Last Updated on November 26, 2025 by Bilal Hasdemir

At Liv Hospital, we focus on patient care and new ideas. We use interventional radiology to help people avoid open surgery. Interventional Radiology (IR) is a new way to treat many health issues without big surgery.
We use imaging technology for quick and safe procedures. This means patients can get better faster and stay in the hospital less. Thanks to imaging guidance, we can find and fix problems more accurately and safely. Many patients ask, “what is interventional?” This new field is changing how we treat and diagnose diseases.
Key Takeaways
- Interventional Radiology (IR) is a minimally invasive alternative to traditional surgery.
- IR uses imaging technologies for diagnosis and treatment.
- Faster recovery and reduced hospital stays are significant benefits of IR.
- IR offers a range of solutions for various medical conditions.
- Imaging guidance enables precise and less risky procedures.
Understanding Interventional Radiology: Definition and Core Concepts
Interventional radiology uses images to guide minimally invasive treatments. It’s a key part of modern healthcare, providing safer options than old surgeries.
The Official Interventional Radiology Definition
Interventional radiology means using images to do treatments and tests. It shows how IR relies on new imaging tech for its work.
We use tools like ultrasound and CT scans to see inside the body. This helps us do precise treatments with less harm.
Historical Development of IR as a Medical Specialty
IR’s history is one of growth and new ideas. It started in the 1960s and has changed a lot.
| Year | Milestone |
| 1960s | Introduction of angiography, marking the beginning of IR |
| 1970s-80s | Advancements in catheter technology and embolization techniques |
| 1990s-present | Integration of advanced imaging modalities like MRI and CT scans into IR practice |
The Minimally Invasive Philosophy of IR
IR focuses on small, less hurtful treatments. These methods cause less pain and quicker healing than big surgeries.
Key benefits of IR’s minimally invasive approach include:
- Smaller incisions, often just a needle puncture or small nick in the skin
- Reduced risk of infection and other complications
- Less post-procedure pain
- Shorter hospital stays and quicker recovery times
IR’s focus on small treatments opens new ways to help patients. It leads to better care and a better life for many.
The Technology Behind IR: Imaging Modalities Used
Interventional radiology uses advanced imaging to guide procedures. These tools help doctors see inside the body in real-time. This ensures treatments are precise and effective.
Ultrasound and CT Scanning in IR Procedures
Ultrasound and CT scanning are key in IR. Ultrasound technology uses sound waves to create images. It helps guide needles and catheters during procedures.
CT scanning gives detailed images of the body. This helps doctors plan and do complex procedures. CT-guided interventions are used for biopsies and tumor treatments.
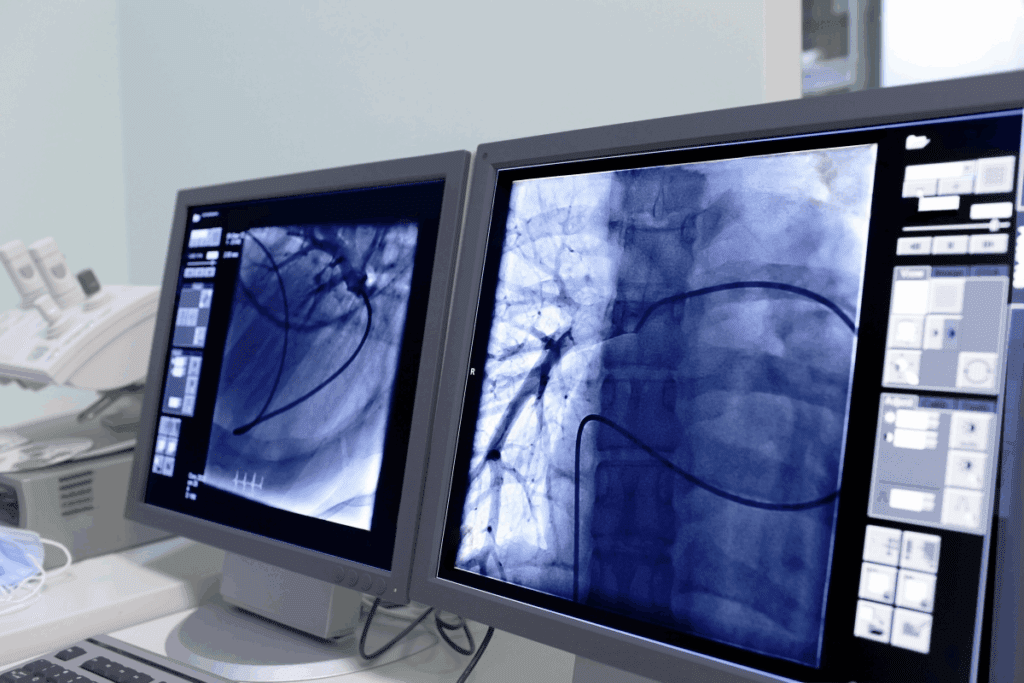
Fluoroscopy and MRI Applications
Fluoroscopy offers real-time X-ray images. It’s used in vascular interventions like angioplasty. It helps doctors see moving body structures.
MRI gives detailed images of soft tissues. It’s great for procedures involving the liver and kidneys. MRI-guided interventions are becoming more common.
Advanced Imaging Technologies in Modern IR Practice
New imaging technologies have improved IR. Fusion imaging combines data from CT, MRI, and ultrasound. This makes procedures more precise.
| Imaging Modality | Key Features | Common IR Applications |
| Ultrasound | Real-time imaging, portable, no ionizing radiation | Vascular access, biopsies, drainage procedures |
| CT Scanning | High-resolution images, detailed cross-sectional views | Biopsies, tumor treatments, drainage procedures |
| Fluoroscopy | Real-time X-ray imaging, dynamic visualization | Vascular interventions, angioplasty, stenting |
| MRI | High-resolution soft tissue imaging, no ionizing radiation | Liver, kidney, and other organ interventions |
These imaging modalities are getting better. This will help IR do more complex procedures safely. It’s good news for patients.
What Is Interventional Radiology in Practice: Common Procedures
Interventional radiology (IR) has changed medical care by introducing new, less invasive treatments. These treatments help treat many health issues. They are key to modern healthcare, leading to better results and faster healing.
Vascular Interventions: Angioplasty and Stenting
Vascular interventions are a big part of IR, focusing on blood vessel diseases. Angioplasty and stenting are two main treatments. Angioplasty uses a balloon to widen narrowed arteries. Stenting places a metal tube to keep arteries open.
These methods help with diseases like PAD and CAD. They greatly improve patient outcomes by easing symptoms and preventing serious heart problems.
Oncological Procedures: Tumor Ablation and Embolization
IR is also key in cancer treatment. Tumor ablation uses heat or cold to kill cancer cells. Tumor embolization blocks the tumor’s blood supply, starving it.
These methods can be used alone or with other treatments like chemo or surgery. They offer a less invasive option for those not suited for traditional surgery.
| Procedure | Description | Benefits |
| Tumor Ablation | Destroys cancer cells using heat or cold | Minimally invasive, preserves organ function |
| Tumor Embolization | Cuts off blood supply to the tumor | Reduces tumor size, alleviates symptoms |
Urological and Biliary Interventions
IR also treats urological and biliary issues. For example, percutaneous nephrostomy drains urine from the kidney. Biliary drainage drains bile from the liver, helping with blockages.
These treatments help patients with urinary or biliary problems. They improve life quality and lower the risk of complications.
Drainage Procedures and Biopsies
IR specialists also do drainage and biopsy procedures. Abscess drainage removes infected fluid. Biopsies take tissue samples for diagnosis.
These are critical for diagnosing and treating many conditions, from infections to cancers. They are done under imaging, ensuring they are accurate and safe.
The Interventional Radiologist: Training and Expertise
Interventional radiologists are highly skilled medical professionals. They have specialized training. They play a key role in diagnosing and treating various medical conditions using minimally invasive procedures.
Educational Requirements for Interventional Radiologists
To become an interventional radiologist, one must go through a lot of education and training. This includes finishing medical school, then a residency in radiology. Often, they also do fellowship training in interventional radiology.
The path to becoming an interventional radiologist is tough and demanding. It needs a strong base in medicine and a deep understanding of radiology.
Specialized Skills and Certifications
Interventional radiologists need specialized skills. They must be good at using imaging technologies like ultrasound, CT, and fluoroscopy. They also need to get certifications, such as board certification in radiology, to show their expertise.
Certifications are key. They make sure interventional radiologists meet high standards. They pass tough exams and keep learning to stay up-to-date with new field advancements.
The Multidisciplinary Approach in IR Teams
Interventional radiology teams work together in a multidisciplinary environment. They team up with other healthcare professionals to give patients the best care. This teamwork ensures patients get the best treatment outcomes.
By working with specialists from different fields, interventional radiologists can offer a more complete approach to patient care. They combine their skills with others to get the best results for patients.
IR vs. Traditional Surgery: Key Differences
It’s important to know the differences between IR and traditional surgery. IR has many benefits over traditional surgery.
Incision Size and Invasiveness Comparison
IR and traditional surgery differ in incision size and invasiveness. IR uses minimally invasive methods, often with tiny incisions or needle punctures. Traditional surgery needs larger incisions for direct access.
IR’s smaller incisions cause less damage and trauma. This leads to less pain and faster healing for patients. It’s great for those at high risk for complications from big surgeries.
Anesthesia Requirements and Options
IR and traditional surgery also differ in anesthesia. IR uses local anesthesia or conscious sedation. Traditional surgery often needs general anesthesia, making the patient unconscious.
Using local anesthesia or conscious sedation in IR is safer. It’s better for patients with health conditions or at risk for anesthesia complications.
Recovery Time and Hospital Stay Duration
Recovery time is another big difference. IR procedures have faster recovery times and shorter hospital stays. Many IR procedures are done on an outpatient basis, so patients go home the same day.
Traditional surgery requires longer hospital stays for recovery. It also means longer post-operative pain and discomfort.
Risk Profiles and Complication Rates
IR and traditional surgery have different risk profiles and complication rates. IR has lower complication rates due to its minimally invasive nature and avoiding general anesthesia. Risks like infection, bleeding, and anesthesia reactions are lower in IR.
But, IR is not risk-free. Patients should talk to their healthcare provider about the risks and benefits of IR procedures. This helps make informed decisions about their care.
Benefits of Choosing IR Over Conventional Surgery
Choosing IR over traditional surgery can lead to better results, quicker recovery, and fewer complications. We will look at the benefits that make IR a good choice for many patients.
Reduced Pain and Complications
One big benefit of IR is less pain and complications. IR is minimally invasive, causing less damage and trauma than open surgery.
- Smaller incisions mean less pain and scarring.
- Lower risk of infection because of less tissue exposure.
- Fewer complications from anesthesia and surgical trauma.
Faster Recovery and Return to Normal Activities
Patients who have IR procedures usually recover faster. This is because IR is less invasive, disrupting the body less.
The benefits include:
- Shorter hospital stays or even outpatient procedures.
- Quicker return to daily activities and work.
- Less need for post-procedure pain management.
Cost-Effectiveness and Healthcare Economics
IR procedures are often more cost-effective than traditional surgery. They require less hospital resources, have shorter recovery times, and fewer complications, all leading to lower healthcare costs.
Key economic benefits include:
- Reduced hospital stay costs.
- Lower costs associated with managing complications.
- Fewer resources required for post-procedure care.
Accessibility for High-Risk Patients
IR is a vital option for high-risk patients who may not be good candidates for traditional surgery. This is due to underlying health conditions or other factors.
The advantages for high-risk patients include:
- Ability to undergo necessary treatments with fewer risks.
- Alternative to surgery for patients with significant comorbidities.
- Potential for improved outcomes in a patient population that is often more challenging to treat.
Clinical Applications: When Is IR the Preferred Option?
We use IR for many clinical needs, making treatment safer and faster. It’s a key part of modern medicine, a gentler way to treat many conditions instead of surgery.
Cardiovascular Conditions Treated with IR
IR is key in fighting heart diseases. It does angioplasty and stenting to clear blocked arteries. This helps prevent heart attacks and strokes.
It also uses embolization to treat diseases like peripheral artery disease.
Cancer Diagnosis and Treatment Approaches
In cancer care, IR helps in both finding and treating cancer. It does biopsies to diagnose cancer. Then, it uses tumor ablation and chemoembolization to kill cancer cells without harming nearby healthy tissue.
Management of Kidney Stones and Renal Conditions
IR is great for kidney stone and renal issues. It uses ureteroscopy and percutaneous nephrolithotomy to treat stones. These methods are less invasive than open surgery.
Gastrointestinal and Hepatobiliary Applications
IR is also used for the gut and liver. It does biliary drainage and transjugular intrahepatic portosystemic shunt (TIPS). These help with liver disease and bile duct problems.
Knowing how IR works helps doctors give patients the best treatments. This improves health and life quality.
Patient Experience: What to Expect During an IR Procedure
The journey through an Interventional Radiology (IR) procedure is complex. It starts long before the actual procedure. Understanding the stages from preparation to recovery is key.
Pre-Procedure Preparation and Consultation
Patients first meet with their interventional radiologist for a detailed consultation. This is where they discuss their medical history and the procedure’s details. We also talk about the benefits of IR over traditional surgery.
Before the procedure, patients may need to:
- Stop certain medications
- Undergo lab tests
- Follow dietary restrictions
During the Intervention: Procedure Environment
Patients are placed in a sterile environment for the procedure. The team, including the radiologist, watches over the patient. This ensures safety and success.
The procedure uses advanced imaging like fluoroscopy or ultrasound. We aim to keep patients comfortable, using local anesthesia and sedation if needed.
Post-Procedure Care and Follow-up Protocols
After the procedure, patients are in a recovery area. Here, they are monitored for any immediate issues. We provide instructions for recovery, including rest and follow-up appointments.
Good post-procedure care is vital for a smooth recovery. Our team is ready to answer any questions or concerns.
Patient Selection and Candidacy Factors
Not every patient is a good fit for IR procedures. The decision depends on health, condition, and past treatments.
We evaluate each patient individually. We consider factors like condition severity, past surgeries, and comorbidities.
By choosing the right candidates and tailoring our approach, we ensure the best outcomes. This approach minimizes risks.
The Future of Interventional Radiology: Emerging Trends
Interventional Radiology (IR) is set to change medical practice with new trends and tech. The field is growing fast, thanks to new ideas that help patients more and make treatments better. These changes will make treatments less invasive and more efficient.
Advancements in Technology
New tech is leading the way in IR’s future. Improvements in imaging like better ultrasound and advanced CT and MRI machines help doctors do their jobs better. Also, image-guided therapy gets more precise and effective.
New devices and tools are also key. For example, better catheters, guidewires, and stents help doctors do more. These advancements mean better results and less time recovering.
Artificial Intelligence and Machine Learning in IR
Artificial Intelligence (AI) and Machine Learning (ML) are changing IR. They help analyze images better, leading to more accurate diagnoses and plans. AI spots things in images that humans might miss, helping patients more.
AI and ML are also being used to guide procedures and predict outcomes. They look at big data to find the best treatments for each patient. This makes care more personalized and effective.
Expanding Applications in Previously Surgical Domains
IR is moving into areas once only surgery could reach. This includes treating cancers, vascular diseases, and more. IR’s minimally invasive methods mean patients recover faster and face fewer risks.
As IR grows, it will play a bigger role in managing complex conditions. This will lead to better care and more efficient healthcare.
Integration with Other Medical Specialties
IR is working more with other specialties than ever before. Doctors from different fields are teaming up to care for patients. This teamwork leads to better treatment plans and outcomes.
As IR keeps evolving, we’ll see even more teamwork. This integration is key to IR’s growing role in medicine today.
Conclusion: The Growing Importance of IR in Modern Medicine
Interventional Radiology (IR) is key in today’s medicine. It offers non-invasive treatments that improve patient care and life quality. IR’s role is growing, helping treat many health issues.
IR’s approach, using advanced imaging, appeals to those looking for surgery alternatives. It brings benefits like less pain, quicker healing, and lower costs. These changes are reshaping how we tackle medical problems.
The future of IR is bright, with new trends and tech on the way. As IR evolves, we’ll see more creative treatments and better patient care. In short, IR’s role in modern medicine is vital and will shape healthcare’s future.
FAQ
What is Interventional Radiology (IR)?
Interventional Radiology is a medical field. It uses imaging to do small, precise procedures. These help diagnose and treat diseases.
How does IR differ from traditional surgery?
IR is different because it’s less invasive. It uses small cuts and imaging to guide the procedure. This means patients recover faster and stay in the hospital less.
What imaging modalities are used in IR?
IR uses several imaging tools. These include ultrasound, CT scans, fluoroscopy, and MRI. They help doctors see exactly where they’re working.
What kind of procedures are performed in IR?
IR does many procedures. These include vascular treatments, cancer treatments, and procedures for the kidneys and liver. They also do biopsies and drain fluids.
What training is required to become an interventional radiologist?
To be an IR doctor, you need a lot of education and training. This includes learning special skills and getting certifications.
What are the benefits of choosing IR over conventional surgery?
Choosing IR has many advantages. It can reduce pain and complications. Patients recover faster and it’s often cheaper. It’s also good for people who can’t have traditional surgery.
When is IR the preferred option for treatment?
IR is often the best choice for many conditions. This includes heart diseases, cancer, kidney stones, and problems with the liver and digestive system.
What can patients expect during an IR procedure?
Patients get ready for the procedure by following certain steps. The procedure is done in a clean, monitored area. Afterward, they get care and follow-up instructions.
What is the future of IR?
The future of IR looks bright. New technologies and trends are emerging. IR is also being used in more areas and working with other medical fields.
Is IR a cost-effective treatment option?
Yes, IR can save money. It reduces the time patients spend in the hospital and speeds up recovery. This can lower healthcare costs.
Can IR be used for high-risk patients?
Yes, IR is a good option for high-risk patients. It’s safer than traditional surgery for them.