on the valve. This can make it harder for the valve to move. At this point, people might start feeling short of breath or have chest pain.
Severe Calcification
Severe calcification has a lot of calcium. It makes the valve work very poorly. This can cause aortic stenosis, where the valve gets too narrow. It blocks blood flow from the heart.
Impact on Heart Function
The effect on the heart depends on how severe the calcification is. As it gets worse, the heart works harder. If not treated, it can lead to heart failure. Knowing the severity helps doctors decide if treatment is needed.
- Mild calcification might not need treatment right away but needs watching.
- Moderate to severe calcification often needs treatment, either medicine or surgery.
Medical Management of Calcified Aortic Valve
Managing a calcified aortic valve needs a full plan. This includes medicine, lifestyle changes, and keeping an eye on how the disease is doing. The aim is to slow the disease, control symptoms, and boost the patient’s life quality.
Medication Options
There’s no medicine to reverse aortic valve calcification. But, some drugs can help with related issues like high blood pressure and high cholesterol. Statins and beta-blockers might be given to manage these problems.
Lifestyle Modifications
Changing your lifestyle is key in managing a calcified aortic valve. Patients should eat well, stay active, stop smoking, and drink less alcohol. These steps can help manage symptoms and slow the disease.
Monitoring and Follow-up Care
Keeping an eye on the disease is vital for patients with a calcified aortic valve. They need regular echocardiograms and visits with a cardiologist. This helps track the disease and adjust treatment plans if needed.
- Regular echocardiograms to monitor valve function
- Follow-up appointments with a cardiologist
- Adjustments to medication and lifestyle recommendations based on disease progression
Surgical Treatments for Aortic Valve Calcification
When aortic valve calcification gets severe, surgery is often the best choice. We know surgery can seem scary, but it can greatly improve life and survival for many.
Traditional Valve Replacement Surgery
Traditional valve replacement surgery is open-heart surgery. It replaces the calcified valve with a new one. This method has been the top choice for treating severe aortic valve calcification, with great success rates. It takes longer to recover than newer methods, but results are usually excellent.
Minimally Invasive Procedures
Minimally invasive surgeries are newer options. They use smaller cuts and might heal faster. Patients with severe aortic calcification might find these options appealing, but it depends on their health.
Transcatheter Aortic Valve Replacement (TAVR)
TAVR is a less invasive method. It uses a catheter to insert a new valve, usually through the femoral artery. TAVR is great for those at high risk or who can’t have traditional surgery. It offers quicker recovery and less risk, making it a popular choice.
Recovery and Rehabilitation
Recovering from aortic valve surgery, including TAVR, needs a good rehab plan. We focus on post-op care and cardiac rehab. These programs help patients get strong and improve heart health, leading to the best results.
Understanding surgical options for aortic valve calcification helps patients make better choices. We aim to provide top care and support every step of the way.
Recent Research and Emerging Treatments
New research is leading to better treatments for cardiac valve calcification. This condition is complex, but scientists are finding new ways to help. These discoveries bring hope for better health outcomes for patients.
Biological Mechanisms of Calcification
Studies have made big strides in understanding cardiac valve calcification. It’s not just a simple process. It involves many molecular pathways. Knowing this helps scientists create targeted treatments.
Experimental Therapies
New treatments are being tested to fight cardiac valve calcification. These include medicines and new surgical methods. Promising results from early trials show these treatments could be game-changers.
Future Directions in Treatment
As research deepens, we expect treatments to get more precise and effective. The future might bring precision medicine tailored to each patient. This could change how we manage this condition.
By keeping up with these advances, we can offer the best care to those with cardiac valve calcification.
Conclusion: Living with a Calcified Aortic Valve
Living with a calcified aortic valve means you need to be careful and keep an eye on your health. We’ve talked about how the condition affects your heart and the treatment options available. Knowing how severe the calcification is helps decide the best treatment.
A calcified heart valve can cause serious health problems if not treated. If the aorta is calcified, it affects the valve, possibly leading to aortic stenosis. To manage this, following medical advice and making lifestyle changes can help slow the disease.
People with a calcified aortic valve should stay in close touch with their doctor. They might need to change their treatment plan. This could include taking medicine, making lifestyle changes, or even surgery like TAVR.
Understanding your condition and its effects is key to managing your health. Regular check-ups and following treatment plans are vital. This helps improve your quality of life and outcomes if you have a calcified aortic valve.
What does it mean when the aortic valve is calcified?
When the aortic valve is calcified, calcium builds up on it. This makes the valve stiff and can stop it from working right.
What are the causes of aortic valve calcification?
Many things can cause aortic valve calcification. These include getting older, certain health conditions, genes, and lifestyle choices.
What are the symptoms of a calcified aortic valve?
Symptoms can start with shortness of breath and feeling tired. They can also include chest pain and heart palpitations.
How is aortic valve calcification diagnosed?
Doctors use several tests to find out if you have a calcified aortic valve. These include echocardiograms, CT scans, and cardiac MRIs.
What is the difference between a calcified valve and a calcified aorta?
A calcified valve means calcium on the heart valve. A calcified aorta means calcium on the aorta wall. They are different and affect the body in different ways.
How is the severity of aortic valve calcification graded?
Doctors grade the severity from mild to severe. They look at how much calcium is there and how it affects the heart.
What are the treatment options for a calcified aortic valve?
Doctors can treat it with medicine and lifestyle changes. They can also do surgery, like traditional replacement or TAVR.
What is the progression from calcification to aortic stenosis?
Calcification can narrow the valve opening. This blocks blood flow and can cause serious problems.
Can lifestyle modifications help manage a calcified aortic valve?
Yes, eating right, exercising, and managing stress can help. They can slow the disease’s progress.
What is the role of monitoring and follow-up care in managing a calcified aortic valve?
Regular check-ups are key. They help catch problems early and adjust treatment plans as needed.
What are the emerging treatments for cardiac valve calcification?
New treatments are being tested. They aim to stop calcification by targeting its causes. This could be a future treatment option.
What is cardiac valve calcification?
It’s when calcium builds up on heart valves. This makes them stiff and can affect how they work.
What is aortic valvular calcification?
It’s when the aortic valve gets calcified. This is a specific type of cardiac valve calcification.
What does severe aortic calcification mean?
It means the aortic valve or aorta has a lot of calcium. This can lead to serious health problems and complications.
References
- Vinmec International Hospital (Heart Valve Calcification) : https://www.vinmec.com/eng/blog/heart-valve-calcification-symptoms-and-treatment-en
- PMC – PubMed Central : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4888946
- AHA Journals (Circulation) : https://www.ahajournals.org/doi/10.1161/circulationaha.104.486738
- Nature Cardiovascular Research : https://www.nature.com/articles/s41569-023-00845-7
- Gladstone Institutes (Potential Therapy for One of the Leading Causes of Heart Disease) : https://gladstone.org/news/potential-therapy-one-leading-causes-heart-disease


































