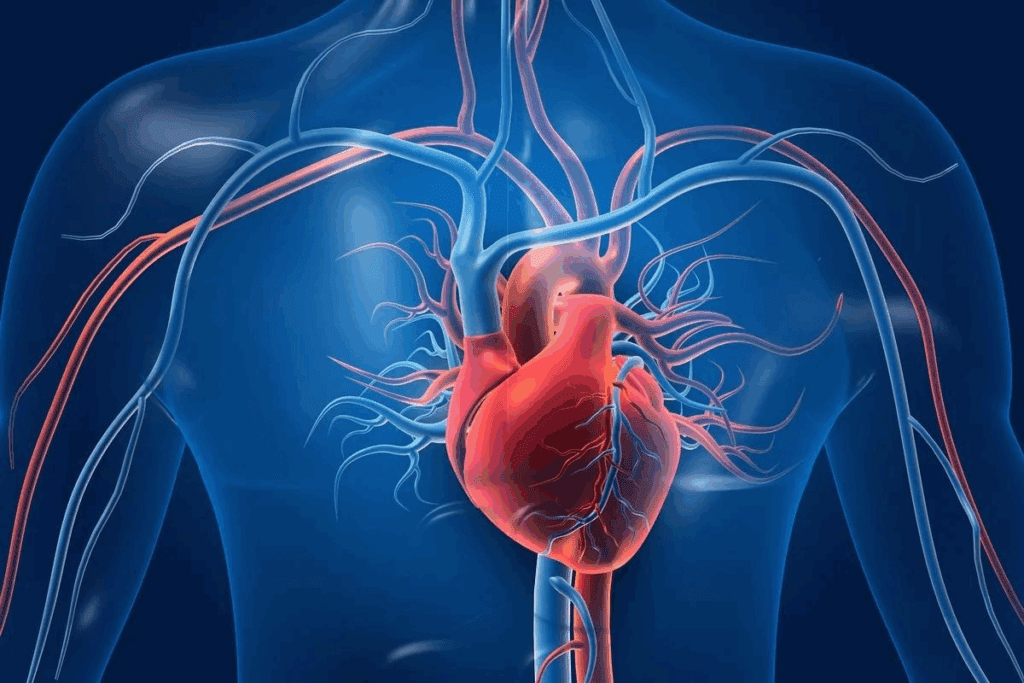
At Liv Hospital, we know the question about heart stents is complex. The choice to use cardiac stents depends on many things. This includes the person’s body shape and how bad their heart disease is.
We see that every patient is different, and the number of stents needed depends on each person’s heart condition and overall health. Our team works closely with every patient to find the safest and most effective treatment plan. Many people ask about the maximum number of stents in heart, and while there isn’t a fixed limit, doctors carefully evaluate risks and benefits before placing additional stents to ensure the best possible outcomes.
Key Takeaways
- The number of stents that can be placed depends on individual anatomy and coronary disease severity.
- Cardiac stents are used to restore blood flow through blocked arteries.
- The decision to place stents is made on a case-by-case basis.
- Liv Hospital’s team of experts works closely with patients to determine the best treatment plan.
- Patient-centered care is our top priority at Liv Hospital.
Understanding Cardiac Stents and Their Purpose

Cardiac stents are tiny, expandable tubes used to treat coronary artery disease. This disease can lead to heart attacks if not treated. These devices are key to keeping arteries open, ensuring blood flows freely to the heart.
What Are Cardiac Stents?
Cardiac stents, also known as coronary stents, are small, mesh-like tubes made from metal or other materials. They are placed in narrowed or blocked arteries to restore blood flow. This helps alleviate symptoms of coronary artery disease, like chest pain, and lowers the risk of heart attacks.
How Stents Work to Improve Blood Flow
Placing a cardiac stent involves a minimally invasive procedure called angioplasty. A thin, flexible tube called a catheter is guided to the blocked artery. The stent is then expanded to push aside the blockage, widening the artery. This improves blood flow to the heart muscle, reducing heart damage.
Stents not only improve blood flow but also stabilize the plaque. This reduces the chance of it rupturing and causing a blockage. This is critical for patients with acute coronary syndrome, where heart attack is high.
Types of Cardiac Stents Available Today
There are several types of cardiac stents, each designed for different patient needs. The main categories include:
- Bare Metal Stents (BMS): These are the original stents, made from metal mesh. They are less used now due to a higher risk of restenosis (re-narrowing of the artery).
- Drug-Eluting Stents (DES): These stents are coated with medication to prevent artery re-narrowing. They are the preferred choice for many due to their effectiveness in reducing restenosis.
- Bioresorbable Stents: A newer type of stent that gradually dissolves over time. They may reduce long-term complications associated with traditional metal stents.
Each stent type has its benefits. The choice depends on the patient’s condition, including the severity of their coronary artery disease and overall health.
The Maximum Number of Stents in the Heart: Is There a Limit?

Cardiac stents are a common treatment for coronary artery disease. But, is there a limit to how many can be implanted? The decision to place multiple stents depends on the patient’s health and the severity of their condition.
Medical Perspective on Stent Quantity
From a medical standpoint, there’s no strict limit on the number of stents. The decision is made based on each patient’s unique situation. This includes their coronary anatomy, the location and severity of blockages, and their heart function.
Key Considerations for Multiple Stent Placement:
- The extent of coronary artery disease
- The presence of complex lesions
- The patient’s response to previous stent placements
- Overall cardiovascular health
Case Reports of Multiple Stent Placements
There have been cases where patients got multiple stents successfully. These cases show how modern cardiac care is flexible and adaptable.
| Number of Stents | Patient Profile | Outcome |
| 2-3 Stents | Patients with multiple blockages | Improved blood flow, symptom reduction |
| 4 or more Stents | Complex cases with extensive disease | Managed symptoms, improved quality of life |
Why There’s No Fixed Upper Limit
The lack of a strict upper limit on stent placement is due to the unique nature of cardiac disease. Each patient’s condition is different, needing a personalized treatment approach.
We look at many factors when deciding on multiple stent placements. This ensures each patient gets the best care for their specific needs.
Factors That Determine How Many Stents Can Be Placed
Many factors decide how many stents can go into the heart. Putting stents in is a big decision. It needs a full check of the patient’s health.
Individual Coronary Anatomy
Every person’s heart arteries are different. This difference affects how many stents are needed. We look at artery size, any odd shapes, and how the arteries connect.
Key aspects of coronary anatomy that affect stent placement include:
- The diameter and length of the coronary arteries
- The presence of any coronary artery anomalies
- The extent of calcification or plaque buildup
Severity and Location of Blockages
The blockages in the arteries are very important. We check how tight they are and where they are. This helps decide how many stents are needed.
| Blockage Severity | Typical Treatment Approach |
| Mild Stenosis (<50%) | Monitoring or medical therapy |
| Moderate Stenosis (50-70%) | Stent placement or angioplasty |
| Severe Stenosis (>70%) | Stent placement, potentially with multiple stents |
A top cardiologist says, “The blockage’s location and how bad it is decide the treatment. This includes how many stents are needed.”
Overall Heart Function and Health
The heart’s function and the patient’s health are key. We check the heart’s pumping ability, any other heart issues, and overall health. This helps decide on the right number of stents.
By looking at these factors, we choose the best number of stents for each patient. This ensures the best results for them.
Common Scenarios: 2 Heart Stents and 3 Stents in Heart
Patients with multiple blockages in their coronary arteries might need 2 or 3 stents. This is common in treating coronary artery disease. The goal is to make sure the heart gets the oxygen and nutrients it needs.
When 2 Heart Stents Are Typically Needed
Doctors might suggest 2 heart stents in certain situations. These include:
- Multiple blockages in different branches of the coronary arteries
- A blockage in a large coronary artery that requires stenting to maintain blood flow
- Restenosis (re-narrowing) of a previously stented artery
In these cases, 2 stents can improve blood flow to the heart. This reduces symptoms like chest pain and shortness of breath.
Patients Living with 3 Stents in the Heart
Many patients with coronary artery disease have 3 stents in their hearts. While it’s a concern, many lead active and fulfilling lives. The key is to work closely with your healthcare team and make lifestyle adjustments as needed.
Important considerations for patients with 3 stents include:
- Adhering to a healthy diet and exercise plan
- Taking medications as prescribed to prevent clotting and manage other conditions
- Attending regular follow-up appointments with your cardiologist
Managing Daily Life with Multiple Stents
Living with multiple stents requires some adjustments. But with the right mindset and support, patients can lead normal, active lives. It’s essential to understand your condition, follow your treatment plan, and make healthy lifestyle choices.
Some tips for managing daily life with multiple stents include:
- Staying informed about your condition and treatment options
- Maintaining a healthy weight through diet and exercise
- Managing stress through relaxation techniques such as meditation or deep breathing
By taking these steps, patients with 2 or 3 stents in their hearts can enjoy improved health and well-being. This reduces the risk of complications and improves their quality of life.
Complex Cases: 4 Stents in Heart and Beyond
Advanced coronary artery disease can lead to the need for multiple stents. This presents unique challenges. In such cases, patients might need 4 or more stents to treat multiple blockages effectively.
Medical Indications for 4 Heart Stents
The decision to use 4 or more stents is made when a patient has extensive coronary artery disease. This disease involves multiple blockages. It can affect several arteries or long segments of one artery.
Medical reasons for using multiple stents include:
- Multiple blockages in different coronary arteries
- Long lesions that cannot be treated with a single stent
- Restenosis (re-narrowing) of previously stented areas
- Complex bifurcation lesions involving major side branches
Patients Living with 5 Stents
Some patients live with 5 stents due to severe coronary artery disease. While it poses challenges, many lead active lives with proper management.
| Aspect | Considerations for Patients with 5 Stents |
| Medication Management | Dual antiplatelet therapy (DAPT) for an extended period, potentially lifelong aspirin use |
| Lifestyle Adjustments | Dietary changes, regular exercise, and smoking cessation |
| Follow-up Care | Regular check-ups with cardiologists, periodic stress tests |
Managing Risks with Higher Stent Numbers
As the number of stents increases, so does the risk of complications. Managing these risks is key for patients with 4 or more stents.
Key strategies include:
- Strict adherence to prescribed medications
- Regular follow-up appointments with healthcare providers
- Lifestyle modifications to reduce cardiovascular risk factors
- Monitoring for signs of stent failure or new blockages
By carefully managing their condition, many patients with multiple stents can lead fulfilling lives.
Exceptional Situations: Can You Have 6 Stents in Your Heart?
Doctors have seen patients with six or more stents in their hearts. These cases are rare but show the need for tailored heart care. They involve complex heart disease.
Documented Cases of Patients with 6+ Stents
There are cases where patients have had more than six stents. These patients often have severe heart disease. They haven’t gotten better with other treatments.
- Patients with multiple blockages in various coronary arteries
- Individuals with a history of previous stent placements or coronary artery bypass grafting
- Cases where stenting is preferred over more invasive surgical procedures
Special Considerations for Extensive Stenting
Requiring six or more stents brings special concerns. These include:
- Increased risk of complications: More stents can lead to higher risks of bleeding or stent thrombosis.
- Enhanced monitoring requirements: Patients with many stents need more check-ups and tests.
- Complex antiplatelet therapy management: Managing blood thinners gets harder with more stents.
Long-term Outcomes and Monitoring
Long-term results for patients with six or more stents vary. They depend on heart health, lifestyle, and medication.
Key factors influencing long-term outcomes include:
- Lifestyle changes, like diet and exercise
- Following prescribed medications, including blood thinners
- Regular visits to a cardiologist
With proper management, patients with many stents can live well. Even with six or more stents, they can have active and meaningful lives.
How Many Stents Can Be Placed in One Artery
Deciding to put more than one stent in an artery is a tough call. It depends on many technical and medical factors. Cardiologists must think about the benefits and risks for each patient and the artery’s specific needs.
Technical Considerations for Multiple Stents in One Vessel
Putting multiple stents in one artery needs careful planning and skill. Factors like stent size, blockage severity, and artery shape matter a lot. The goal is to place the stents correctly, covering the diseased area well and avoiding problems.
Choosing the right stent size and position is a big challenge. Wrong sizing can cause stent failure or blockage, while bad placement might not fully cover the area. Tools like intravascular ultrasound (IVUS) or optical coherence tomography (OCT) help place stents accurately.
Overlapping Stents: Benefits and Risks
Often, stents need to overlap to cover the diseased area fully. Overlapping stents can reduce the chance of blockage coming back. But there are risks like more metal in the artery, which might increase the chance of clotting.
- Increased risk of stent thrombosis
- Potential for increased inflammation
- Higher metal burden
To lower these risks, cardiologists plan stent placement carefully. They consider the stent type and the artery’s condition. Drug-eluting stents, which release medicine to prevent cell growth, can help prevent blockage.
Case Examples of 2 Stents in One Artery
There are cases where two stents were placed in one artery successfully. For example, when a long blockage is present, two stents are used to cover it fully. The procedure needs precise planning to avoid issues.
In summary, the choice to use multiple stents in one artery is complex. By carefully looking at technical and medical factors, cardiologists can get the best results for their patients.
How Many Heart Stents Can Be Put In During One Procedure
The number of stents in one heart procedure depends on several things. These include the patient’s health and the blockage’s complexity.
Cardiologists look at the patient’s health, blockage severity, and procedure feasibility. They decide how many stents can be used at once.
How Many Stents Can Be Placed at One Time
Often, more than one stent is used in a single procedure. This is common when blockages are close together in the heart’s arteries.
The number of stents varies by case. But, placing two or three stents in one go is not rare.
When Staged Procedures Are Recommended
In some cases, staged procedures are better. This means stents are placed in steps, with time to recover between each step.
Staged procedures are chosen for complex blockages or when caution is needed. This approach helps manage risk.
Recovery Differences Between Approaches
Recovery times differ between single-procedure and staged-procedure patients. Single-procedure patients might take longer to recover at first.
But staged procedure patients have shorter recovery times between steps. Their overall treatment time is longer, though.
To show the recovery and procedure differences, let’s look at a comparison table:
| Procedure Type | Recovery Time | Number of Stents | Patient Condition |
| Single Procedure | Longer initial recovery | Multiple stents | Stable, with complex blockages |
| Staged Procedures | Shorter between stages, longer overall | Multiple stents, placed in stages | Complex cases or high-risk patients |
Knowing these differences helps patients prepare for their treatment and recovery.
Long-term Considerations for Patients with Multiple Stents
The success of multiple stents depends on several factors. These include sticking to medication, regular check-ups, and making lifestyle changes. A detailed plan is needed to keep the stents working well and avoid problems.
Medication Requirements
Patients with multiple stents often take antiplatelet therapy to stop blood clots. It’s important to take the medication as directed. Common drugs include:
- Aspirin
- P2Y12 inhibitors (e.g., clopidogrel, prasugrel)
The length of time for taking these drugs varies. Always follow your cardiologist’s advice on how long to take them.
| Medication | Purpose | Typical Duration |
| Aspirin | Prevent platelet aggregation | Indefinite |
| P2Y12 inhibitors | Prevent clot formation | 6-12 months or longer |
Follow-up Care and Monitoring
Regular visits to the cardiologist are key. They help check the stents and heart health. These visits might include:
- Stress tests to check heart function
- Coronary angiography to see the stents
- Blood tests for clotting or other issues
Finding problems early helps fix them quickly. This lowers the chance of serious issues.
Lifestyle Modifications for Stent Longevity
Changing your lifestyle is important for stent health. Key changes include:
- Quitting smoking
- Eating a heart-healthy diet
- Staying active
- Managing stress
Living a healthy lifestyle helps the stents last longer and improves heart health.
Understanding and following these long-term tips helps patients with multiple stents live well. It’s a team effort between patients, doctors, and healthcare teams for the best results.
Conclusion: Individualized Approach to Cardiac Stenting
The number of stents in the heart varies greatly from person to person. Deciding on stents depends on many factors. These include the heart’s structure, blockage severity, and overall heart health.
There’s no single answer to how many stents are needed. Each person’s situation is unique. So, a tailored approach to stenting is key. This ensures each patient gets the right treatment for their needs.
Understanding cardiac stenting and its complexities helps patients make better choices. Personalized medical advice is vital for the best results. It guides individuals through their stenting procedures effectively.
FAQ
How many stents can be placed in the heart?
The number of stents in the heart varies. It depends on the person’s anatomy and the disease’s severity.
Is there a maximum limit to the number of stents that can be placed?
There’s no fixed limit on stents from a medical standpoint. The decision is based on the person’s condition and need.
What determines the number of stents that can be placed?
Several factors decide on stent placement. These include the heart’s anatomy, blockage severity, and overall health.
Can you have 2 or 3 stents in your heart?
Yes, sometimes 2 or 3 stents are needed. This is often the case with complex heart disease.
Can you have 4 or more stents in your heart?
Yes, in severe cases, 4 or more stents might be required. This is for extensive heart disease.
Can you have 6 stents in your heart?
Though rare, some patients have had 6 or more stents. Such cases need careful long-term management.
How many stents can be placed in one artery?
Placing multiple stents in one artery has technical aspects. These include the benefits and risks of overlapping stents.
How many stents can be placed during one procedure?
Deciding on multiple stents in one go depends on the patient’s condition. Sometimes, procedures are done in stages.
What are the long-term considerations for patients with multiple stents?
Patients with multiple stents need ongoing care. This includes medication, follow-ups, and lifestyle changes.
What are the risks associated with having multiple stents?
Risks include complications like stent thrombosis or restenosis. Close monitoring and management can reduce these risks.
How can patients manage their daily lives with multiple stents?
Patients can manage daily life with a healthy lifestyle. This includes a balanced diet, exercise, stress management, and following medication and care plans.
References
- Amirzadegan A., et al. (2019). Single Long Stents versus Overlapping Multiple Stents: Clinical Outcomes and Safety. Cardiovascular Revascularization Medicine, 20(9), 731-738. https://pmc.ncbi.nlm.nih.gov/articles/PMC6981347/