Last Updated on November 26, 2025 by Bilal Hasdemir
Chronic pain affects millions worldwide, and for many, medication and therapy alone may not provide enough relief. In these cases, advanced chronic pain medical procedures are often required.
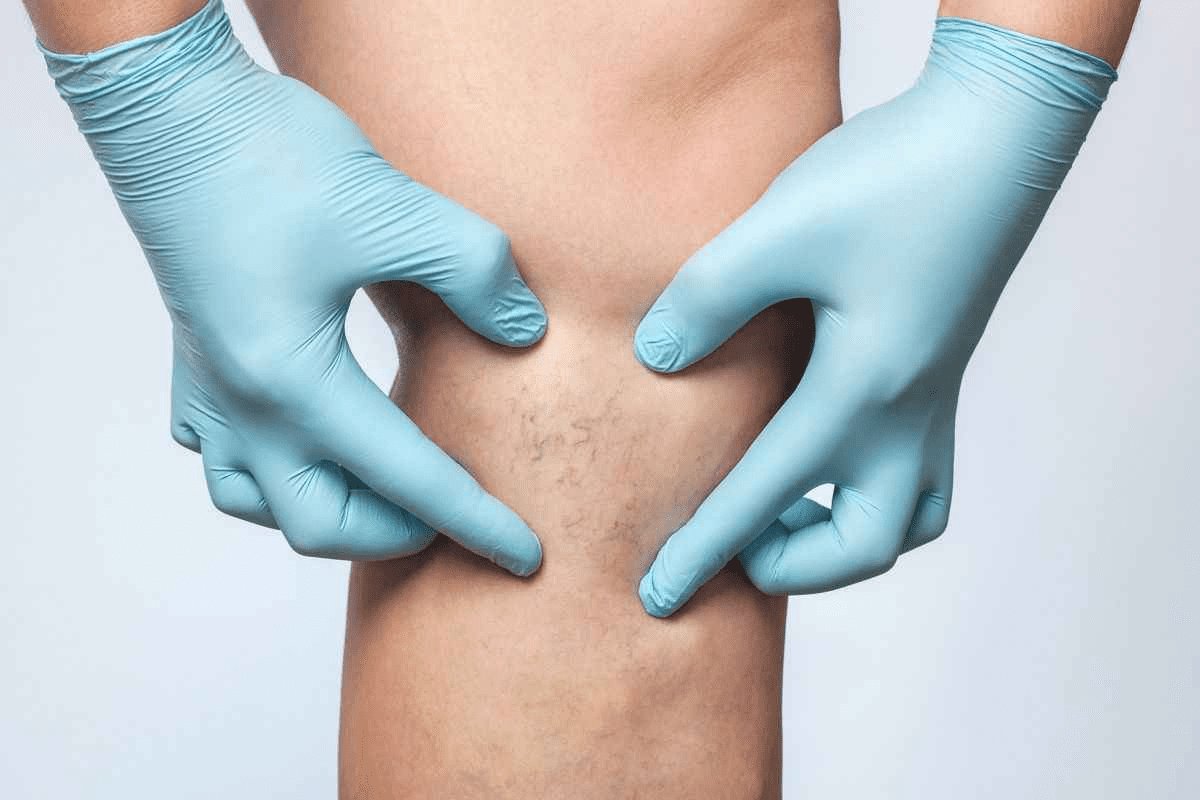
Invasive procedures in medicine involve inserting or penetrating the body through incisions or injections. These procedures are essential for diagnosing and treating various health conditions, including chronic pain. A vascular radiologist plays a critical role in these treatments, using advanced imaging techniques to guide minimally invasive procedures safely and accurately.
At leading pain clinics like Liv Hospital, our team of experts, including skilled vascular radiologists, offers targeted, interventional pain procedures. These minimally invasive treatments provide fast, effective relief while minimizing recovery time. The expertise of a vascular radiologist ensures that each procedure is precise, safe, and optimized for the best possible outcome.
Key Takeaways
- Chronic pain affects millions worldwide, requiring effective treatment options.
- Invasive procedures are medical interventions that penetrate the body.
- These procedures are key for diagnosing and treating chronic pain.
- Liv Hospital offers advanced interventional pain procedures for rapid relief.
- Minimally invasive options reduce downtime and promote recovery.
Defining Invasive Procedures in Modern Medicine

In modern medicine, invasive procedures vary from small to big. They range from tiny cuts to open surgeries. These methods are key for diagnosing and treating health issues, like chronic pain.
Medical Definition and Classification Criteria
Invasive procedures involve going into the body, either through the skin or other surfaces. They aim to diagnose or treat health problems. The level of invasiveness, technology used, and the condition treated determine their type.
There are different types of invasive procedures:
- Diagnostic procedures, such as biopsies or exploratory surgeries
- Therapeutic procedures, like interventional pain procedures aimed at relieving chronic pain
- Surgical interventions, ranging from minimally invasive surgeries to complex open surgeries
| Procedure Type | Description | Examples |
| Minimally Invasive | Procedures that involve small incisions or insertions | Laparoscopic surgery, arthroscopic procedures |
| Moderately Invasive | Procedures that require larger incisions or more significant intrusion | Some orthopedic surgeries, certain types of tumor removals |
| Fully Invasive | Major surgeries that involve significant incisions and tissue disruption | Open-heart surgery, complex spinal surgeries |
The Purpose Behind Invasive Medical Interventions
Invasive medical interventions are used when other treatments don’t work. They help treat health issues that need direct action. For example, interventional pain procedures target pain sources directly.
Key benefits of invasive procedures include:
- Precise diagnosis and treatment of complex medical conditions
- Effective pain management through interventional pain procedures
- Minimally invasive options that reduce recovery time and minimize scarring
Understanding invasive procedures helps us see their importance in healthcare. They can greatly improve patient outcomes.
The Spectrum of Invasive Operations: From Minimally Invasive to Open Surgery

Surgical operations range from small, minimally invasive techniques to open surgery. The choice depends on the patient’s condition and the nature of the ailment. It also considers the risks and benefits of each surgery type.
Knowing about invasive operations is key for patients and doctors. It helps in making informed decisions and setting realistic recovery expectations.
Minimally Invasive Techniques
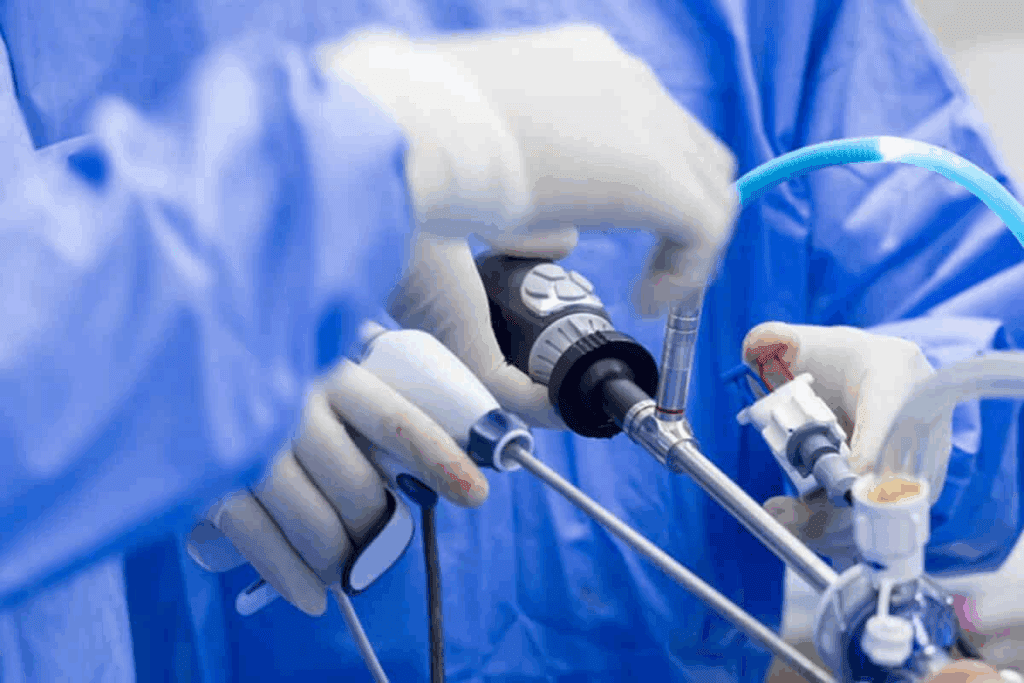
Minimally invasive surgery has changed the field, bringing many benefits. These surgeries use small incisions, causing less damage and pain. They also lead to quicker recovery times. Laparoscopic and arthroscopic surgeries are examples, used for pain relief.
Benefits of Minimally Invasive Techniques:
- Smaller scars
- Less postoperative pain
- Shorter hospital stays
- Faster return to normal activities
These pain procedures, like injections and ablations, are popular. They offer effective relief with little downtime.
Moderately Invasive Procedures
Moderately invasive procedures are a middle ground. They use slightly larger incisions than minimally invasive surgeries. Yet, they offer quicker recovery times and less pain compared to open surgery.
Examples include some spinal and orthopedic surgeries. These are used when less invasive methods are not enough.
Fully Invasive Surgical Operations
Fully invasive surgeries, or open surgeries, require larger incisions. They are more invasive and have longer recovery times. Yet, they are needed for complex conditions not treatable by less invasive means.
Open surgery is used for major operations like cardiovascular and neurosurgeries. Advances in surgery and care have improved outcomes for these patients.
| Type of Surgery | Incision Size | Recovery Time | Postoperative Pain |
| Minimally Invasive | Small | Short | Less |
| Moderately Invasive | Moderate | Moderate | Moderate |
| Fully Invasive | Large | Long | More |
Understanding the differences between these surgeries is vital. It helps in making informed decisions about care. Patients and doctors can then choose the best treatment plan together.
Chronic Pain: A Global Health Challenge
Millions of people worldwide live with chronic pain. This condition deeply affects their lives. It impacts both their physical and emotional health.
The Prevalence and Impact of Chronic Pain
Chronic pain is a big problem globally. It can come from injuries, infections, or ongoing conditions like arthritis. It affects not just health but also work and daily life.
The economic burden of chronic pain is huge. It includes healthcare costs, lost productivity, and reduced quality of life. Chronic pain costs the world billions every year.
Limitations of Conservative Treatment Approaches
First steps in treating chronic pain include medication and physical therapy. But, these methods have their limits. Some patients may not get enough relief, and others face side effects.
These treatments might not fix the pain’s cause. This can lead to a cycle of needing more medication. Pain clinic procedures offer a more focused way to manage chronic pain.
Knowing the limits of traditional treatments helps us find new solutions. Pain clinic procedures are a big step forward. They offer hope to those who haven’t found relief yet.
Interventional Pain Management: A Targeted Approach
Interventional pain management is key in fighting chronic pain. It uses small procedures to give relief. This field has grown a lot, helping those who didn’t get better with usual treatments.
What Is an Interventional Pain Specialist?
An interventional pain specialist is a doctor who treats chronic pain with small procedures. They learn a lot about injections and devices to help patients. They aim to give specific relief for different pain types.
These specialists work with patients to make plans that fit their needs. They use their knowledge to improve patients’ lives a lot.
The Evolution of Interventional Pain Medicine
Interventional pain medicine has grown a lot over time. New tech and understanding pain better have helped it grow. Now, it includes many procedures for different pains.
New methods and better old ones are being developed. This is important for safer and more effective treatments for patients.
The table below shows important moments in interventional pain management’s growth:
| Year | Milestone | Description |
| 1980s | Introduction of Epidural Steroid Injections | Started interventional pain management as a field. |
| 1990s | Advancements in Nerve Blocks | Improved ways to target pain relief. |
| 2000s | Spinal Cord Stimulation | Was first used for neuropathic pain. |
Knowing the history of interventional pain management shows how advanced pain relief is today.
Common Interventional Pain Procedures and Their Applications
Interventional pain procedures are key in managing chronic pain that doesn’t get better with usual treatments. They aim to help those with long-term pain, like back pain and arthritis.
Epidural Steroid Injections for Spinal Pain
Epidural steroid injections are a common treatment for spinal pain due to inflammation. They put steroids near the spinal cord to cut down inflammation and ease pain. This method works well for people with herniated discs, spinal stenosis, or spondylolisthesis.
These injections can greatly reduce pain and improve function. They might even help avoid surgery. But, like any procedure, they can have risks like infection, bleeding, and nerve damage.
Nerve Blocks for Targeted Pain Relief
Nerve blocks inject a local anesthetic or steroid into a nerve to block pain signals. This method is great for diagnosing and treating chronic pain, like complex regional pain syndrome and neuropathic pain.
Nerve blocks can give quick pain relief. They can be used over and over to manage long-term pain. While generally safe, there’s a chance of nerve damage, infection, or allergic reactions.
Radiofrequency Ablation for Long-Term Results
Radiofrequency ablation (RFA) uses radio waves to heat up and destroy nerve endings. This stops pain signals. RFA is often used for chronic pain from arthritis, facet joint syndrome, and sacroiliac joint dysfunction.
RFA offers long-lasting pain relief and less need for pain meds. It also has a quick recovery time. But, it can have risks like infection, bleeding, and temporary discomfort at the site.
Joint Injections for Arthritic Conditions
Joint injections put corticosteroids or hyaluronic acid into the joint to reduce inflammation and pain. They’re used for conditions like osteoarthritis, rheumatoid arthritis, and gout.
Joint injections can greatly reduce pain and improve joint function. While safe, there’s a chance of infection, temporary pain increase, and allergic reactions to the substances.
Advanced Interventional Techniques for Complex Pain Conditions
For those with complex pain, new hope comes in the form of advanced interventional techniques. These treatments aim to help those who haven’t found relief with traditional pain management.
Spinal Cord Stimulation for Neuropathic Pain
Spinal cord stimulation (SCS) is a top choice for neuropathic pain that’s tough to treat. It involves a device that sends electrical impulses to the spinal cord. This stops pain signals from reaching the brain.
Many patients with chronic neuropathic pain have seen big improvements with SCS. The procedure is done under local anesthesia. Afterward, the device is fine-tuned to maximize pain relief.
Kyphoplasty and Vertebroplasty for Vertebral Compression Fractures
Kyphoplasty and vertebroplasty are two minimally invasive methods for vertebral compression fractures. They involve injecting bone cement into the fractured vertebra to stabilize it and ease pain.
- Kyphoplasty creates a cavity in the vertebra before adding cement, aiming to restore some height.
- Vertebroplasty directly injects cement into the fracture to stabilize it.
Both methods are effective in reducing pain and improving mobility for patients with vertebral compression fractures.
MILD Procedure for Lumbar Spinal Stenosis
The MILD (Minimally Invasive Lumbar Decompression) procedure is a new approach for lumbar spinal stenosis. It removes a small part of the lamina to decompress the spinal canal and relieve nerve pressure.
This procedure is done under local anesthesia and has a quick recovery time. It’s a good option for those looking for relief from lumbar spinal stenosis symptoms.
Occipital Nerve Blocks for Migraine Management
Occipital nerve blocks are a valuable treatment for migraines. They involve injecting a local anesthetic and steroid around the occipital nerves to reduce inflammation and pain.
We often use occipital nerve blocks alongside other treatments for migraine management. The procedure is quick and can offer significant relief for migraine sufferers.
Advanced interventional techniques, like those mentioned, are a big step forward in treating complex pain conditions. They provide targeted and effective pain relief, improving the lives of those who haven’t found relief elsewhere.
The Science Behind Invasive Operations for Pain Relief
Invasive operations for pain relief are based on understanding pain and how the body reacts to injury. We look into how these methods help patients with chronic pain.
Mechanism of Action: How Pain Signals Are Interrupted
Interventions like ir injections target pain pathways. They interrupt or change these pathways to lessen or stop pain. This is done by using medication or techniques like radiofrequency ablation to block pain signals.
The body’s pain signals are complex, involving many neurotransmitters and pathways. Procedures aim to find and block the main pain sources. For example, epidural steroid injections can reduce inflammation around spinal nerves, lowering pain.
Duration and Efficacy of Different Interventional Approaches
The length and success of pain relief vary by procedure and patient. Some, like nerve blocks, offer quick relief lasting weeks to months. Others, such as spinal cord stimulation, can manage pain long-term by constantly adjusting signals.
Knowing how long and well each method works is key for setting patient expectations and making treatment choices. We work with patients to find the best treatment for their needs and history.
By understanding pain and using advanced techniques, we offer personalized pain relief solutions for each patient.
Technology and Precision in Interventional Pain Medicine
Technology has changed interventional pain medicine a lot. Now, treatments are more effective and have fewer side effects. This is thanks to technology, which has greatly improved patient care, back pain procedures included.
Imaging Guidance Techniques for Accuracy
Imaging guidance is a big tech advance in pain management. Fluoroscopy and ultrasound make procedures more accurate. Fluoroscopy shows X-rays in real time, helping place needles correctly for injections and blocks.
Ultrasound is a safe choice for soft tissue procedures. It doesn’t use radiation. These tools help target pain sources, making treatments more effective.
Minimizing Risks Through Advanced Technology
Advanced tech in pain procedures also cuts down risks. Precise imaging helps avoid nerve damage or infections. Radiofrequency ablation makes pain relief last longer by treating the right spots.
Also, tech helps create custom treatment plans. We can pinpoint pain sources and tailor treatments. This makes treatments work better and safer for patients.
Benefits and Risks of Interventional Pain Procedures
It’s important to know the benefits and risks of interventional pain procedures. These treatments have evolved a lot. They offer new pain management procedures for when other treatments don’t work.
Interventional pain specialists play a big role in helping patients. They are trained to treat chronic pain with minimally invasive methods. An interventional pain specialist helps diagnose and treat chronic pain.
Patient-Reported Outcomes and Satisfaction Rates
Many patients see big improvements after these treatments. For example, a study on epidural steroid injections showed many patients felt less pain and could function better.
| Procedure | Success Rate | Patient Satisfaction |
| Epidural Steroid Injections | 70% | 85% |
| Nerve Blocks | 65% | 80% |
| Radiofrequency Ablation | 75% | 90% |
Potential Complications and Side Effects
While these procedures are safe, they can have risks. Possible complications include infection, bleeding, and nerve damage. It’s key for patients to talk about these risks with their interventional pain specialist.
Recovery Time and Return to Function
Recovery times differ based on the procedure. For instance, nerve blocks might let patients get back to normal in a few days. But, more invasive surgeries might need longer recovery times.
Knowing what to expect during recovery is important. Our team helps patients with personalized care and guidance. This makes their recovery smoother.
When to Consider Interventional Pain Management
If chronic pain lasts even after trying usual treatments, it’s time to look into interventional pain management. This approach directly targets the pain source, helping those who haven’t seen relief from traditional methods. We’ll talk about who’s a good fit for these treatments and what the process involves.
Ideal Candidates for Interventional Procedures
People with chronic pain that hasn’t improved with usual treatments are often good candidates. They go through a detailed check to see if these procedures are right for them.
Choosing interventional pain management depends on several things. These include how bad the pain is, how it affects daily life, and the person’s overall health. Table 1 shows what makes someone a good candidate.
| Characteristics | Description |
| Chronic Pain | Pain that lasts longer than 3-6 months, beyond what’s normal |
| Failed Conservative Treatments | Not getting better with usual meds, therapy, or lifestyle changes |
| Significant Impact on Daily Life | Pain that affects daily activities, sleep, and quality of life |
The Consultation and Treatment Planning Process
The first step is a detailed check-up with a pain specialist. They look at your medical history, do a physical exam, and review your past treatments and tests.
In the consultation, the specialist talks about your symptoms, what you hope to achieve, and what you expect. They work together to create a treatment plan. This might include interventional injections or other pain management methods.
Conclusion
Interventional pain procedures are a valuable treatment for chronic pain. We’ve looked at different techniques, from simple to complex surgeries. These methods help manage various pain conditions.
These pain relief procedures can greatly reduce pain for many. This improves their life quality. Knowing the benefits and risks helps patients and doctors make better choices.
As we keep improving in interventional pain medicine, staying updated is key. We think these procedures will keep being a big part of pain management. They offer targeted relief when other treatments don’t work.
FAQ
What is an interventional pain specialist?
An interventional pain specialist is a doctor who treats chronic pain with small, non-invasive methods. They use injections and devices that are implanted under the skin.
What are interventional pain procedures?
These are medical treatments that use injections and devices to find and treat chronic pain. They are less invasive than traditional surgery.
What is the difference between minimally invasive and open surgery?
Minimally invasive procedures use small cuts and special tools. This causes less damage and leads to quicker healing. Open surgery, on the other hand, uses bigger cuts and more damage to tissues.
How do epidural steroid injections work for spinal pain?
These injections put corticosteroids near the spinal cord. This reduces swelling and eases pain.
What is radiofrequency ablation used for?
This procedure uses radio waves to heat up and damage nerves. It helps to relieve pain for a long time.
What are the benefits of interventional pain management?
It targets pain directly, giving lasting relief. It helps improve life quality for those who haven’t found relief with other treatments.
What are the possible risks and complications of interventional pain procedures?
Risks include infection, bleeding, nerve damage, and allergic reactions. But these are rare with proper care.
How long does it take to recover from interventional pain procedures?
Recovery time varies. But most people can get back to normal in a few days to a week.
What is spinal cord stimulation used for?
This involves a device that sends electrical impulses to the spinal cord. It blocks pain signals, helping with neuropathic pain.
Are interventional pain procedures covered by insurance?
Many are covered by insurance. But coverage can depend on the procedure and the insurance company.
What is the role of imaging guidance in interventional pain medicine?
Imaging like fluoroscopy and ultrasound helps make procedures safer and more accurate. It guides the doctor’s actions.
Can interventional pain management be used in conjunction with other treatments?
Yes, it can be used with other treatments like physical therapy and medication. This provides a full care plan.