Last Updated on November 26, 2025 by Bilal Hasdemir

We are looking into irreversible electroporation (IRE), also called IRE ablation. It’s a new way to treat different cancers. This method uses electrical pulses to damage cell membranes, leading to cell death.
Learning about irreversible electroporation helps us see its role in fighting cancer. It’s great because it doesn’t harm important parts like blood vessels and nerves. This makes it a good choice for treating tumors in hard-to-reach places.
Key Takeaways
- IRE ablation is a non-thermal tissue ablation technique.
- It uses short, high-voltage electrical pulses to create nanopores in cell membranes.
- This results in targeted cell death while preserving critical structures.
- IRE is specially good for treating tumors in sensitive areas.
- It offers a promising treatment option for various types of cancer.
Understanding IRE Ablation: The Fundamentals
IRE ablation, also known as irreversible electroporation, is a new way to treat cancer. It’s a non-thermal method that’s getting a lot of attention. It’s seen as a less invasive option compared to traditional surgery.
Definition and Basic Principles
IRE ablation uses high-voltage electrical pulses to damage cancer cells. It creates tiny holes in their membranes, causing them to die. This method is different because it doesn’t use heat or cold like other treatments do.
The treatment is guided by imaging, making it precise. This helps avoid harming healthy tissue. Because of this, IRE can be done on an outpatient basis. This means patients don’t have to stay in the hospital as long, and they face fewer side effects.
Historical Development of Irreversible Electroporation
IRE was first used in patients in 2008. It was used to treat certain cancers. One area where it’s been used a lot is in Stage III pancreatic cancer. This is a tough condition to treat.
Studies have shown IRE is safe and effective. They’ve seen good results in patient survival. As more research is done, IRE might help even more people with tough diagnoses.
The Science Behind Irreversible Electroporation

Understanding IRE is key to seeing its promise in fighting complex cancers. It works by using high-voltage electrical pulses to kill tumor cells.
Cell Membrane Nanopores: The Mechanism of Action
IRE works by making tiny holes in cell membranes, causing cells to die. This happens without harming the tissue around them. High-voltage electrical pulses create these holes, disrupting the cell’s balance.
Nanopore formation is vital in IRE. These holes let ions and molecules flood in, causing the cell to die naturally. This is called apoptosis.
Differentiating IRE from Thermal Ablation Techniques
IRE is different from heat-based treatments that kill cancer cells. Heat can harm nearby tissues. But IRE is a non-thermal method that keeps tissues like blood vessels and nerves safe.
| Characteristics | IRE Ablation | Thermal Ablation |
| Mechanism of Action | Creates nanopores in cell membranes | Uses heat to destroy cancer cells |
| Effect on Surrounding Tissue | Preserves surrounding tissue structures | Can damage surrounding tissues due to heat |
| Applicability | Ideal for tumors in delicate anatomical areas | May not be suitable for tumors near critical structures |
IRE’s precision is why it’s so valuable in cancer treatment. It’s perfect for areas where keeping tissue safe is essential. As we learn more about IRE, its advantages over traditional methods become clearer.
How IRE Ablation Works in Clinical Practice
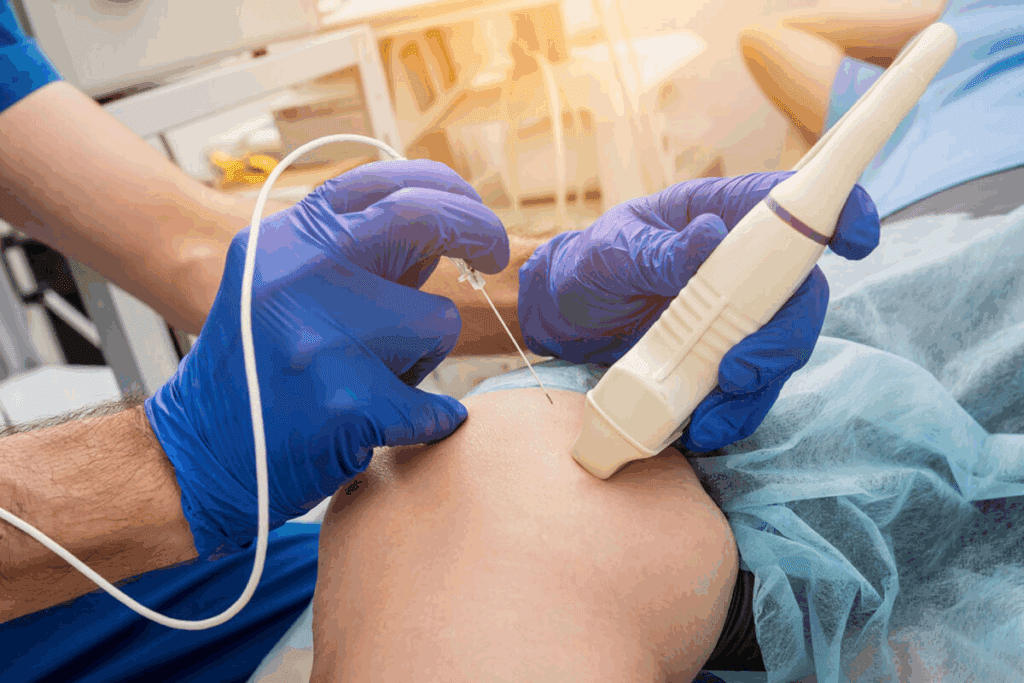
The IRE procedure is done under imaging guidance. This lets doctors precisely target tumors with needle electrodes. This precision is key for the treatment’s success.
The IRE Procedure Step-by-Step
We start by placing needle electrodes around the tumor. This is done under imaging like ultrasound or CT scans. Then, these electrodes are connected to a high-voltage generator.
The generator sends electrical pulses. These pulses make nanopores in cancer cells’ membranes, causing them to die.
The process is both precise and effective. Key steps include:
- Preparation of the patient, including positioning and sedation
- Insertion of needle electrodes around the tumor under imaging guidance
- Delivery of high-voltage pulses through the electrodes
- Monitoring of the procedure in real-time to ensure accuracy
Equipment and Technology Used in IRE
The technology for IRE includes special electrodes and generators. NanoKnife is one technology developed for IRE procedures.
We use advanced imaging to guide electrode placement and monitor the procedure. This ensures the treatment is accurate and safe for healthy tissues.
Applications of IRE Ablation in Oncology
IRE ablation is changing how we treat cancer. It brings new hope to patients with different types of cancer. This method is making a big difference, mainly for cancers in hard-to-reach places.
One big plus of IRE ablation is it helps keep the healthy tissue around tumors safe. This is great for cancers like prostate, liver, and pancreatic cancers. It’s a big advantage because these areas are very sensitive.
Prostate Cancer Treatment with IRE
For prostate cancer, IRE ablation is a less invasive option. It might help keep urinary and sexual functions intact. Early studies show it’s effective and has fewer side effects than older treatments.
IRE’s precision is key. It targets cancer cells while protecting the healthy tissue. This is important for keeping patients’ quality of life high.
Liver Cancer Applications
IRE ablation is also great for liver cancer. It’s perfect for tumors near major blood vessels or other important structures. Traditional methods might harm these areas, but IRE is safer.
Pancreatic Cancer and IRE
Pancreatic cancer is another area where IRE ablation is promising. It’s a good option for locally advanced pancreatic cancer. IRE can target tumors without harming the surrounding pancreatic tissue.
As research grows, IRE ablation’s role in cancer treatment will likely expand. We’re dedicated to keeping up with these advancements. This way, we can offer our patients the best and latest treatments.
Advantages of IRE Ablation Over Traditional Treatments
Irreversible electroporation (IRE) ablation has many benefits over traditional cancer treatments. It works differently, not using heat. This means it can keep important areas around the tumor safe, lowering the chance of problems and better results for patients.
Preservation of Critical Structures
IRE ablation is great because it keeps vital structures like blood vessels and nerves safe. It doesn’t harm these areas like heat treatments do. This makes it perfect for tumors close to important parts of the body.
For example, in treating prostate cancer, IRE helps keep the urethral sphincter and nerves safe. This could lower the risk of problems like not being able to control urine or having trouble with erections.
Reduced Recovery Time and Hospital Stays
IRE ablation means patients get better faster and don’t have to stay in the hospital as long. It’s a less invasive method that causes less damage and pain.
| Treatment | Average Recovery Time | Average Hospital Stay |
| IRE Ablation | 1-3 days | 1-2 days |
| Traditional Surgery | 1-2 weeks | 3-5 days |
With IRE ablation, patients can get back to their lives sooner. It’s a more convenient and less stressful option for them.
In summary, IRE ablation is great because it keeps important areas safe and helps patients recover faster. It’s a valuable choice for treating many types of cancer.
Patient Selection and Preparation for IRE Treatment
Choosing the right patients for IRE treatment is key to success. We focus on picking the best candidates to get the most from IRE while keeping risks low. This means looking at the patient’s health, the tumor’s details, and the patient’s overall condition.
Ideal Candidates for IRE Ablation
The best candidates for IRE have tumors in sensitive areas. For example, those with prostate, liver, or pancreatic cancer might benefit. We check each case carefully, looking at the tumor’s size, where it is, and the patient’s health history.
Pre-Procedure Protocols and Requirements
Before IRE treatment, patients go through detailed checks. We use MRI or CT scans to see the tumor’s size and where it is. We also look at the patient’s health and any past treatments to make the procedure fit their needs.
By carefully choosing and preparing patients for IRE, we make the treatment safer and more effective. Our team works with patients to give them care that’s just right for them.
Clinical Outcomes and Efficacy of IRE Ablation
Recent studies have shown IRE ablation is effective against various cancers. It’s important to look at both short-term and long-term results.
Short-Term Results and Success Rates
Studies have found IRE to be effective in treating several cancers. For example, in prostate cancer, less than 10% of patients have experienced recurrence after IRE treatment. This shows IRE could be a good treatment option.
The success of IRE is due to its precision in targeting cancer cells. It does this while keeping important structures safe.
IRE works by creating nanopores in cell membranes, causing cell death. This method is effective for tumors near vital structures, where other treatments might be risky.
Long-Term Efficacy and Ongoing Research
The short-term results are promising, but we need more on long-term effects. Research is ongoing to see how long IRE’s benefits last. Early signs suggest IRE can control tumors for a long time, improving patient outcomes.
As more research comes in, we’ll understand IRE’s full role in cancer treatment. These studies are key to confirming its long-term benefits and any limitations.
In summary, IRE ablation shows promise in both short-term and long-term results. As research continues, we expect to learn more about its place in cancer treatment.
Potential Side Effects and Complications
It’s important for patients to know about the side effects and complications of IRE ablation. This treatment has shown great promise in fighting cancer. But, it’s key to understand the risks involved.
Common Side Effects After IRE Treatment
People who get IRE ablation might feel pain, nausea, and inflammation. This is more common if the pancreas is treated. We make sure patients know about these side effects to help them prepare and recover better.
Effective management of these side effects is key. It helps patients live better lives. The medical team and patient education play big roles in this.
Managing and Minimizing Complications
We use several ways to manage and reduce complications. These include careful patient selection, precise technique during the procedure, and detailed post-procedure care. These steps help lower the risk of problems and speed up recovery.
| Complication | Management Strategy | Outcome |
| Pain | Effective pain management protocols | Reduced discomfort |
| Nausea | Antiemetic medication | Improved patient comfort |
| Pancreatitis | Close monitoring and supportive care | Minimized risk of severe pancreatitis |
By knowing about the side effects and complications of IRE ablation, we can improve patient results and life quality. Effective management strategies are key to this.
Conclusion: The Future of IRE Ablation in Cancer Treatment
IRE ablation is a big step forward in cancer treatment. It’s a non-thermal, minimally invasive method that keeps important structures safe. This makes it a great choice for patients with complex tumors.
Research and clinical trials are showing great promise for IRE ablation. They are proving it’s safe and effective. This could lead to better treatment options and improved lives for patients.
As doctors learn more about IRE ablation, it will become a more common treatment. Its unique benefits make it a powerful tool in the fight against cancer. We can look forward to seeing its impact grow.
FAQ
What is IRE ablation?
IRE ablation, or irreversible electroporation, is a way to kill cancer cells without heat. It uses electrical pulses to make holes in cell membranes. This leads to the death of targeted cells.
How does IRE differ from thermal ablation techniques?
IRE doesn’t use heat to kill cancer cells. This is different from other methods. It helps keep the surrounding tissues, like blood vessels and nerves, intact.
What are the applications of IRE ablation in oncology?
IRE ablation is used to treat different cancers, like prostate, liver, and pancreatic cancers. It’s a minimally invasive option that helps preserve important structures.
What are the advantages of IRE ablation?
IRE ablation has many benefits. It helps keep important structures safe, reduces recovery time, and shortens hospital stays. This makes it a more convenient choice for patients.
Who are ideal candidates for IRE ablation?
The best candidates for IRE ablation have tumors in areas where keeping tissue safe is key. They go through tests, like imaging studies, to see if they’re a good fit.
What are the common side effects of IRE ablation?
Side effects of IRE ablation include pain, nausea, and swelling. It’s important to manage these side effects well to improve patients’ quality of life.
What is the historical development of IRE?
IRE was first used in patients in 2008 for treating certain cancers. It has grown in use, with a big increase in treating locally advanced pancreatic cancer.
How is IRE ablation performed?
IRE ablation is done with great care using advanced imaging. Needles are placed around the tumor and connected to a high-voltage generator. Then, electrical pulses are delivered.
What are the short-term results of IRE ablation?
Early studies show promising results, with less than 10% of patients seeing cancer come back after treatment for prostate cancer. But, more research is needed to understand long-term effects.
Is IRE ablation a safe procedure?
IRE ablation is usually safe, but it can have side effects and complications. Choosing the right patients, using precise techniques, and good care after the procedure help reduce risks.
References
Shrestha, O., Basukala, S., Thapa, N., et al. (2023). Endovenous laser ablation versus conventional surgery (ligation and stripping) for primary great saphenous varicose vein: A systematic review and meta-analysis. Annals of Medicine and Surgery, 85, 4509-4519. https://pubmed.ncbi.nlm.nih.gov/37663729/