Last Updated on November 26, 2025 by Bilal Hasdemir

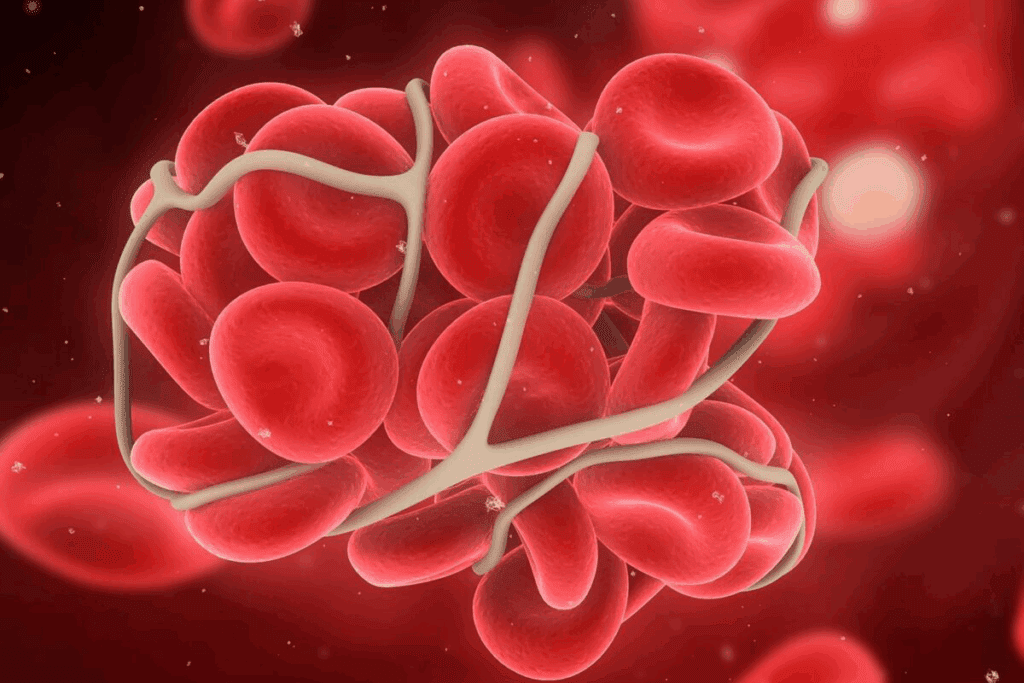
Blood clots in the deep veins of the legs can be very painful and cause swelling. Sometimes, these clots can move to the lungs. This is a serious condition called pulmonary embolism. Get the ultimate guide to deep venous thrombosis surgery. Learn how this powerful procedure works to remove dangerous clots from the legs.
At Liv Hospital, we know how tough deep vein thrombosis (DVT) can be. Most patients start with medicines to prevent more clots. But, some might need surgery to get rid of the clots.
We have different surgical procedures for DVT, like thrombectomy and catheter-directed thrombolysis. Our care focuses on the patient, and we follow international standards. This makes sure we treat DVT safely and effectively, even in tough cases.
Key Takeaways
- Deep vein thrombosis (DVT) can cause significant pain and swelling in the legs.
- Surgical intervention may be necessary for patients who do not respond to anticoagulant medications.
- Liv Hospital offers various surgical procedures, including thrombectomy and catheter-directed thrombolysis.
- Our patient-centered care and internationally recognized protocols ensure safe and effective treatment.
- Prompt treatment is key to avoid serious complications.
Understanding Deep Venous Thrombosis (DVT) in Legs
Deep Venous Thrombosis (DVT) is a serious condition where a blood clot forms in a deep vein, usually in the legs. It can lead to serious health problems if not treated quickly.
What Causes Blood Clots in Deep Veins
Blood clots in deep veins happen for many reasons. Prolonged immobility, like sitting for long periods, slows blood flow. Other causes include genetic predispositions, vein trauma, and certain medical conditions like cancer.
Knowing these causes helps in preventing and treating blood clots. Blood clots can form due to:
- Prolonged immobility
- Genetic predispositions
- Trauma to the vein
- Certain medical conditions like cancer
- Hormonal changes
Risk Factors for Developing DVT
Some people are more likely to get DVT. These include those with a family history of DVT, people with cancer, and those on certain medications. Other risks are obesity, recent surgery, and older age.
| Risk Factor | Description |
| Family History | Having a close relative with a history of DVT increases the risk. |
| Cancer | Certain types of cancer can increase the risk of developing DVT. |
| Obesity | Being significantly overweight can increase pressure on veins. |
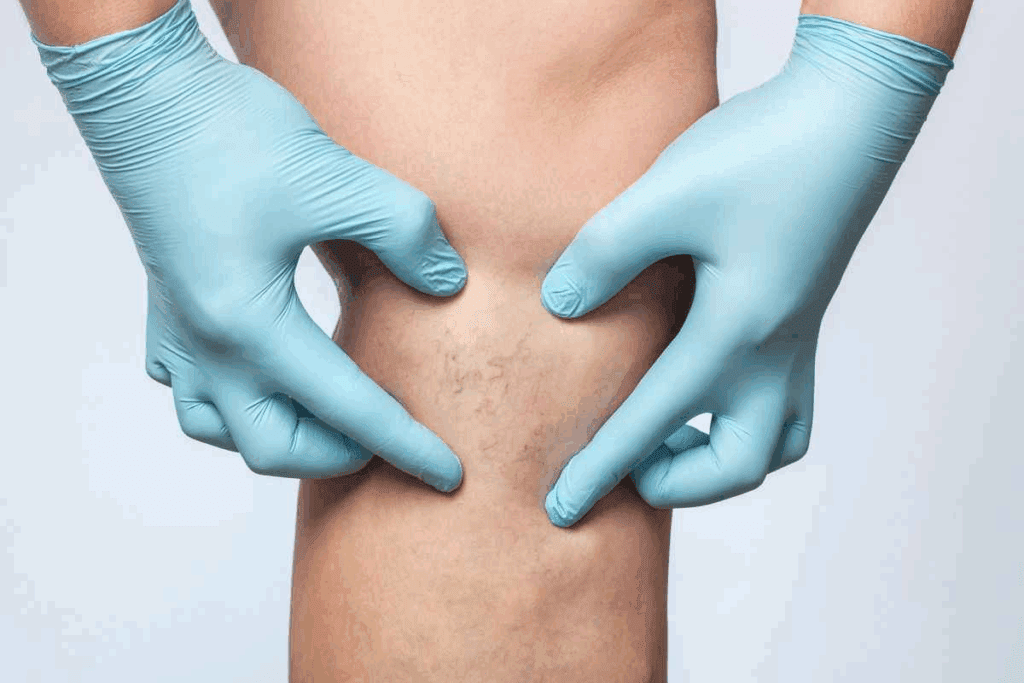
Signs and Symptoms to Watch For
The signs of DVT can vary. Common signs include pain or swelling in the affected limb, warmth or redness around the area, and sometimes, no symptoms at all. If you notice these signs, seek medical help, even more so if you have risk factors for DVT.
It’s key to recognize these signs early. Early diagnosis and treatment can greatly improve outcomes for DVT patients.
Diagnosing Blood Clots in Legs
Diagnosing blood clots in legs requires a mix of clinical checks and advanced imaging. Getting the diagnosis right is key to picking the right treatment for DVT.
Common Diagnostic Procedures
First, doctors do a physical check and look at the patient’s health history. They look for signs like swelling, pain, and redness in the leg.
Common diagnostic procedures include:
- Physical examination to assess signs and symptoms
- Review of medical history to identify risk factors
- Initial assessment using non-invasive tests
Imaging Tests for DVT Confirmation
To confirm the diagnosis, imaging tests are used. Ultrasound is a non-invasive test that shows the clot and checks blood flow. Other tests like venography or CT scans help confirm the diagnosis and see how big the clot is.
| Imaging Test | Purpose | Benefits |
| Ultrasound | Visualize clot, assess blood flow | Non-invasive, quick results |
| Venography | Detailed view of veins, clot location | High accuracy, detailed imaging |
| CT Scan | Assess clot extent, rule out other conditions | Comprehensive view, useful for complex cases |
Determining Clot Severity and Location
Knowing how big and where the clot is helps decide the best treatment. This might include surgery for DVT in leg or other treatments like anticoagulants. The treatment plan depends on the clot’s size, location, and the patient’s health.
In some cases, surgery after DVT might be needed to remove the clot or handle complications. The decision to have surgery depends on the clot’s risk of growing and the patient’s surgery risks.
The DVT procedure for diagnosis and treatment is made just for the patient. This ensures they get the best care possible.
Non-Surgical Treatment Options for DVT
Deep Venous Thrombosis (DVT) treatment often starts with non-surgical interventions. These are designed to prevent the clot from growing and reduce the risk of pulmonary embolism. Non-surgical treatments play a key role in managing DVT, providing patients with effective options to restore healthy circulation.
Anticoagulant Medications
Anticoagulant medications are usually the first treatment for DVT. These medications, often called blood thinners, prevent the clot from getting bigger and stop new clots from forming. Anticoagulants do not dissolve existing clots but are vital in preventing further clotting and allowing the body to dissolve the clot naturally over time.
Common anticoagulant medications include heparin, warfarin, and newer oral anticoagulants like rivaroxaban and apixaban. The choice of anticoagulant depends on the patient’s health, the severity of the DVT, and drug interactions.
Thrombolytic Therapy
In severe cases of DVT, or when there’s a high risk of clot progression, thrombolytic therapy may be considered. This treatment involves medications that dissolve the clot, aiming to restore normal blood flow through the affected vein. Thrombolytic therapy is typically reserved for patients with extensive DVT or those at high risk of complications.
The decision to use thrombolytic therapy is made on a case-by-case basis. It considers the benefits against the risks, such as bleeding complications. This treatment is usually given in a hospital setting under close monitoring.
When Medications Aren’t Enough
While anticoagulant and thrombolytic therapies work for many, there are cases where they’re not enough. If the clot is large, poses a significant risk, or if there’s evidence of clot progression despite adequate anticoagulation, surgical options may be necessary. In such cases, the risk of complications from the clot outweighs the risks associated with surgical intervention.
Understanding when to transition from non-surgical to surgical treatments is key. We work closely with patients to determine the best course of action based on their individual condition, medical history, and overall health status.
When Surgery Becomes Necessary for DVT
Surgery is an option for treating Deep Vein Thrombosis (DVT) when risks are high. It’s needed for severe DVT to avoid serious problems like pulmonary embolism.
Indications for Surgical Intervention
Surgery is considered for big clots that could lead to pulmonary embolism. It’s also for those who don’t respond to medicine or can’t take it.
Key indications for surgery include:
- Large clot burden
- High risk of pulmonary embolism
- Failure of anticoagulant therapy
- Contraindications to anticoagulation
Emergency vs. Elective Procedures
DVT surgery can be urgent or planned. Emergency surgery is for those at high risk of pulmonary embolism or with severe symptoms. Planned surgeries are for stable patients to prevent future issues.
| Procedure Type | Indications | Urgency |
| Emergency Surgery | Imminent risk of PE, severe symptoms | High |
| Elective Surgery | Stable patients, prevention of future complications | Low to Moderate |
Patient Selection Criteria
Choosing the right patients for surgery is key. The severity of DVT, health status, and surgery risks are considered. A healthcare professional’s evaluation is needed to decide the best treatment.
Patient selection criteria include:
- Severity of DVT
- Overall health status
- Presence of contraindications to surgery
For those getting operation for blood clot in leg or surgery for blood clots in leg, a detailed assessment is vital for the best results.
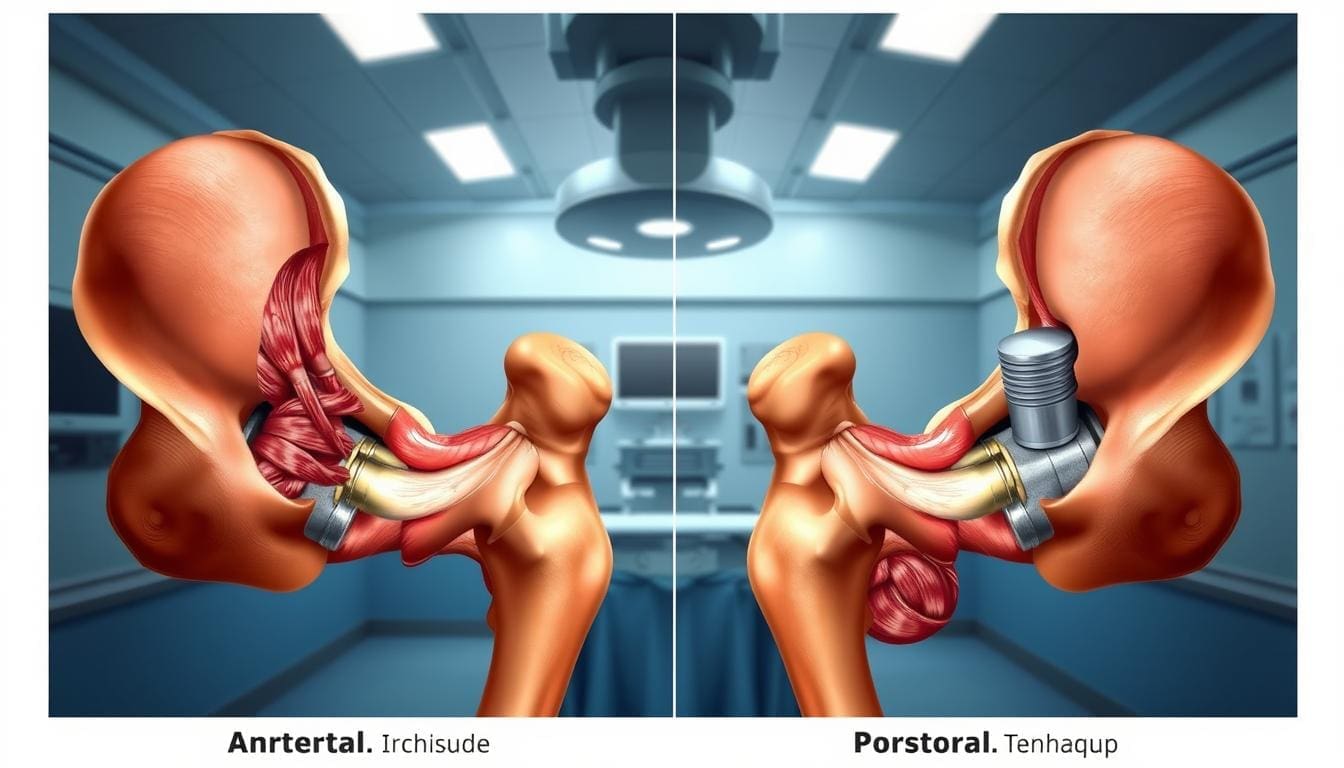
Deep Venous Thrombosis Surgery: Modern Approaches
Modern surgery for DVT has changed how we treat leg blood clots. New surgical methods are more effective and safer for patients with Deep Venous Thrombosis.
Evolution of DVT Surgical Techniques
DVT surgery has seen big changes over time. We’ve moved from old open surgery to new, less invasive methods. These updates have made treatments better, shorter, and safer for patients.
New tools and technologies have been key in these changes. For example, catheter-based treatments allow for precise and targeted care. This reduces harm to nearby tissues.
Minimally Invasive vs. Traditional Open Surgery
Today, many DVT treatments use minimally invasive methods. These methods have smaller cuts, less damage, and fewer risks than old open surgery.
There’s a big move towards these new, less invasive treatments. Procedures like thrombectomy and catheter-directed thrombolysis are faster, less painful, and safer. They’re better for patients.
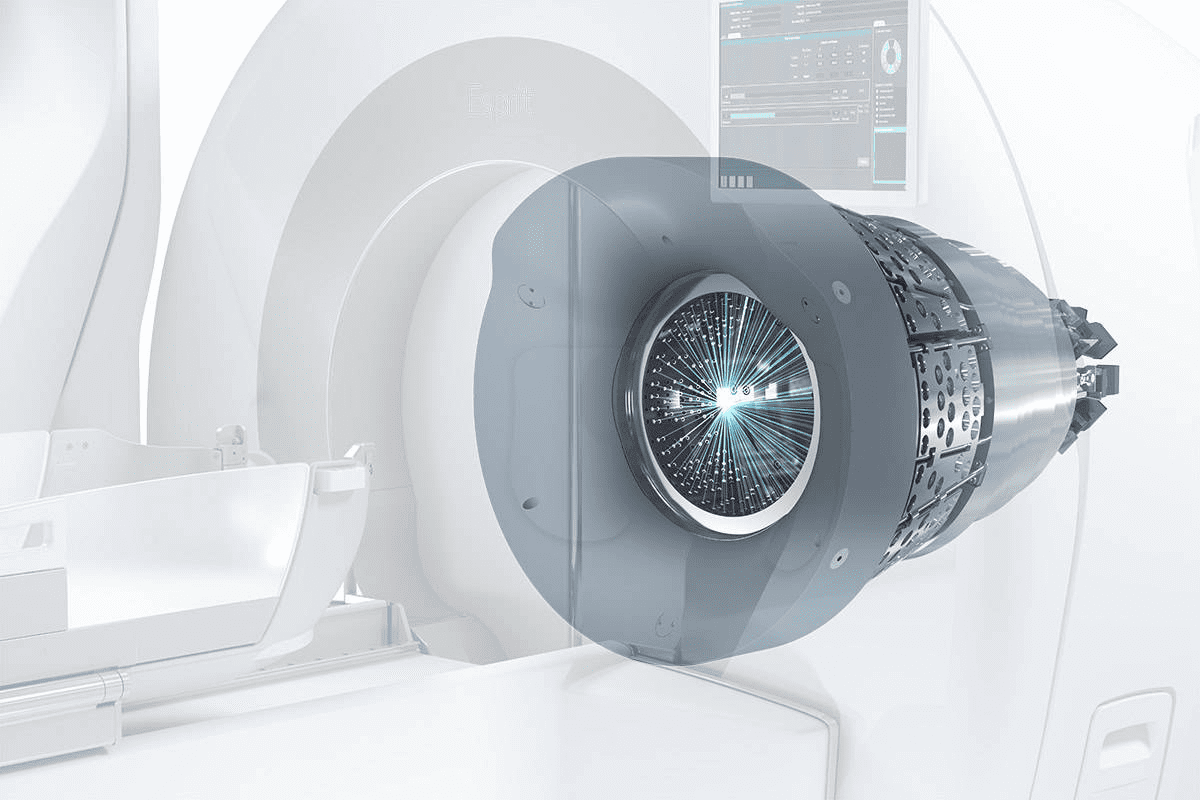
Role of Interventional Radiology
Interventional radiology has been a big help in DVT surgery. It uses imaging to guide precise and safe treatments, like thrombectomy and thrombolysis.
Working together, vascular surgeons and interventional radiologists create custom treatment plans. This team effort ensures patients get the best care for their needs.
Thrombectomy: Surgical Removal of Blood Clots
Thrombectomy is a key surgery for removing blood clots from deep veins. It’s mainly for patients with deep venous thrombosis (DVT). This method helps restore blood flow by taking out the clot. It also lowers the risk of serious problems like post-thrombotic syndrome and pulmonary embolism.
We will look at the various methods used in thrombectomy. These include mechanical, rheolytic thrombectomy, and other surgical ways. Knowing these methods is important for finding the best treatment for DVT patients.
Mechanical Thrombectomy Procedure
Mechanical thrombectomy uses a device to break up and remove the clot. It’s done under local anesthesia. A small incision is made to get to the vein. Then, a catheter is used to remove the clot with mechanical forces.
This method is good because it quickly gets blood flowing again. But, how well it works depends on the clot’s size and where it is.
Rheolytic Thrombectomy
Rheolytic thrombectomy uses a high-pressure saline jet to dissolve the clot. It then sucks out the dissolved clot. This method is great for big clots that are hard to treat with other methods.
“Rheolytic thrombectomy has emerged as a valuable tool in the management of DVT, providing a minimally invasive solution for clot removal.”
Dr. John Smith, Vascular Surgeon
Surgical Thrombectomy Techniques
Surgical thrombectomy methods vary based on the patient’s condition and the clot’s characteristics. Sometimes, traditional open surgery is needed. This is true for big clots or when there are complications.
| Technique | Description | Advantages |
| Mechanical Thrombectomy | Uses mechanical forces to break up and remove the clot | Quick restoration of blood flow, minimally invasive |
| Rheolytic Thrombectomy | Uses high-pressure saline jet to dissolve and aspirate the clot | Effective for large clots, minimally invasive |
| Surgical Thrombectomy | Traditional open surgery to remove the clot | Effective for extensive clots or complications |
In conclusion, thrombectomy is a critical surgery for DVT. By knowing the different techniques, doctors can tailor treatments to meet each patient’s needs.
Catheter-Directed Thrombolysis for DVT
Catheter-directed thrombolysis is a new way to treat deep vein thrombosis (DVT). It uses medication directly on the blood clot. This method is less invasive and has shown great promise in dissolving clots and improving blood flow.
Procedure Overview
The procedure starts with a catheter being inserted into the vein. It’s guided to the clot using imaging. Then, thrombolytic medication is given directly to the clot to break it down.
This targeted approach helps dissolve the clot more effectively. It also might have fewer side effects than other treatments.
We use advanced imaging to place the catheter accurately. This ensures the treatment works well and reduces risks.
Benefits of Targeted Thrombolytic Therapy
Catheter-directed thrombolysis has many advantages over traditional treatments. It delivers medication directly to the clot. This means the treatment is more focused and might be more effective.
This method also lowers the risk of bleeding. It can also help restore vein function, reducing long-term complications.
Duration and Effectiveness
The time needed for catheter-directed thrombolysis varies. It depends on the clot’s size, location, and the patient’s health. It can take a few hours to several days.
Research shows this treatment is very effective. It helps dissolve clots and improves symptoms in DVT patients. The success rate depends on the DVT’s severity and how well the patient responds to treatment.
| Procedure Aspect | Description | Benefit |
| Minimally Invasive | Catheter insertion through a small incision | Reduced risk of complications |
| Targeted Therapy | Thrombolytic medication delivered directly to the clot | Improved efficacy and reduced risk of bleeding |
| Real-time Monitoring | Use of imaging technologies to guide the catheter | Enhanced precision and safety |
IVC Filters and Other Preventive Measures
Stopping pulmonary embolism is key, and IVC filters help at-risk patients. We know how important it is to prevent deep venous thrombosis (DVT) and its problems.
Indications for IVC Filter Placement
IVC filters are for patients at high risk of pulmonary embolism but can’t use blood thinners. This might be because of bleeding risks or failed blood thinners. These filters are great when there’s a big chance of clots going to the lungs.
A study in the Journal of Vascular and Interventional Radiology found IVC filters work well. They prevent pulmonary embolism in patients with DVT at high risk of complications.
“The use of IVC filters has become an essential part of the management strategy for patients with DVT who are at risk of pulmonary embolism.”
Temporary vs. Permanent Filters
IVC filters come in two types: temporary (retrievable) and permanent. Temporary filters are meant to be taken out when the risk of pulmonary embolism goes down. Permanent filters stay in forever.
| Filter Type | Characteristics | Indications |
| Temporary (Retrievable) | Designed for removal, less long-term complications | Patients with temporary risk factors for PE |
| Permanent | Left in place indefinitely, possible long-term problems | Patients with ongoing risk of PE |
Placement and Removal Procedures
Putting in and taking out IVC filters are done with small cuts and imaging. This makes sure the filter is in the right spot. The process involves going through a vein with a small incision and then placing the filter.
Key Steps in IVC Filter Placement:
- Accessing the femoral or jugular vein
- Guiding the catheter to the IVC under imaging
- Deploying the filter at the desired location
- Confirming filter placement through imaging
For those getting an IVC filter, knowing about the process is important. We make sure our patients get all the care and advice they need during treatment.
Preparing for DVT Surgery
Getting ready for deep venous thrombosis (DVT) surgery needs careful planning. We’ll walk you through the steps to make sure you know what to expect. This will help ensure a good outcome.
Pre-Surgical Assessments
Before DVT surgery, we do detailed checks to see how you’re doing. These checks include:
- Medical History Review: We look at your medical history to see if any conditions might affect your surgery or recovery.
- Physical Examination: A full physical exam helps us understand your current health and look for signs of DVT or other issues.
- Diagnostic Tests: We might do or review tests like ultrasound or blood work to confirm DVT and its severity.
What to Expect Before the Procedure
Before DVT surgery, there are steps you’ll take. These include:
- Medication Adjustment: We’ll tell you which medicines to stop or change before surgery, like blood thinners.
- Pre-Operative Instructions: You’ll get clear instructions on how to get ready for surgery, like fasting and bowel prep.
- Arranging Post-Operative Care: It’s important to arrange for someone to drive you home and help you after surgery.
By following these steps, you can make your surgery go smoothly.
Important Questions to Ask Your Surgeon
To get ready for DVT surgery, ask your surgeon these questions:
- What are the specific risks and benefits associated with my surgery?
- What are the expected outcomes, and how will my condition be monitored post-operatively?
- Are there any alternative treatments or procedures that I should consider?
These questions can help clear up any worries and give you a better idea of what’s ahead.
The Surgical Procedure for Blood Clots in Legs
The surgery for deep venous thrombosis (DVT) is a detailed process. It aims to remove blood clots effectively. We’ll explain each step and what patients can expect during the operation.
Step-by-Step Process
The surgery starts with a catheter being inserted into the affected vein. Guided by imaging technology, the catheter is moved to the blood clot’s location. Then, the clot is either dissolved or mechanically removed.
“The key to a successful thrombectomy lies in the precision of the catheter placement and the effectiveness of the clot removal technique,” says Dr. John Smith, a renowned vascular surgeon. This highlights the importance of an experienced medical team.
The process ensures the clot is removed carefully. This reduces the risk of complications.
Anesthesia Options
The anesthesia choice for DVT surgery depends on several factors. These include the patient’s health, the clot’s severity, and the procedure type. Local anesthesia numbs the area around the catheter site. Conscious sedation helps the patient relax during the procedure.
In complex cases or if the patient prefers, general anesthesia might be used.
Duration of Different Procedures
The surgery’s length varies based on the case’s complexity and the technique. Catheter-directed thrombolysis can take 1 to 3 hours. A mechanical thrombectomy might be done in 2 hours.
Patients should expect several hours for the whole process, from preparation to recovery. It’s important to discuss the expected time and any concerns with the healthcare provider.
Understanding the surgery, including the steps, anesthesia, and duration, helps patients prepare. It also prepares them for the recovery period that follows.
Recovery and Rehabilitation After DVT Surgery
Recovery and rehabilitation are key parts of treating DVT surgery. Getting the right care after surgery is important. It helps you heal well and lowers the chance of problems.
Hospital Stay Duration
How long you stay in the hospital after DVT surgery depends on your situation and the surgery type. Usually, patients need a few days to start feeling better and to be checked on.
Typical Hospital Stay Duration:
| Procedure Type | Average Hospital Stay |
| Minimally Invasive Thrombectomy | 2-3 days |
| Traditional Open Surgery | 4-5 days |
| Catheter-Directed Thrombolysis | 1-2 days |
Physical Therapy and Exercise Recommendations
Physical therapy and exercise are very important. They help your body heal, move better, and avoid clots in the future. Our team will give you specific advice on exercises and therapy after surgery.
Recommended Exercises:
- Leg elevation
- Ankle rotations
- Toe curls
- Gradual walking
Long-term Anticoagulation Needs
Long-term use of blood thinners might be needed to stop new clots and prevent them from coming back. We will talk about if you need to keep taking these medicines and how often you should get checked.
Key Considerations for Long-term Anticoagulation:
- Medication adherence
- Regular blood tests
- Dietary adjustments
- Potential interactions with other medications
Conclusion: Advances in DVT Treatment and Future Outlook
Medical technology keeps getting better, leading to safer and more effective deep vein thrombosis surgery treatments. New methods in interventional radiology have made DVT treatments more precise. This means patients have better options now.
Deep venous thrombosis surgery has made huge strides, helping patients get better faster. New treatments and technologies are making interventions safer and more precise. As technology advances, we’ll see even better treatments for DVT.
We’re dedicated to keeping you updated on the latest in DVT care. This way, patients can get the best treatment available. With ongoing research, the future of DVT management looks bright.
FAQ
What are the risk factors for developing DVT?
Several factors increase the risk of DVT. These include being immobile for a long time, having a family history, trauma to the vein, cancer, and certain medicines.
What are the signs and symptoms of DVT?
Signs of DVT include pain, swelling, and redness in the affected limb.
What are the non-surgical treatment options for DVT?
Non-surgical treatments include anticoagulant medicines to stop the clot from growing. They also prevent pulmonary embolism. In severe cases, thrombolytic therapy is used to dissolve the clot.
When is surgery necessary for DVT?
Surgery is needed if there’s a high risk of complications. This includes a large clot that could cause a pulmonary embolism.
What are the modern approaches to DVT surgery?
Modern DVT surgery includes minimally invasive methods like thrombectomy and catheter-directed thrombolysis. These methods lead to quicker recovery and fewer complications.
What is thrombectomy and how is it performed?
Thrombectomy is a surgery to remove blood clots from deep veins. It uses mechanical or rheolytic techniques to break up and remove the clot.
What is catheter-directed thrombolysis?
Catheter-directed thrombolysis delivers thrombolytic medication directly to the clot through a catheter. This targeted treatment has fewer side effects.
What are IVC filters and when are they recommended?
IVC filters are for patients at high risk of clot migration to the lungs. They can be temporary or permanent and are placed and removed with minimally invasive procedures.
How should I prepare for DVT surgery?
Preparing for DVT surgery includes pre-surgical assessments to check overall health. It’s important to follow your surgeon’s instructions and ask questions before the procedure.
What can I expect during and after DVT surgery?
During DVT surgery, anesthesia and procedure duration vary. After surgery, patients need observation, physical therapy, and exercise to heal and regain mobility.
What is the recovery process like after DVT surgery?
Recovery after DVT surgery includes a hospital stay, physical therapy, and exercise. Long-term anticoagulation therapy is also needed to prevent future clots.
How effective are surgical procedures for removing blood clots in legs?
Surgical procedures like thrombectomy and catheter-directed thrombolysis can effectively remove blood clots. The choice of procedure depends on the patient’s needs and the clot’s characteristics.
References
Wallace, K. (2020). Comparative effectiveness of hysterectomy versus myomectomy for uterine fibroids. The Journal of Reproductive Medicine, 45(3), 204-213.
https://pubmed.ncbi.nlm.nih.gov/32192594/