Last Updated on November 26, 2025 by Bilal Hasdemir
What is the best back fracture treatment? Learn how long it takes to heal a broken back and what the essential recovery process involves. A broken back is a serious injury. It can happen from trauma, osteoporosis, or falls. The healing time for a broken back depends on many things. These include your age, health, and how bad the injury is.
Understanding the recovery process is key for those with a broken back. Studies show that healing a spinal fracture can take 6 to 12 weeks on average. But, this time can be longer based on your health and the effectiveness of the treatment.
At Liv Hospital, we focus on our patients. We give them care and advice based on the latest research. Our team creates a recovery plan just for you. This plan aims to help you heal the best way possible.
Key Takeaways
- The average healing time for a spinal fracture is between 6 to 12 weeks.
- The recovery process varies depending on age, overall health, and injury severity.
- A personalized recovery plan is key for the best healing.
- Liv Hospital offers patient-centered care and evidence-based advice.
- Good treatment can really help with how fast you recover.
What Constitutes a Broken Back: Types and Definitions

A broken back, or vertebral fracture, is when one or more vertebrae break. This can happen due to trauma, osteoporosis, or other spine issues.
Knowing the different types of vertebral fractures is key. It helps doctors choose the right treatment and predict how well you’ll recover. We’ll look at the various classifications and what they mean.
Vertebral Fracture Classifications
Vertebral fractures are sorted by where in the spine they happen and how severe they are. The spine has three main parts: the neck, upper back, and lower back. Each part can have different types of fractures.
“The classification of a vertebral fracture is key for knowing how stable the spine is and what treatment to use.”
— Orthopedic Specialist
- Compression Fractures: These happen when a vertebra collapses, often because of osteoporosis.
- Burst Fractures: These are more severe, where the vertebra breaks into pieces.
- Flexion-Distraction Fractures: These happen from a mix of bending and stretching forces, common in car accidents.
- Fracture-Dislocations: These are fractures with big displacements, which can harm the spinal cord.
Difference Between Fractures and Dislocations
It’s important to tell fractures and dislocations apart. A fracture is a bone break, while a dislocation is when a joint or vertebra moves out of place.
| Characteristics | Fractures | Dislocations |
| Nature of Injury | Break in the bone | Displacement of vertebrae or joint |
| Stability | Can be stable or unstable | Often unstable |
| Treatment Approach | Varies from conservative to surgical | Usually needs immediate care, possibly surgery |
Severity Scales and Their Impact on Recovery
Doctors use scales to measure how severe a vertebral fracture is. This helps predict how well you’ll recover. Knowing if a fracture is stable or unstable is very important, as unstable ones might need surgery.
The recovery time depends a lot on the fracture’s severity and type. Understanding these classifications helps doctors create treatment plans that fit each patient’s needs. This increases the chances of a good recovery.
Common Causes of Back Fractures
Trauma, osteoporosis, and certain activities are common causes of back fractures. Knowing these causes helps in prevention and treatment.
Traumatic Injuries and Accidents
Traumatic injuries often lead to back fractures. These can happen in car accidents, falls, sports injuries, or violent acts. Medical News Today says trauma is the top reason for broken backs.
These incidents can put a lot of pressure on the spine, causing fractures. The severity of the fracture depends on the force and how it hits the spine.
Osteoporosis and Age-Related Fractures
Osteoporosis is a big cause of back fractures in older adults. It makes bones weak, making them more likely to break.
“Osteoporosis is a major risk factor for vertebral fractures, which can occur even without significant trauma.”
Fractures from osteoporosis often happen in the thoracic and lumbar spine. They can lead to chronic pain and disability.
Sports and High-Impact Activities
Participating in sports and high-impact activities raises the risk of back fractures. Activities like heavy lifting, bending, or high-impact landings stress the spine.
| Sport/Activity | Risk Level | Common Fracture Type |
| Gymnastics | High | Compression Fracture |
| Football | High | Burst Fracture |
| Weightlifting | Moderate | Stress Fracture |
Falls and Their Impact on the Spine
Falls are a common cause of back fractures, mainly in the elderly and young children. The type of fracture depends on how the person lands and the surface they fall on.
Preventing falls and managing osteoporosis are key to reducing back fracture risk. Understanding causes and taking preventive steps can greatly improve outcomes for those at risk.
If You Break Your Back: Immediate Consequences and Emergency Response
A broken back sets off a chain of reactions that need quick action. The body’s first response can greatly affect the injury’s outcome.
Initial Physiological Responses
When you break your back, your body reacts with pain, inflammation, and shock. The severity of these reactions depends on the fracture’s nature and location. Pain management is key in the early stages to avoid more harm.
Potential Neurological Implications
A broken back can lead to serious neurological implications, like spinal cord damage. This can cause numbness, tingling, or weakness in limbs. It can also lead to bladder or bowel problems. Knowing these risks is vital for proper care.
Emergency Medical Procedures
The emergency response to a broken back includes stabilizing the patient. This is to prevent further injury, like damage to the spinal cord. Immobilization with a backboard or cervical collar is common. The patient is then taken to a hospital for a detailed assessment.
First 24-48 Hours After Injury
The first 24-48 hours after a back injury are very important. Medical teams watch the patient closely, manage pain, and start treatment. This time is critical for preventing further problems and starting the healing process.
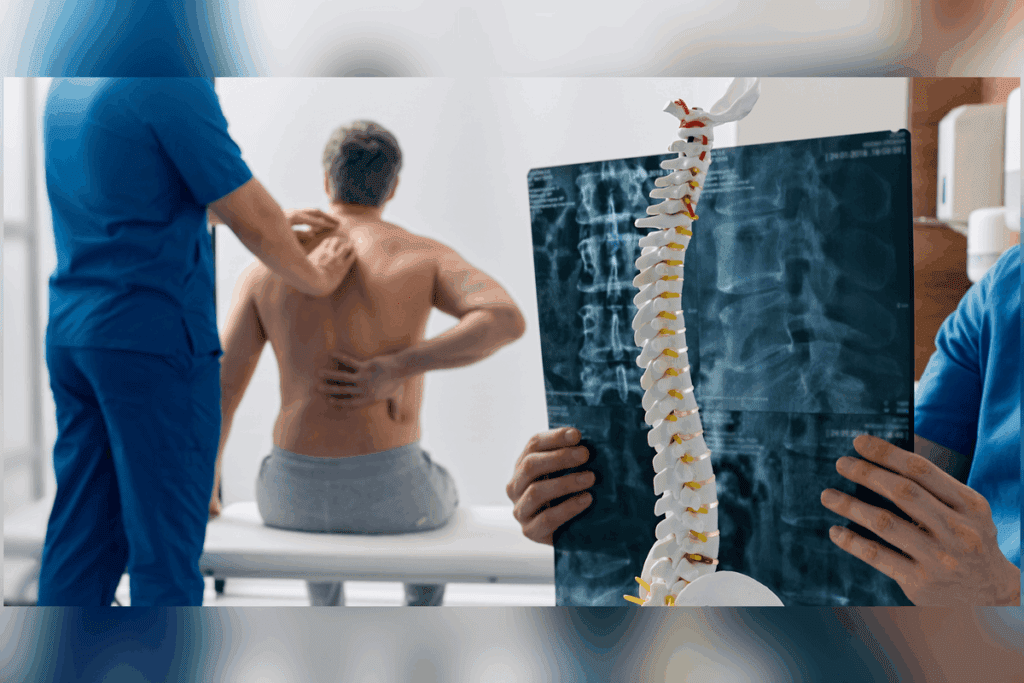
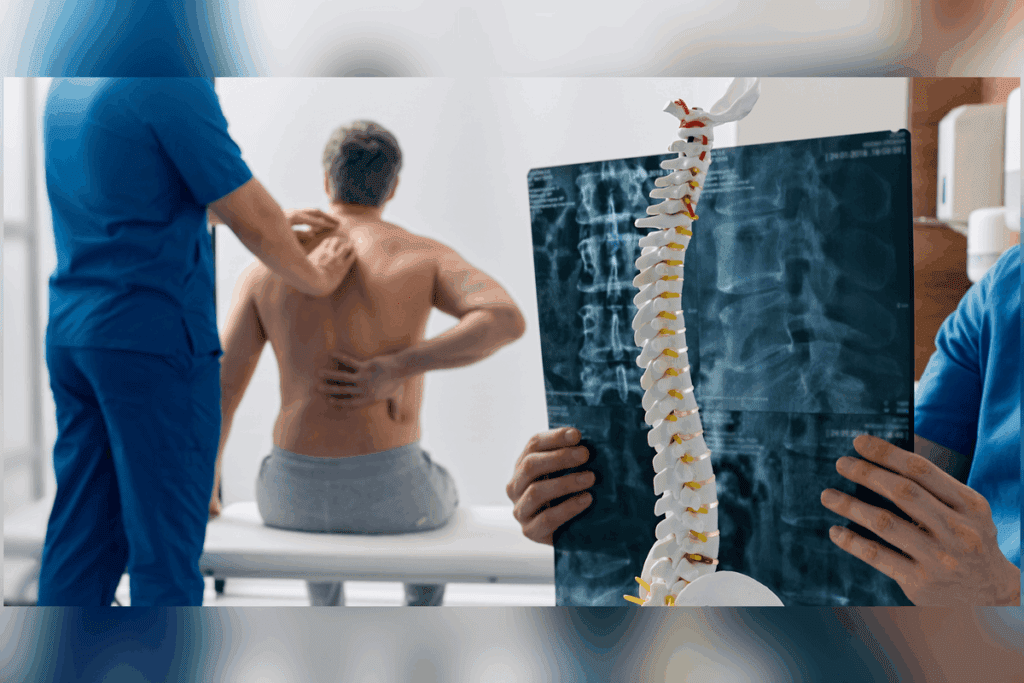
Diagnosing a Broken Back: Signs and Medical Assessment
Figuring out if someone has a broken back involves looking for symptoms and doing detailed medical checks. When someone might have a vertebral fracture, doctors need to check how bad the injury is.
Recognizing Symptoms of Vertebral Fractures
Vertebral fractures can show different symptoms based on how bad and where the fracture is. Common signs are severe back pain, trouble moving, and sometimes, numbness or weakness in the limbs. It’s important for people to see a doctor if they have these symptoms, even more so after a big injury.
Diagnostic Imaging Techniques
Getting a correct diagnosis of a broken back depends a lot on imaging tests. The main ones used are:
- X-rays: Good for the first check and finding fractures.
- CT scans: Show detailed bone pictures and are great for complex fractures.
- MRI scans: Best for soft tissue injuries, like spinal cord damage.
These tests help doctors see how bad the injury is and decide on the best treatment.
Neurological Evaluation Process
Checking the nerves and spinal cord is key when someone has a vertebral fracture. This check looks at motor function, sensory perception, and reflexes. Knowing the results helps doctors figure out how serious the injury is and what treatment to use.
| Diagnostic Tool | Primary Use | Benefits |
| X-ray | Initial fracture detection | Quick, widely available |
| CT Scan | Detailed bone assessment | High-resolution images |
| MRI | Soft tissue evaluation | Excellent for nerve assessment |
By looking at symptoms, doing imaging tests, and checking the nerves, doctors can accurately diagnose and treat vertebral fractures. This helps patients get better and recover faster.
Back Fracture Treatment Options and Approaches
Treatment for back fractures depends on the injury’s type and the patient’s health. Most people with spine compression fractures don’t need surgery, says NYU Langone Health. Instead, doctors often suggest medication, back braces, and exercises to ease pain and keep patients active.
Conservative Management Strategies
For stable fractures, the first treatment is usually conservative management. This includes:
- Pain management through medication
- Use of custom-fit back braces for support
- Modified activity levels to avoid exacerbating the injury
- Physical therapy to maintain mobility and strength
“Conservative management is often effective in treating stable fractures, allowing patients to recover without surgical intervention,” says a leading orthopedic specialist. Early mobilization and appropriate bracing can significantly improve outcomes.
Surgical Interventions for Unstable Fractures
For severe or unstable fractures, surgery might be needed. Surgical options include:
- Vertebroplasty or kyphoplasty to stabilize the vertebrae
- Spinal fusion to join vertebrae together
- Decompression surgery to relieve pressure on the spinal cord or nerves
Surgery decisions depend on the fracture’s severity, the patient’s health, and any neurological symptoms. The goal of surgery is to stabilize the spine, alleviate pain, and prevent further injury.
Medication Protocols for Pain and Healing
Managing pain is key in treating back fractures. Medication protocols may include:
- Over-the-counter pain relievers for mild to moderate pain
- Prescription medications for more severe pain
- Medications to prevent or treat osteoporosis, if applicable
It’s essential to follow a healthcare provider’s guidance on medication use to minimize side effects and ensure effective pain management. A well-managed pain regimen can significantly improve the recovery experience.
“The key to successful treatment is a personalized approach that addresses the individual’s specific needs and health status.”
— Orthopedic Specialist
Average Healing Timeframes for Different Types of Back Fractures
Knowing how long it takes for back fractures to heal is key. The time it takes for a spinal fracture to heal is usually 6 to 12 weeks. But, this time can change based on several things.
Standard Recovery Timeline
Most back fractures take 6 to 12 weeks to heal. During this time, the body fixes the fracture and the spine gets stronger. Younger, healthier people might heal in 4 to 6 weeks.
“The recovery process is not just about the fracture itself, but also about the overall health and well-being of the patient,” says a leading orthopedic specialist. This shows why it’s important to think about a person’s health when guessing how long it will take to heal.
Healing Expectations by Fracture Type
Different fractures heal at different rates. For example:
- Compression fractures, often linked to osteoporosis, heal in 8 to 12 weeks.
- Burst fractures, which are more serious, can take up to 3 to 6 months to fully heal.
- Flexion-distraction injuries, also known as seatbelt fractures, usually need 6 to 12 weeks to recover.
Age and Health Factors Affecting Recovery Speed
Age and health are big factors in how fast someone heals. Older people or those with health problems might heal slower because of weaker bones and other health issues. Younger people with no health problems usually heal faster.
| Fracture Type | Typical Healing Time | Factors Influencing Recovery |
| Compression Fracture | 8-12 weeks | Osteoporosis, age |
| Burst Fracture | 3-6 months | Severity of fracture, neurological involvement |
| Flexion-Distraction Injury | 6-12 weeks | Associated injuries, overall health |
Realistic Milestones During the Healing Process
Knowing the healing milestones can keep patients motivated and on track with their treatment. Important milestones include:
- Initial stabilization of the fracture (0-4 weeks)
- Gradual increase in mobility and strength (4-8 weeks)
- Return to normal activities with caution (8-12 weeks)
By knowing these milestones, patients can better understand their recovery timeline and work towards a successful recovery.
The Initial Recovery Phase: Pain Management and Stabilization
Managing pain and stabilizing the spine are key in the first steps after a back fracture. We aim to control pain, avoid further injury, and prepare for a good recovery.
Pain Control Strategies and Medications
Pain management is vital in the early recovery. We use different strategies and medicines to ease pain. These include:
- Over-the-counter pain relievers: Like acetaminophen or ibuprofen for mild to moderate pain.
- Prescription medications: For more severe pain, stronger drugs are used.
- Muscle relaxants: To handle muscle spasms that can happen with a broken back.
It’s important to work with healthcare providers to find the right pain medicines. A pain management specialist says, “Effective pain control is key for patients to stay mobile and comfortable while healing.”
Bed Rest Guidelines: Duration and Positioning
Bed rest is often needed right after a back fracture. But, how long and how to position are important to avoid more harm and help healing.
- Duration: Bed rest should be as brief as possible, usually no more than a few days, to avoid issues like blood clots or muscle loss.
- Positioning: Patients are often told to lie on their back with a pillow under their knees to ease spine strain.
Early Mobilization Techniques
Starting to move early is important in recovery. Gentle exercises help keep flexibility and strength. Techniques include:
- Log rolling: A way to turn in bed that keeps the spine straight.
- Gentle stretching: To keep flexibility and reduce stiffness.
Preventing Secondary Complications
It’s critical to prevent other problems during the early recovery phase. This includes:
- Monitoring for neurological changes: Like numbness, tingling, or weakness in the limbs.
- Preventing blood clots: With anticoagulant medicines or compression stockings.
- Maintaining a healthy diet: To support bone healing and overall health.
By managing pain, following bed rest guidelines, using early mobilization, and preventing other issues, patients can do well in the initial recovery phase. This helps set the stage for a successful recovery from a broken back.
Bracing and External Support Methods
Braces are often used to treat back fractures, like compression fractures. They provide the needed support and stability as the spine heals.
NYU Langone Health says specialists can make a brace to fit the spine. This ensures the brace meets the patient’s specific needs.
Types of Braces for Different Fracture Locations
Braces vary based on the fracture’s location and severity. For example, thoracic lumbar sacral orthotics (TLSO) are used for thoracic or lumbar fractures. These braces limit motion and support the area, helping it heal.
A jewett brace is sometimes recommended for more stability and support.
Duration of Brace Wear by Fracture Type
The time a patient wears a brace varies by fracture type. For compression fractures, it’s usually 6 to 12 weeks. But, this can change based on healing progress and doctor’s advice.
“The goal of bracing is to provide sufficient support to the spine during the healing process, reducing pain and preventing further injury.” –
Orthopedic Specialist
Transitioning Away From External Support
As the fracture heals, patients start wearing the brace less. This is done through regular checks to see if the spine is strong enough. Physical therapy helps strengthen back muscles and improve posture.
Stopping external support needs careful planning. Patients are told to slowly reduce brace use, with their doctor’s help.
Physical Therapy and Rehabilitation Process
After a back fracture, a good physical therapy plan is key for recovery. We know everyone’s recovery path is different. So, our rehab programs are made just for you.
Early Phase Rehabilitation Exercises
In the first steps of recovery, we focus on gentle exercises. These help with healing and keep the spine stable. The early phase rehabilitation exercises stop muscle loss and boost blood flow.
- Breathing exercises to improve lung capacity
- Gentle stretching to maintain flexibility
- Isometric exercises to strengthen core muscles without straining the spine
Progressive Strength and Mobility Training
As you get better, we add progressive strength and mobility training. This part makes your spine stronger and improves how you move. It includes exercises that make your muscles work harder and increase your range of motion.
- Gradually increasing resistance to strengthen back and abdominal muscles
- Improving flexibility through controlled stretching exercises
- Enhancing balance and coordination to reduce the risk of falls
NYU Langone’s Rusk Rehabilitation says physical therapy is great for making back muscles stronger. Our programs are based on this, giving you the tools for a full recovery.
“Rehabilitation after a spinal fracture is not just about healing the bone; it’s about restoring function and improving quality of life.”
Expert in Physical Medicine and Rehabilitation
Pain Management During Rehabilitation
Managing pain well is key during rehab. We work with you to create a pain plan. This might include medicine, physical treatments, and other therapies.
Measuring Progress and Adjusting Programs
We always measure progress and tweak your program as needed. This makes sure you’re reaching your goals and getting better steadily.
| Rehabilitation Phase | Goals | Interventions |
| Early Phase | Maintain spinal stability, prevent muscle atrophy | Breathing exercises, gentle stretching, isometric exercises |
| Progressive Phase | Enhance strength, improve mobility | Resistance training, flexibility exercises, balance training |
Long-Term Recovery and Return to Normal Activities
Recovering from a broken back takes time, effort, and a good plan. First, we focus on managing pain and stabilizing the injury. Then, we work on building strength, improving movement, and getting back to our daily lives.
Gradual Reintroduction of Daily Activities
Slowly getting back to daily tasks is key to long-term recovery. Medical News Today says a tailored exercise program helps. It helps avoid injury and ensures a smooth return to normal life.
- Start with low-intensity activities such as walking or light stretching.
- Gradually increase the intensity and duration based on comfort and tolerance.
- Monitor for any signs of pain or discomfort that may indicate overexertion.
Return to Work Timeline and Considerations
Going back to work after a back injury depends on many things. This includes the job type, injury severity, and overall health. Desk jobs might be easier to return to than jobs that are very physical.
Key considerations for returning to work include:
- Assessing the physical demands of the job and making necessary adjustments.
- Discussing a gradual return to work plan with the employer.
- Ensuring proper ergonomics and workplace safety to prevent re-injury.
Permanent Lifestyle Modifications
Some back injuries might mean making long-term changes to avoid future problems. This could be keeping a healthy weight, exercising regularly, and improving posture.
- Adopting a balanced diet rich in calcium and vitamin D to support bone health.
- Engaging in regular physical activity, such as walking or swimming, to maintain strength and flexibility.
- Practicing good posture and lifting techniques to reduce strain on the back.
Long-Term Prognosis After Back Fracture
The outlook after a back fracture varies. It depends on the injury’s severity, treatment success, and overall health. Most people recover well, but some might have ongoing pain or limited mobility.
Factors influencing long-term prognosis include:
- The severity and type of the fracture.
- The presence of any underlying health conditions, such as osteoporosis.
- Adherence to the rehabilitation program and lifestyle modifications.
Understanding these factors and following a healthcare plan can improve recovery and long-term outcomes.
Conclusion: Navigating the Journey to Recovery
Understanding the recovery process is key for those with a broken back. The healing journey is complex and varies greatly among people. The time it takes to heal can range from weeks to months, based on the fracture’s severity and health.
Following a healthcare provider’s advice is vital during recovery. This ensures the best outcome and avoids complications. The journey includes physical healing and adapting to new habits, sometimes needing rehabilitation to regain strength.
Being patient and persistent is critical during recovery. Healing a broken back takes time, and knowing this helps manage expectations. With medical treatment, rehabilitation, and lifestyle changes, one can overcome the challenges of a broken back.
FAQ
What is a broken back, and how is it defined?
A broken back, or vertebral fracture, happens when a vertebra in the spine cracks or breaks. This can be due to injuries, osteoporosis, or falls.
How long does it take to heal a broken back?
The healing time for a broken back varies. It depends on the fracture’s severity and the person’s health. It usually takes 6 to 12 weeks to start healing, but full recovery can take months.
What are the common causes of back fractures?
Back fractures can be caused by accidents, osteoporosis, sports injuries, or falls. These causes lead to different types of fractures, affecting the spine in various ways.
What are the immediate consequences of breaking one’s back?
Breaking one’s back can cause pain, shock, and neurological issues. It’s important to follow emergency medical procedures. The first 24-48 hours are critical.
How is a broken back diagnosed?
To diagnose a broken back, doctors look for symptoms and use imaging like X-rays or MRI. They also do a neurological evaluation to assess the injury.
What are the treatment options for back fractures?
Treatment for back fractures includes non-surgical and surgical options. Medication is used for pain and healing. The best treatment depends on the fracture’s severity and type.
What is the role of bracing and external support in recovery?
Bracing and external support, like wearing a brace, help stabilize the spine. The type and duration of brace use depend on the fracture’s location and severity.
What is the physical therapy and rehabilitation process like?
Physical therapy and rehabilitation start with early exercises. They progress to strength and mobility training. Pain management and measuring progress are also key.
How long does it take to return to normal activities after a back fracture?
The time to return to normal activities varies. It depends on the fracture’s severity and individual factors. A gradual return to daily activities is recommended.
Are there any long-term implications after a back fracture?
Yes, back fractures can have long-term effects. They may require permanent lifestyle changes and ongoing management of symptoms.
What is the long-term prognosis after a back fracture?
The long-term prognosis varies. It depends on the fracture’s severity, treatment, and individual health. With proper care, many people can recover well.
How can secondary complications be prevented during recovery?
To prevent secondary complications, early mobilization and proper pain management are key. Following a rehabilitation program tailored to individual needs is also important.
References
Bicket, M. C., et al. (2013). Epidural injections for spinal pain: A systematic review and meta-analysis. Pain Physician, 16(5), E453-E470. https://pubmed.ncbi.nlm.nih.gov/24195874/