
Atrial fibrillation (AFib) and heart attacks are two serious heart issues. They are not the same. AFib is a heart rhythm problem that can raise your risk of a heart attack. We will look into how AFib impacts your heart health and what you can do to stay safe.
Studies show that people with AFib face a higher risk of heart attacks. They found a 63 percent increase in the risk of NSTEMI, a common heart attack type. At Liv Hospital, our team is here to help. We aim to give you the care you need to manage your AFib risk.
Key Takeaways
- AFib is a type of cardiac arrhythmia that can increase the risk of heart attack.
- Individuals with AFib are at a higher risk of developing NSTEMI, a common type of heart attack.
- Understanding the differences between AFib and heart attack is key for effective management.
- Comprehensive care is available for patients with AFib, including diagnosis, treatment, and management.
- Working with a healthcare team can help you mitigate risks associated with AFib.
Understanding Atrial Fibrillation: A Complete Overview
Atrial fibrillation (AFib) is a heart condition that affects millions globally. It poses serious risks to heart health. We will explore AFib’s causes, risk factors, and how common it is among different groups.
What Happens in the Heart During AFib
In atrial fibrillation, the heart’s upper chambers beat irregularly. This creates a quivering effect instead of a normal contraction. This irregularity can lead to symptoms like palpitations, shortness of breath, and fatigue.
The chaotic electrical activity in the atria disrupts the heart’s rhythm. It makes it harder for the heart to pump blood efficiently. This can cause clots to form.
Common Causes and Risk Factors
Several factors can lead to atrial fibrillation. These include:
- Age: The risk of developing AFib increases with age, after 65.
- Hypertension: High blood pressure is a significant risk factor for AFib.
- Heart disease: Conditions like coronary artery disease and heart valve problems can increase the risk.
- Obesity: Being overweight or obese is linked to a higher risk of developing AFib.
- Diabetes: People with diabetes are at a higher risk of developing AFib.
Prevalence of Atrial Fibrillation
Atrial fibrillation is the most common serious arrhythmia. It affects an estimated 33 million people worldwide. Its prevalence is expected to rise due to an aging population and better survival rates from heart attacks.
In the United States, AFib affects about 2.7 to 6.1 million people. This number is expected to more than double by 2030.
Understanding AFib’s prevalence and risk factors is key to developing effective prevention and treatment strategies. Recognizing its causes and symptoms can help individuals seek medical attention early. This can reduce the risk of complications.
Heart Attack Explained: Mechanism and Types
A heart attack happens when blood flow to the heart is blocked. This causes damage to the heart muscle. It’s a serious medical emergency that needs quick attention.
STEMI vs. NSTEMI Heart Attacks
Heart attacks are mainly two types: STEMI and NSTEMI. The main difference is in the electrocardiogram (ECG) findings and the heart muscle damage.
STEMI heart attacks have a complete blockage of a coronary artery. This causes a lot of damage to the heart muscle. An ECG shows an ST-segment elevation. NSTEMI heart attacks have a partial blockage. They cause less damage but are urgent medical cases.
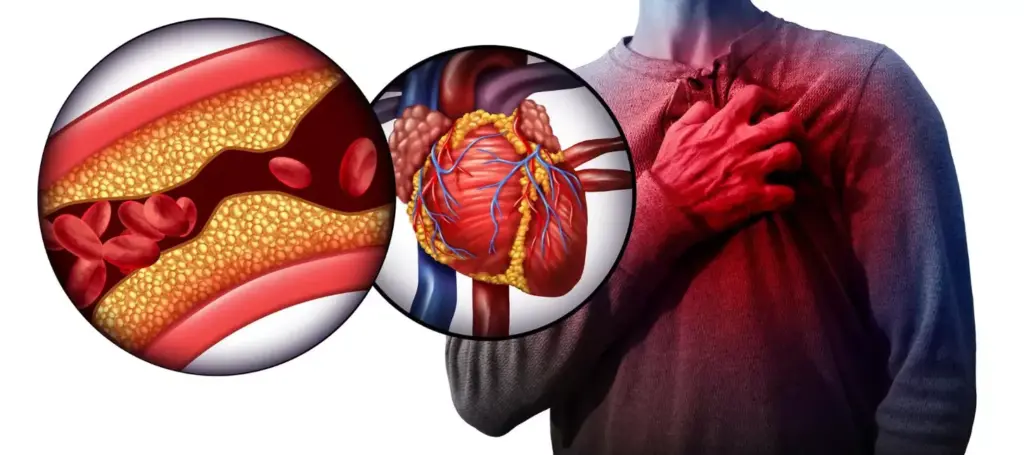
What Causes a Heart Attack
The main cause of a heart attack is a blockage of blood flow to the heart muscle. This usually happens when a blood clot forms on atherosclerosis (plaque) inside a coronary artery. Other factors include:
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
- Family history of heart disease
Risk Factors for Myocardial Infarction
Knowing the risk factors for heart attacks is key to prevention. Some major risk factors are:
| Risk Factor | Description |
|---|---|
| Age | Risk increases with age, after 45 for men and 55 for women. |
| Hypertension | High blood pressure can damage arteries, making them more prone to blockage. |
| Hyperlipidemia | High levels of LDL cholesterol can cause plaque in arteries. |
Understanding these risk factors and types of heart attacks helps manage health. It also helps seek timely medical help when needed.
Is AFib a Heart Attack? Understanding the Critical Differences
Atrial fibrillation (AFib) and heart attack are two different heart issues. AFib is about an irregular heart rhythm. A heart attack, on the other hand, is when blood flow to the heart is blocked.
Electrical Problem vs. Blood Flow Blockage
AFib is mainly an electrical issue with the heart’s rhythm. A heart attack, though, is caused by a blockage in the coronary arteries. This blockage stops blood from reaching the heart muscle.
Acute vs. Chronic Condition
A heart attack is an urgent situation that needs quick medical help. AFib, though, is often a long-term condition that needs ongoing care. Knowing these differences helps both patients and doctors make better choices.
Different Underlying Mechanisms
AFib happens because of abnormal electrical signals in the atria, causing irregular heartbeats. A heart attack, by contrast, is when blood flow to the heart is blocked for too long. This damage or death to heart muscle tissue occurs.
| Characteristic | AFib | Heart Attack |
|---|---|---|
| Primary Cause | Electrical disturbance in the heart | Blockage of coronary arteries |
| Onset | Often chronic | Acute event |
| Symptoms | Irregular heartbeat, palpitations | Chest pain, shortness of breath |
| Treatment Approach | Rhythm control, rate control, anticoagulation | Immediate medical intervention, possible thrombolysis or PCI |
The Connection Between AFib and Heart Attack Risk
Atrial fibrillation (AFib) is a known risk for heart attacks. It’s important to understand this link to manage heart health. Studies show that people with AFib face a higher risk of heart attacks, mainly non-ST-elevation myocardial infarction (NSTEMI).
Statistical Evidence of Increased Risk
Research has shown that AFib raises heart attack risk. Big studies have looked at this link, controlling for other factors. People with AFib are more likely to have heart attacks because of the irregular heartbeat and blood clot risk.
The 63% Higher Risk of NSTEMI
A study found that AFib raises the risk of NSTEMI by 63%. NSTEMI is a heart attack where a coronary artery is partially blocked. This highlights the need to watch and manage AFib to avoid heart problems.
Shared Risk Factors
AFib and heart attacks share risk factors like hypertension, diabetes, and coronary artery disease. Managing these factors is key to lowering AFib and heart attack risks. By tackling these common risks, people can greatly reduce their chance of heart issues.
How AFib Contributes to Heart Attack Vulnerability
Atrial fibrillation (AFib) makes heart attacks more likely in several ways. We’ll look at how AFib makes the heart more vulnerable to attacks. We’ll focus on the main factors that connect these two conditions.
Blood Stasis and Clot Formation
AFib increases heart attack risk mainly by causing blood stasis and clotting. The heart’s upper chambers don’t beat right, leading to blood pooling and clotting. These clots can then travel to the coronary arteries, causing a heart attack.
| Mechanism | Description | Risk |
|---|---|---|
| Blood Stasis | Pooling of blood in the heart due to irregular heartbeat | Clot formation |
| Clot Formation | Formation of blood clots in the heart | Embolism, heart attack |
| Embolism | Clots breaking loose and traveling to other parts of the body | Heart attack, stroke |
Strain on the Heart Muscle
AFib also strains the heart muscle, raising heart attack risk. The irregular, fast heartbeat of AFib can weaken the heart muscle. This leads to cardiomyopathy, where the heart can’t work right.
Inflammatory Processes
Inflammation is key in both AFib and heart attacks. Research shows inflammation helps create and keep AFib going. This inflammation can also lead to atherosclerosis, where plaque builds up in arteries, raising heart attack risk.
Knowing how these mechanisms work is vital for managing AFib and heart attack risk. By tackling the root causes and using the right treatments, we can lower heart attack risk. This improves overall heart health.
Recognizing Symptoms: AFib vs. Heart Attack
Atrial fibrillation (AFib) and heart attacks are serious heart issues. They have different symptoms, but some can be similar. It’s important to know the differences to get the right medical help.
Distinctive Symptoms of Each Condition
AFib symptoms include palpitations, shortness of breath, and feeling tired. On the other hand, a heart attack usually causes chest pain or discomfort. This pain can spread to the arm, neck, or jaw.
Overlapping Symptoms That Cause Confusion
Both AFib and heart attacks can make you feel short of breath and tired. This makes it hard to tell them apart. But, it’s key to remember that their causes are different.
When to Seek Emergency Medical Attention
If you have severe chest pain, trouble breathing, or faint, get help right away.
| Symptom | AFib | Heart Attack |
|---|---|---|
| Palpitations | Common | Rare |
| Chest Pain | Occasional | Common |
| Shortness of Breath | Common | Common |
Chest Pain in AFib vs. Heart Attack: Important Distinctions
Chest pain can be a symptom of both AFib and heart attack. But, the way it feels is different. Knowing these differences helps doctors diagnose and treat correctly.
Characteristics of AFib-Related Chest Discomfort
AFib chest pain feels like palpitations or irregular heartbeat, not just pain. People might feel their heart skipping beats or racing. This pain can come and go and isn’t always linked to exercise.
- May feel like palpitations or irregular heartbeat
- Often intermittent
- Not necessarily related to physical exertion
Classic Heart Attack Chest Pain Patterns
Heart attack chest pain feels like pressure or tightness in the chest. It’s often described as squeezing or crushing. This pain can spread to the arms, back, neck, jaw, or stomach.
- Usually feels like pressure or tightness
- Can radiate to other parts of the body
- Often associated with physical exertion or emotional stress
Diagnostic Approaches for Chest Pain
Getting the right chest pain diagnosis is key to tell AFib from heart attack. Doctors use:
- Electrocardiogram (ECG) to check heart rhythm and look for problems
- Blood tests to find signs of heart damage
- Imaging tests like echocardiography or coronary angiography to see the heart’s shape and how it works
Understanding the differences in chest pain helps doctors choose the best tests and treatments.
Long-Term Heart Damage: Comparing AFib and Heart Attack
It’s important to know how AFib and heart attacks affect the heart over time. Both can cause lasting damage, but in different ways.
Effects of AFib on Heart Structure
Atrial fibrillation can change the heart’s shape. The irregular beats can make the atria bigger, which might lower heart function. It also raises the risk of blood clots, leading to stroke or other problems.
AFib can also lead to heart failure if not treated. People with AFib need to work with their doctors to manage symptoms and avoid long-term harm.
Permanent Damage from Myocardial Infarction
A heart attack kills heart muscle cells because of blocked blood flow. This damage is permanent and can cause scarring in the heart. The damage’s extent depends on the attack’s severity and length.
After a heart attack, the heart tries to adjust by remodeling. But this can sometimes cause more problems, like heart failure.
Cumulative Effects on Heart Health
Having both AFib and a heart attack can severely affect the heart. The heart’s structure changes from AFib and scarring from the heart attack can worsen heart function.
Managing both conditions needs a detailed plan. This includes medicines, lifestyle changes, and sometimes procedures like catheter ablation or pacemaker implantation.
| Condition | Short-Term Effects | Long-Term Effects |
|---|---|---|
| AFib | Irregular heartbeats, palpitations | Enlargement of atria, heart failure |
| Heart Attack | Chest pain, shortness of breath | Scarring, heart failure |
Diagnostic Methods: Differentiating Between AFib and Heart Attack
Diagnosing AFib and heart attack requires different methods. Each uses various tools to make sure the right treatment is given. We will look at how these conditions are distinguished.
ECG Findings in Each Condition
An electrocardiogram (ECG) is key for both AFib and heart attack. AFib shows an irregular rhythm without P waves and changing heart rates. Heart attack ECGs might show ST-segment elevation or depression, showing how severe the heart damage is.
Blood Tests and Biomarkers
Blood tests are essential for heart attack diagnosis, focusing on cardiac biomarkers like troponin. High troponin levels mean heart muscle damage. AFib diagnosis doesn’t rely on specific biomarkers but blood tests can spot underlying issues like thyroid problems.
Advanced Imaging Techniques
Tests like echocardiography and cardiac MRI offer detailed heart views. They help find damaged heart muscle, check heart function, and spot complications from both AFib and heart attack.
Using these diagnostic methods, doctors can tell AFib from heart attack. This ensures the right treatment is given.
Treatment Approaches: Different Strategies for Different Conditions
Managing AFib and heart attack well needs a deep understanding of treatment options. We’ll look at how to handle these conditions through lifestyle changes, medicines, and procedures.
Managing AFib to Reduce Heart Attack Risk
It’s key to manage AFib to lower heart attack risk. This means making lifestyle changes, taking medicines, and sometimes, getting procedures to fix the heart rhythm.
- Lifestyle Modifications: People with AFib should eat well, exercise, quit smoking, and drink less alcohol.
- Medications: Doctors often prescribe anticoagulants and anti-arrhythmics. Anticoagulants prevent strokes by stopping blood clots. Anti-arrhythmics control the heart’s rhythm.
- Procedures: Sometimes, cardioversion or catheter ablation are needed to fix the heart rhythm.
Acute Heart Attack Interventions
Quick actions are vital to protect the heart during a heart attack. These include emergency angioplasty, thrombolytic therapy, and CABG.
- Emergency angioplasty opens blocked arteries to restore blood flow.
- Thrombolytic therapy uses drugs to dissolve heart attack-causing clots.
- CABG is surgery that bypasses blocked arteries.
Medications That Address Both Conditions
Some medicines help with both AFib and heart attack. These include beta-blockers and antiplatelet agents.
- Beta-Blockers: These drugs lower the heart’s workload and need for oxygen, helping both conditions.
- Antiplatelet Agents: These prevent blood clots that can lead to heart attacks.
| Treatment Approach | AFib | Heart Attack |
|---|---|---|
| Lifestyle Modifications | Heart-healthy diet, regular exercise, smoking cessation | Heart-healthy diet, regular exercise, smoking cessation |
| Medications | Anticoagulants, anti-arrhythmics | Antiplatelet agents, beta-blockers, thrombolytics |
| Procedures/Interventions | Cardioversion, catheter ablation | Emergency angioplasty, CABG |
Prevention Strategies: Reducing Your Risk of AFib and Heart Attack
Being proactive about heart health can lower the risk of atrial fibrillation (AFib) and heart attacks. By making lifestyle modifications and managing risk factors, you can control your heart health.
Lifestyle Modifications for Heart Health
Healthy lifestyle choices are key to preventing AFib and heart attacks. This includes:
- Regular Exercise: Doing moderate activities like brisk walking, cycling, or swimming for 150 minutes a week.
- Balanced Diet: Eating lots of fruits, veggies, whole grains, and lean proteins. Avoid too much saturated fats, sodium, and sugars.
- Stress Management: Using stress-reducing methods like meditation, yoga, or deep breathing.
- Avoiding Tobacco: Quitting smoking and staying away from secondhand smoke.
- Limiting Alcohol Consumption: Drinking alcohol in small amounts, if at all.
Medical Management of Risk Factors
Managing risk factors well is key to preventing AFib and heart attacks. This includes:
- Hypertension Management: Keeping blood pressure in check through lifestyle changes and, if needed, medication.
- Cholesterol Management: Keeping cholesterol levels healthy through diet, exercise, and, if needed, medication.
- Diabetes Management: Controlling blood sugar levels through lifestyle changes and, if needed, medication.
- Obesity Management: Staying at a healthy weight through diet and exercise.
Monitoring and Follow-up Recommendations
Regular check-ups and follow-ups with healthcare providers are vital. This includes:
- Regular visits to monitor blood pressure, cholesterol levels, and other risk factors.
- Following prescribed medications and treatment plans.
- Knowing the signs and symptoms of AFib and heart attacks. Seek medical help right away if you notice them.
By following these prevention strategies, you can greatly lower your risk of AFib and heart attacks. This improves your overall heart health.
Conclusion: Living Well with AFib While Minimizing Heart Attack Risk
Managing atrial fibrillation (AFib) well is key to lowering heart attack risk. We’ve looked into how AFib affects heart health. It’s important to know how these conditions are connected.
To live well with AFib, you need a full plan. This includes changing your lifestyle, getting medical help, and keeping an eye on your health. A heart-healthy lifestyle can lower your heart attack risk and boost your overall health.
Managing AFib right means working with your doctor to create a plan just for you. This might include medicines, procedures, and lifestyle changes. These should fit your needs and health situation.
Being active in managing AFib can help you avoid heart attacks and live well. It’s vital to stay informed, follow your treatment plan, and choose a healthy lifestyle. This way, you can manage AFib and lower your heart attack risk effectively.
Can atrial fibrillation cause a heart attack?
Yes, AFib can raise your risk of heart attack, mainly NSTEMI. This is because of shared risk factors like blood stasis and inflammation.
What is the difference between atrial fibrillation and a heart attack?
AFib is an electrical issue causing irregular heart rhythm. A heart attack, on the other hand, is a blockage of blood flow to the heart, damaging the heart muscle.
Does AFib mean I will have a heart attack?
Having AFib doesn’t mean you’ll definitely have a heart attack. But, it does increase your risk. Managing AFib and risk factors can lower this risk.
Can AFib cause chest pain?
AFib can lead to chest discomfort or pain. But, this pain is different from the severe chest pain of a heart attack. You need a diagnosis to know the cause.
How does AFib affect the heart over time?
AFib can change the heart’s structure and function over time. This can cause long-term damage. It’s important to manage AFib to prevent this damage.
What are the symptoms of AFib and heart attack?
AFib symptoms include an irregular heartbeat and palpitations. Sometimes, it causes chest discomfort. Heart attack symptoms are severe chest pain and shortness of breath. These symptoms can be confusing, so it’s important to get medical help quickly.
Can heart arrhythmia cause a heart attack?
Yes, certain heart arrhythmias like AFib can increase heart attack risk. This is due to blood stasis and inflammation.
How are AFib and heart attack diagnosed?
Doctors use an electrocardiogram (ECG), blood tests, biomarkers, and imaging techniques to diagnose AFib and heart attack.
What are the treatment approaches for AFib and heart attack?
Treatment for AFib includes managing it to lower heart attack risk. For heart attack, there are acute interventions and medications. Tailored treatment plans are key.
Can lifestyle modifications reduce the risk of AFib and heart attack?
Yes, a healthy diet, regular exercise, and managing risk factors can lower the risk of both AFib and heart attack.
Is AFib a chronic condition?
AFib is usually a chronic condition. It needs ongoing management to prevent complications, including heart attack.
How can I minimize my risk of heart attack if I have AFib?
To lower heart attack risk with AFib, manage shared risk factors, follow treatment plans, and make lifestyle changes to support heart health.



































