Last Updated on November 27, 2025 by Bilal Hasdemir
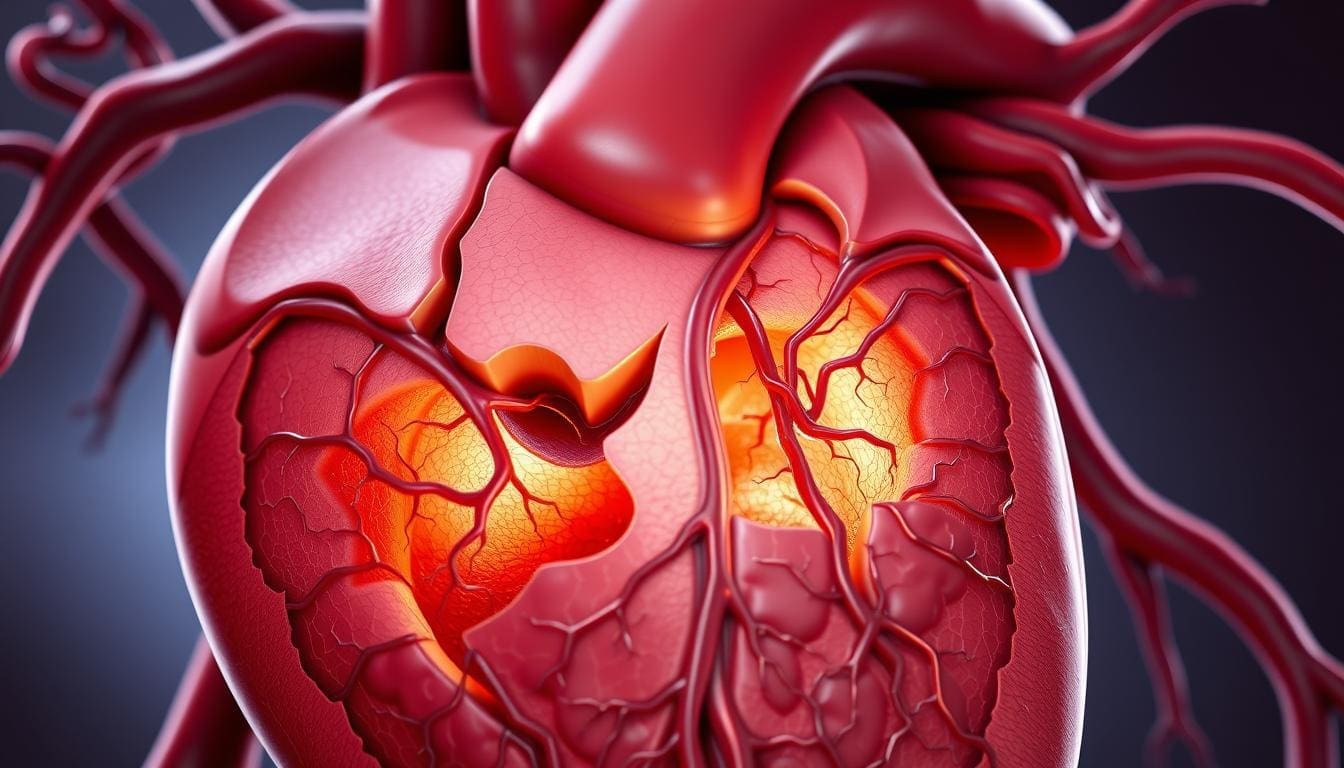
At Liv Hospital, we provide patient-centered care for those with cardiovascular ischemic disease. This condition, also known as ischemic heart disease (IHD), happens when the coronary arteries get narrowed or blocked. This reduces blood flow to the heart.
Ischemic heart disease is a big global health issue, affecting millions worldwide. We will look at the different types of ischemic heart disease, its effects on the heart, and important facts about it.
Knowing about ischemic heart disease is key for prevention, diagnosis, and treatment. We aim to offer trusted advice and support for those looking for top-notch medical care.
It’s important for both doctors and patients to understand ischemic heart disease. This condition happens when the heart doesn’t get enough blood and oxygen. It’s a big reason for sickness and death around the world.
Ischemic heart disease means the heart doesn’t get enough blood. This usually happens because of blocked coronary arteries. These arteries carry blood to the heart muscle.
The main cause is atherosclerosis. This is when plaque builds up in the arteries.
The steps to ischemic heart disease are:
When the heart doesn’t get enough blood and oxygen, it can cause problems. These can range from mild chest pain to a heart attack. The severity depends on how much and for how long the blood flow is reduced.
The effects of reduced blood flow include:
It’s key to know the symptoms and warning signs of ischemic heart disease. Common signs are chest pain or discomfort. This can spread to the arms, back, neck, jaw, or stomach. Other signs are shortness of breath, nausea, feeling lightheaded, or tired.
Being aware of these signs and getting medical help is important. Early treatment can greatly improve a patient’s chances of recovery.
It’s important for both patients and doctors to understand the terms related to heart disease. These terms and abbreviations can be confusing. We aim to make them clear for easier understanding.
IHD stands for Ischemic Heart Disease. I.H.D. is another way to write it, with periods. Both mean the heart doesn’t get enough blood because of blocked arteries. The list of medical abbreviations shows IHD is widely used in medicine.
The words ischemic and ischaemic mean the same thing. But, they are spelled differently based on where you are. In the UK, people use ischaemic, while in the US, it’s ischemic. Both describe when the heart doesn’t get enough blood.
Coronary Heart Disease (CHD) and Ischemic Heart Disease (IHD) are similar but not the same. CHD usually means the arteries are blocked by plaque. IHD is a broader term for any condition that reduces blood flow to the heart. Knowing the difference helps doctors diagnose and treat better.
Understanding ischemic heart disease is key to finding treatments. It involves many factors that reduce heart function.
Atherosclerosis plays a big role in ischemic heart disease. It causes plaque buildup in arteries, making them hard and narrow. This starts with lipids, macrophages, and smooth muscle cells in the artery walls.
These components form plaques, some stable, others unstable. Unstable plaques can rupture, causing sudden ischemic events.
Risk factors like high LDL cholesterol, high blood pressure, smoking, and diabetes affect plaque formation. They cause inflammation and oxidative stress, making plaques unstable.
Atherosclerotic plaques can narrow coronary arteries, reducing blood flow to the heart. This can cause chest pain due to temporary heart muscle ischemia. If a plaque ruptures, it can block the artery, leading to a heart attack.
The extent of artery narrowing determines the disease’s severity. Severe narrowing can cause chronic ischemia, while complete blockage can lead to a heart attack.
Reduced blood flow due to narrowed or blocked arteries leads to heart muscle oxygen deprivation. This is called ischemia. Prolonged ischemia can damage the heart muscle, leading to a heart attack.
The damage’s extent depends on how long and how severe the ischemia is. It also depends on the presence of collateral circulation. Understanding these processes is vital for treating the disease.
It’s important to know the different types of ischemic heart disease. This knowledge helps doctors diagnose and treat it better. Each type has its own signs and symptoms.
Stable angina is a condition where the heart doesn’t get enough oxygen. It causes predictable chest pain or discomfort. This pain usually happens when you’re active or stressed and goes away with rest or medicine.
Managing stable angina involves lifestyle changes and medicine. But, it’s key to watch it closely. It can lead to more serious heart diseases.
Unstable angina is a serious and unpredictable form of angina. It can signal a heart attack is coming. The pain is intense and can happen at rest or with little effort.
Seeing a doctor right away is critical for unstable angina. It means the heart isn’t getting enough oxygen, and a heart attack is likely.
A heart attack happens when the heart doesn’t get enough blood. This damages or kills heart muscle. It’s usually because of a blockage in the coronary arteries.
This blockage can be a blood clot on a plaque. When the plaque ruptures, it forms a thrombus that blocks the artery.
Silent ischemia is when the heart doesn’t get enough blood without pain. It’s dangerous because it often goes unnoticed until it’s too late.
It’s more common in people with diabetes. Doctors use tests like ECGs to find it.
| Type of Ischemic Heart Disease | Characteristics | Symptoms | Urgency |
|---|---|---|---|
| Stable Angina | Predictable chest pain during exertion | Chest pain or discomfort | Low to Moderate |
| Unstable Angina | Unpredictable, intense chest pain | Severe chest pain or discomfort at rest or with minimal exertion | High |
| Myocardial Infarction (Heart Attack) | Blockage of blood flow to the heart muscle | Severe chest pain, shortness of breath, nausea | Critical |
| Silent Ischemia | Reduced blood flow without symptoms | No typical symptoms | Variable, often undiagnosed until severe |
Knowing about these types of ischemic heart disease is key. Each needs a specific plan to manage risks and improve health.
Cardiology faces a big challenge with silent ischemia. This is when heart disease gets worse without symptoms. We’ll look at the risk factors, its link to diabetes, and how hard it is to find this condition.
Silent ischemia has many risk factors like high blood pressure, high cholesterol, smoking, and obesity. Some people are more likely to have it because they don’t feel pain as much. This is due to factors that hide the usual heart disease symptoms.
Diabetes is a big risk because it can damage nerves. This makes it harder to feel pain. Other risks include being older and having a history of heart disease.
Diabetes and silent ischemia are closely linked. High blood sugar in diabetes can damage nerves. This makes it hard for pain signals from the heart to reach the brain.
“The presence of diabetes mellitus is a significant predictor of silent ischemia, highlighting the need for vigilant monitoring in this high-risk population.”
– Journal of Cardiology
Finding silent ischemia is hard because it doesn’t show symptoms. But, there are ways to spot it. Regular heart disease checks are key, even more so for those with diabetes or other risks.
| Detection Method | Description | Benefit |
|---|---|---|
| Stress Test | A test that measures heart function under stress | Identifies ischemia during physical activity |
| Electrocardiogram (ECG) | A recording of the heart’s electrical activity | Detects abnormal heart rhythms and ischemia |
| Coronary Angiography | An imaging test that visualizes the coronary arteries | Identifies blockages in the coronary arteries |
Spotting silent ischemia early is key to managing it well. Knowing the risks and using the right tests helps doctors treat it before it gets worse.
We use many tools to find cardiovascular ischemic disease. This helps us make good treatment plans. We use both non-invasive and invasive tests to understand the disease well.
First, we use non-invasive tests to find the disease. These include:
Imaging tests are key in finding ischemic heart disease. They show the heart’s structure and function. Myocardial Perfusion Imaging (MPI) and Cardiac Magnetic Resonance (CMR) spot ischemic or infarcted areas.
These tests give us important info on ischemic defects. They help us decide on treatment.
When non-invasive tests don’t give clear results or when we need to act, we use invasive tests. The main one is:
Invasive tests give us detailed info on the coronary arteries. This helps us choose the best treatment for ischemic heart disease.
We use many treatments to help manage ischemic heart conditions. The right treatment depends on how severe the condition is and the patient’s health.
Medicines are key in treating ischemic heart disease. They help lessen symptoms, slow the disease’s growth, and prevent serious problems.
| Medication Class | Primary Use | Examples |
|---|---|---|
| Antiplatelet agents | Prevent blood clots | Aspirin, Clopidogrel |
| Beta-blockers | Reduce heart workload | Metoprolol, Atenolol |
| Nitrates | Improve blood flow | Nitroglycerin |
| Statins | Lower cholesterol | Atorvastatin, Simvastatin |
For some, interventional procedures are needed to get blood flowing to the heart again.
Angioplasty and stenting are often used to open blocked or narrowed arteries. A balloon is used to widen the artery, and a stent keeps it open.
Changing your lifestyle is also very important in managing ischemic heart disease. These changes can lessen symptoms, improve life quality, and help treatment work better.
By using these treatments together, we can manage ischemic heart disease well and improve patient results.
To prevent cardiovascular ischemic disease, we need a mix of lifestyle changes and medical care. We’ll look at how to lower the risk of ischemic heart disease. This includes managing risk factors, eating right, exercising, and getting regular check-ups.
It’s key to tackle risk factors that can be changed. These are high blood pressure, high cholesterol, diabetes, smoking, and being overweight. By controlling these, people can greatly lower their risk of heart disease.
Eating well and exercising regularly are key to avoiding heart disease. Eat lots of fruits, veggies, whole grains, and lean meats. Avoid foods high in saturated fats, trans fats, and cholesterol.
Do at least 150 minutes of moderate exercise weekly. Or, do 75 minutes of vigorous exercise. Adding strength training helps too.
Screenings are important for spotting heart disease risk early. People with heart disease in their family, risk factors, or who are older should get checked often. This helps keep their heart health in check.
New ways to prevent heart disease are being studied. This includes new meds, genetic tests, and lifestyle changes. Keeping up with these advances helps make smart choices for heart health.
Being proactive about heart health can greatly reduce heart disease risk. A good plan includes lifestyle changes, regular check-ups, and medical care when needed.
Living with ischemic heart disease means taking charge of your health. It’s about combining medical care, lifestyle changes, and ongoing support. This approach can greatly improve your outlook and help you live a full life.
Staying heart-healthy is key. Eat well, exercise often, and don’t smoke. Also, see your doctor regularly to keep an eye on your health and adjust your treatment if needed.
Managing ischemic heart disease is a big job, but it’s doable. With the right steps, you can enjoy a better life. We’re here to offer top-notch care and support for patients from around the world, guiding them through their journey with ischemic heart disease.
Ischemic heart disease, also known as coronary heart disease (CHD), happens when the heart muscle doesn’t get enough oxygen. This is because the coronary arteries are narrowed or blocked.
Symptoms include chest pain (angina), shortness of breath, and feeling tired. You might also feel pain in your arms, back, neck, jaw, or stomach. Some people have silent ischemia, where they don’t notice any symptoms.
Stable angina is predictable chest pain that happens when you exert yourself and goes away when you rest. Unstable angina is unpredictable and can happen at any time. It’s a sign you might be having a heart attack.
Doctors use tests like electrocardiogram (ECG), stress test, and echocardiogram to diagnose it. They also do coronary angiography and check cardiac biomarkers. These tests help find out if there’s a problem and how bad it is.
Treatment includes medicines, procedures like angioplasty and stenting, and surgery like CABG. Changing your diet, exercising, and managing stress are also important.
Yes, many cases can be prevented. By managing risk factors like high blood pressure, high cholesterol, and smoking, you can lower your risk. Making lifestyle changes and getting medical help are key.
Silent ischemia is when the heart doesn’t get enough blood without symptoms. It’s dangerous because it can lead to a heart attack without warning.
People with ischemic heart disease should follow their treatment plan and make lifestyle changes. They should also watch for symptoms and keep up with doctor’s appointments.
CHD and IHD are often used to describe the same condition. Both refer to narrowed or blocked coronary arteries, which reduces blood flow to the heart.
Yes, new strategies include medicines, advanced procedures, and lifestyle changes. These aim to reduce the risk of getting ischemic heart disease.
“Clinical updates in coronary artery disease: non-invasive diagnostics, risk stratification, medical & interventional management” – MDPI Journal. https://www.mdpi.com/2077-0383/13/16/4600 (mdpi.com)
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!