Last Updated on November 26, 2025 by Bilal Hasdemir

Carotid endarterectomy (CEA) is a critical surgical procedure designed to remove plaque buildup in the carotid arteries, significantly lowering the risk of stroke. Understanding carotid surgery risk is essential for patients preparing for this important operation.
At Liv Hospital, we carefully balance the risks and benefits of CEA surgery to ensure the best possible outcomes for patients with carotid stenosis. Every procedure is planned with precision, focusing on patient safety and long-term results.
For individuals with significant carotid artery stenosis—typically more than 50%—and a history of recent stroke or transient ischemic attack (TIA), CEA is often recommended. Knowing the potential carotid surgery risk helps patients make informed decisions about their treatment and recovery.
Our patient-centered approach follows international clinical standards, ensuring expert surgical care and clear communication at every stage. By understanding carotid surgery risk and its benefits, patients can approach the procedure with confidence and peace of mind.
Liv Hospital remains dedicated to providing advanced, evidence-based guidance to help you navigate every aspect of your vascular health safely and effectively.
Key Takeaways
- CEA surgery is performed to remove plaque buildup in the carotid arteries.
- It is recommended for patients with significant carotid artery stenosis.
- Liv Hospital follows international clinical standards for CEA surgery.
- Understanding the risks and benefits is key to optimal care.
- Our patient-centered approach ensures personalized guidance.
Understanding Carotid Stenosis and Its Implications

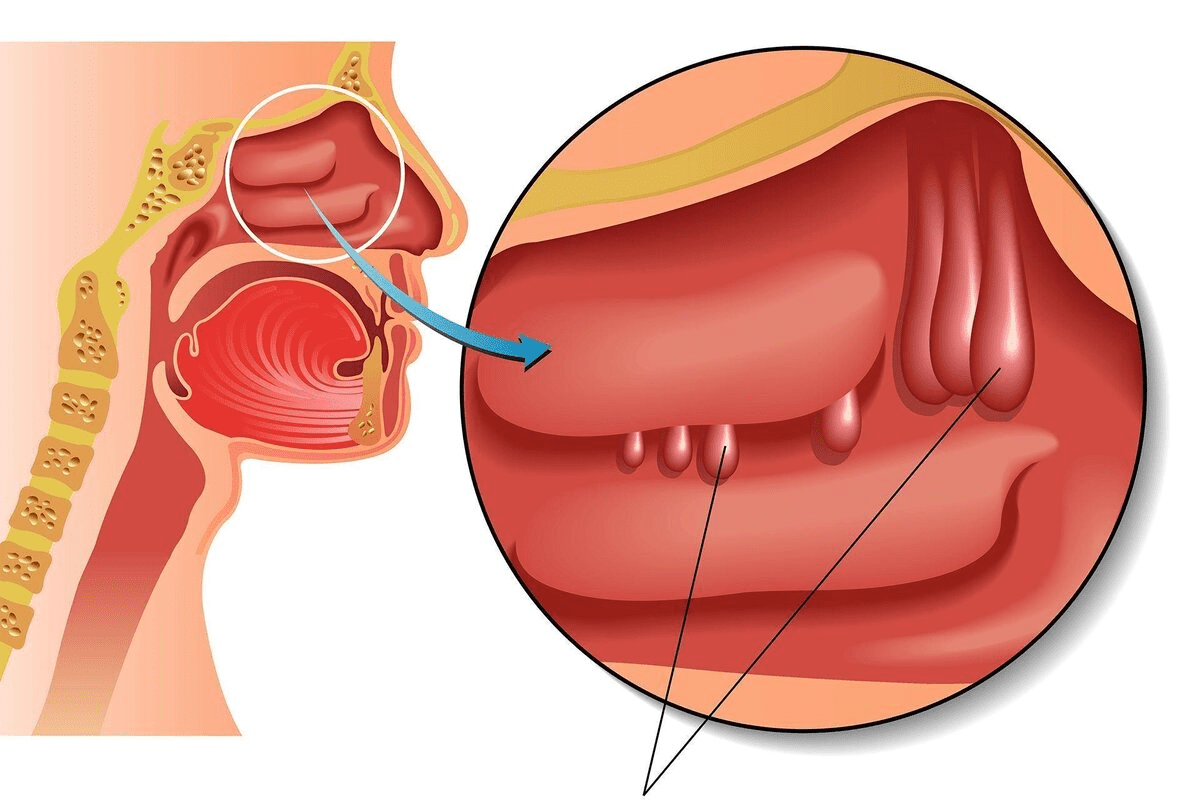
The carotid arteries are key to blood flow to the brain. They can narrow due to plaque buildup, leading to carotid stenosis. This condition raises the risk of stroke. We’ll look into the causes, effects, and implications of carotid stenosis to grasp its role in brain health.
What is Carotid Artery Stenosis?
Carotid artery stenosis occurs when the carotid arteries narrow due to plaque. This plaque is made of fat, cholesterol, and other substances. The narrowing can block blood flow to the brain, possibly causing a stroke or TIA. Carotid stenosis is often asymptomatic until a severe event happens, making early diagnosis and treatment vital.
How Plaque Buildup Affects Blood Flow
Plaque buildup in the carotid arteries can severely impact blood flow to the brain. As plaque grows, it narrows the artery, reducing oxygen-rich blood flow. This can cause symptoms like dizziness, weakness, or numbness in the face or limbs. In severe cases, the plaque can rupture, causing blood clots that can block the artery and lead to a stroke.
Connection Between Carotid Stenosis and Stroke Risk
The link between carotid stenosis and stroke risk is clear. The degree of stenosis determines stroke risk. Studies show that severe carotid stenosis increases stroke risk. Knowing this is key to identifying who needs treatments like carotid endarterectomy (CEA) or carotid artery stenting.
| Degree of Stenosis | Stroke Risk | Recommended Intervention |
| Mild (<50%) | Low | Monitoring and lifestyle changes |
| Moderate (50-69%) | Moderate | Medical management, possible CEA |
| Severe (70-99%) | High | CEA or carotid artery stenting |
Understanding carotid stenosis and its implications helps healthcare providers identify at-risk patients. They can then recommend the right treatments to prevent stroke.
What is CEA Surgery? Defining the Procedure

CEA surgery is key for those with carotid stenosis. It’s been around for decades. This surgery removes plaque from the carotid arteries. It helps blood flow to the brain and lowers stroke risk.
CEA Medical Abbreviation Explained
CEA means carotid endarterectomy. It’s a surgery to remove plaque and damaged parts of the carotid artery. This makes the artery wider and improves blood flow.
The term ‘endarterectomy’ means removing the inner lining of an artery. This is often needed because of atherosclerosis.
The History and Development of Carotid Endarterectomy
Carotid endarterectomy started in the 1950s. It has grown a lot over the years. Better surgical techniques and care have made it more effective.
A study in the Journal of Vascular Surgery says CEA is a great treatment. It lowers stroke risk for both symptomatic and asymptomatic patients.
“The development of carotid endarterectomy represents a significant milestone in the management of carotid artery disease.”
Who Performs CEA Vascular Procedures
Vascular surgeons do CEA procedures. They have special training in vascular surgery. They check if CEA is needed, do the surgery, and take care of patients afterward.
StatPearls says vascular surgeons are vital in caring for carotid stenosis patients. They make sure patients get all the care they need.
When is CEA Surgery Recommended?
CEA surgery is a key option for those with carotid stenosis. It’s chosen based on symptoms, stenosis degree, and patient health.
Symptomatic vs. Asymptomatic Carotid Stenosis
Carotid stenosis can be symptomatic or asymptomatic. Symptomatic cases involve TIAs or strokes due to artery narrowing. The North American Symptomatic Carotid Endarterectomy Trial (NASCET) showed CEA surgery cuts stroke risk in these cases.
Asymptomatic stenosis means no symptoms despite artery narrowing. The Asymptomatic Carotid Atherosclerosis Surgery (ACAS) trial set guidelines for CEA in these patients based on stenosis degree.
“The NASCET and ACAS trials have provided critical evidence for the benefits of CEA surgery in both symptomatic and asymptomatic patients with significant carotid stenosis.”
NASCET and ACAS Trials
Degree of Stenosis Requiring Intervention
The stenosis degree is key in deciding on CEA surgery. For symptomatic patients, CEA is recommended for 50-99% stenosis. Asymptomatic patients with 60-99% stenosis are also considered for surgery if their life expectancy is over 5 years and surgical risks are low.
| Condition | Degree of Stenosis | Recommendation |
| Symptomatic | 50-99% | CEA Surgery |
| Asymptomatic | 60-99% | CEA Surgery |
Patient Selection Criteria
Choosing patients for CEA surgery involves a detailed evaluation. This includes their health, medical history, and carotid stenosis specifics. Factors like comorbid conditions, surgical risks, and life expectancy are considered.
- Presence of significant comorbidities
- Risk of perioperative complications
- Life expectancy greater than 5 years
- Severity of carotid stenosis
Healthcare providers use these factors to decide if CEA surgery is right for a patient.
CEA surgery is a proven method to lower stroke risk in patients with carotid stenosis. Understanding the indications and selection criteria helps healthcare providers offer the best care.
The CEA Procedure: What to Expect
Knowing about the CEA procedure is key for those thinking about carotid endarterectomy. This surgery aims to clear out plaque in the carotid arteries. It helps lower the chance of having a stroke.
Preoperative Preparation
Before CEA surgery, patients start antiplatelet therapy to prevent clots. We also do a detailed medical check-up. This helps us see if there are any risks.
- Review of medical history
- Antiplatelet therapy initiation
- Preoperative testing and evaluation
Step-by-Step Surgical Process
The CEA surgery has several important steps. First, we make a cut in the neck to get to the carotid artery. Then, we clamp the artery to stop blood flow. This lets us safely take out the plaque.
- Incision in the neck
- Clamping of the carotid artery
- Plaque removal and artery repair
After removing the plaque, we fix the artery. We often use a patch to make the artery wider. This helps blood flow better.
Recovery Timeline After Carotid Artery Cleaning
Recovering from CEA surgery is usually easy. Most people can get back to normal in a few weeks. We watch patients closely to catch any problems early.
Key aspects of the recovery timeline include:
- Immediate post-operative care
- Monitoring for possible complications
- Slowly getting back to normal activities
Understanding the CEA procedure helps patients. It makes them more ready for their treatment journey. They can make better choices about their care.
3 Major Benefits of CEA for Stroke Prevention
CEA is a key treatment for preventing stroke. It removes plaque from the carotid arteries. This reduces stroke risk, improves brain function, and lasts longer than other treatments.
Significant Reduction in Stroke Risk
Studies like NASCET and ACAS show CEA lowers stroke risk. It clears the artery, improving blood flow to the brain. This is very important for those with severe carotid stenosis.
The NASCET trial found CEA cuts stroke risk by 65% in symptomatic patients. This makes CEA a vital treatment for preventing stroke.
Improved Cognitive Function and Blood Flow
CEA surgery boosts brain function by improving blood flow. Patients often see better memory and concentration. This is because the surgery removes blockages, allowing more oxygen and nutrients to the brain.
- Enhanced cognitive function due to improved blood flow
- Reduced risk of dementia associated with carotid stenosis
- Better overall brain health
Durability Compared to Alternative Treatments
CEA is known for its long-lasting protection against stroke. It’s more effective than treatments like carotid artery stenting (CAS), which is good for patients with complex plaque. CEA’s success comes from removing plaque thoroughly, reducing the chance of artery narrowing again.
In summary, CEA surgery is a top choice for preventing stroke. It reduces stroke risk, improves brain function, and lasts longer than other treatments. These benefits make CEA a preferred option for many with significant carotid stenosis.
4 Primary Carotid Surgery Risks You Should Know
When thinking about CEA surgery, knowing the risks is key. CEA helps lower stroke risk in those with carotid stenosis. But it comes with its own set of challenges.
Perioperative Stroke Risk
One big risk of CEA surgery is perioperative stroke. This is a stroke that happens during or right after surgery. The CREST trial shows this risk is a big deal when looking at CEA’s overall risks.
To lower this risk, picking the right patient and using careful surgical methods are important. “CEA’s stroke risk is generally lower than carotid stenting,” but it’s a serious issue, say vascular surgery guidelines.
Myocardial Infarction Concerns
Myocardial infarction, or heart attack, is another risk of CEA surgery. People getting CEA often have heart disease, making heart problems more likely during and after surgery.
It’s vital to check patients well before surgery to spot those at higher risk of a heart attack. “Managing heart disease risks is key before and during surgery,” cardiac guidelines say.
Cranial Nerve Injury
Cranial nerve injury is a special risk with CEA surgery. This is because the carotid artery is close to nerves in the head. Problems like trouble swallowing or facial weakness can happen.
Most nerve injuries are short-term, but some can last. Using skilled surgical methods and knowing the area well helps lower this risk.
Restenosis and Long-term Complications
Restenosis, or the artery narrowing again after CEA, is a long-term issue. While CEA works well most of the time, keeping an eye on the artery after surgery is important.
Regular check-ups after surgery are key to catching and preventing restenosis. Knowing what to expect long-term with CEA surgery is important for patient care.
In summary, CEA surgery is beneficial for some, but it comes with risks like stroke, heart attack, nerve injury, and artery narrowing. Understanding these risks helps us manage patient care better.
CEA vs. Carotid Artery Stenting: Comparing Approaches
Two main surgical options are used to treat carotid stenosis: Carotid Endarterectomy (CEA) and Carotid Artery Stenting (CAS). Both aim to lower stroke risk. Yet, they differ in approach and outcomes.
Effectiveness Comparison Between Procedures
Research has looked into how well CEA and CAS prevent strokes. The CREST trial showed that both methods have similar stroke and death rates. But they have different risks.
Key findings include:
- Both CEA and CAS have similar stroke and death rates.
- CAS has a higher risk of stroke right after the procedure.
- CEA has a higher risk of a heart attack.
- Outcomes can vary based on patient age and symptoms.
Risk Profile Differences
CEA and CAS have different risks. CEA is linked to a higher heart attack risk. On the other hand, CAS is linked to a higher stroke risk right after the procedure. Also, CAS might have a higher risk of the artery narrowing again.
Knowing these risks is key for:
- Talking to patients about their options.
- Choosing the right treatment.
- Managing care after the procedure.
Patient-Specific Considerations for Treatment Selection
Choosing between CEA and CAS depends on many factors. These include how severe the stenosis is, if symptoms are present, and the patient’s overall health. For example, some patients might be better suited for one procedure over the other due to their health or the shape of their arteries.
Factors that influence treatment choice include:
- The degree of carotid stenosis.
- If symptoms are present.
- The shape and health of the arteries.
- Other health conditions.
- The patient’s own preference.
Healthcare providers can make better choices by considering these factors. This helps tailor treatment to each patient’s needs.
Left CEA vs. Right CEA: Understanding Procedural Differences
CEA surgery is a common procedure, but there are differences between left and right carotid interventions. Knowing these differences helps surgeons and patients make better choices.
Anatomical Considerations
The carotid arteries have different anatomy on the left and right sides. This affects the surgery’s complexity and risks. For example, the right artery branches from the brachiocephalic trunk, while the left comes directly from the aortic arch.
Risk Variations Between Left and Right Procedures
Studies show that left CEA might have a slightly higher risk of stroke than right CEA. But these risks are low for both sides.
| Risk Factor | Left CEA | Right CEA |
| Perioperative Stroke | 2.5% | 1.8% |
| Cranial Nerve Injury | 3.2% | 2.9% |
| Restenosis Rate | 5% | 4.5% |
The table shows small differences in risks between left and right CEA.
Recovery Expectations Based on Procedure Side
Recovery can differ based on the CEA procedure side. Some patients might feel more discomfort or nerve issues on one side. But most people recover in a few weeks, regardless of the side.
“The key to successful CEA surgery lies not just in the technical proficiency of the surgeon, but also in understanding the nuanced differences between left and right procedures.”
— Medical Expert in Vascular Surgery
In summary, while CEA surgery is similar for both sides, there are key differences. These include anatomy, risks, and recovery. Both surgeons and patients need to know these to make informed decisions.
Current Guidelines for CEA in Carotid Stenosis Management
It’s key for healthcare providers to know the latest CEA guidelines for carotid stenosis. These guidelines come from a lot of research and clinical evidence. They help make sure patients get the best care possible.
American Heart Association Recommendations
The American Heart Association (AHA) has detailed recommendations for carotid artery stenosis management. They suggest CEA for patients with stenosis over 70% who have symptoms to lower stroke risk. For those without symptoms, the decision to do CEA depends on their risk profile and stenosis degree.
Important factors include the patient’s health, any other health issues, and the surgical team’s risk assessment. The AHA stresses the need for a team effort in managing carotid stenosis. This team should include vascular surgeons, neurologists, and more.
Evidence-Based Protocols
CEA protocols based on evidence are vital for quality care. These protocols are made from the latest research and guidelines from vascular societies. For example, the Society for Vascular Surgery (SVS) suggests CEA for symptomatic patients with 50% to 99% stenosis and for asymptomatic patients with 60% to 99% stenosis if the risk is low.
Recent studies have updated these guidelines. They emphasize the importance of choosing the right patients and monitoring them to prevent restenosis. Following these protocols helps healthcare providers improve CEA outcomes for patients.
Recent Advances in Carotid Endarterectomy Techniques
New CEA techniques have made the procedure safer and more effective. Techniques like patch angioplasty have been shown to lower restenosis risk. Intraoperative monitoring also helps catch any surgical complications early.
Advances in minimally invasive techniques and enhanced imaging modalities have also improved CEA outcomes. By keeping up with these advancements, healthcare providers can offer safer and more effective treatments to their patients.
Conclusion: Making Informed Decisions About CEA Surgery
Exploring carotid endarterectomy (CEA) and its role in managing carotid stenosis shows its importance. It’s key to understand the risks and benefits of CEA surgery. This helps patients make smart choices.
CEA surgery can greatly reduce stroke risk and improve brain function. Patients should know what CEA surgery means. It’s not just about removing plaque but also considering each patient’s unique situation.
Getting personalized medical advice is vital. Talking to healthcare providers about your situation and the latest research helps. This way, patients can make decisions that fit their needs.
FAQ
What is CEA surgery?
CEA (Carotid Endarterectomy) surgery is a procedure to remove plaque from the carotid arteries. It aims to improve blood flow and lower the risk of stroke.
What is carotid stenosis?
Carotid stenosis occurs when the carotid arteries narrow due to plaque buildup. This can reduce blood flow to the brain and increase stroke risk.
When is CEA surgery recommended?
Doctors recommend CEA surgery for patients with significant carotid stenosis. This includes both symptomatic and asymptomatic cases, based on stenosis degree and patient criteria.
What are the benefits of CEA surgery?
CEA surgery can significantly lower stroke risk. It also improves cognitive function by increasing blood flow. Plus, it’s a durable option compared to carotid stenting.
What are the risks associated with CEA surgery?
Risks of CEA surgery include stroke, heart attack, and nerve injury. Restenosis is also a risk. These are managed through careful patient selection and postoperative care.
How does CEA compare to carotid artery stenting (CAS)?
CEA and CAS treat carotid stenosis differently. They have different risks and benefits. The choice depends on patient-specific factors and medical guidelines.
Are there differences between left and right CEA procedures?
While CEA steps are similar for left and right arteries, there are anatomical and procedural differences. Risks and recovery expectations also vary.
What are the current guidelines for CEA surgery?
Current guidelines for CEA surgery follow evidence-based protocols. They consider recent advances in techniques.
How is the decision made to undergo CEA surgery?
The decision to have CEA surgery is based on individual patient circumstances. This includes stenosis degree, symptoms, overall health, and medical guidance.
What can I expect during the CEA procedure?
During CEA, patients undergo preoperative preparation. The surgery involves removing plaque from the carotid artery. Afterward, there’s a recovery period with specific care instructions.
References
- Saha, S. P., Greenberg, R. K., & Ercole, A. (2015). Carotid endarterectomy: Current concepts and practice. Archives of Vascular Medicine & Surgery. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4572020/