
A stent is a small, metal mesh tube. It is put into a narrowed or blocked coronary artery. This helps restore normal blood flow to the heart. At Liv Hospital, we know facing heart symptoms can be scary. Knowing when a stent is needed is key for good treatment.
Coronary artery disease and acute heart attacks often require a stent. Many patients ask, “why would someone need a stent?” Symptoms like persistent angina that don’t get better with medicine also indicate you might need one. We aim to give you the best care, ensuring your treatment is safe and effective.
Key Takeaways
- A stent is a tiny, metal mesh tube that holds your artery open to improve blood flow.
- Coronary artery disease and acute heart attacks are primary reasons for needing a stent.
- Symptoms like persistent angina may indicate the need for a stent.
- Liv Hospital provides advanced, patient-centered care for heart stent treatments.
- Understanding when a stent is necessary is key for effective heart treatment.
Understanding Heart Stents: What They Are and How They Work

A heart stent is a tiny, expandable tube. It is placed in a narrowed or blocked artery. This keeps the artery open, allowing blood to flow to the heart.
We use stents during angioplasty. This is after we move plaque out of the way. It ensures the artery stays open.
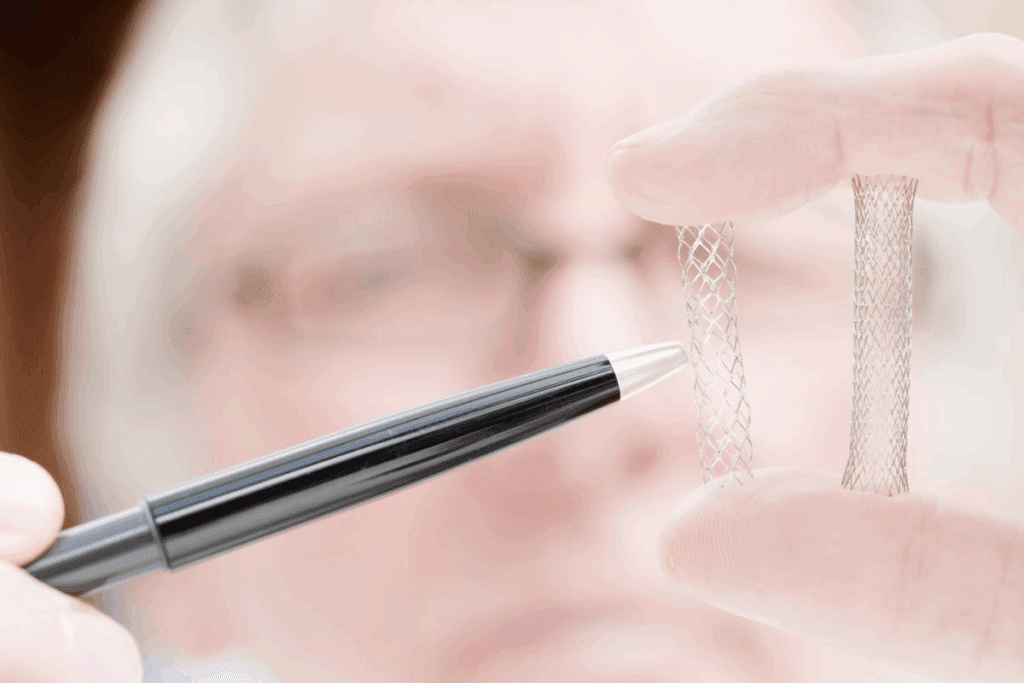
Definition and Structure of Cardiac Stents
Cardiac stents are small, mesh tubes. They are made from metal or other materials. They are designed to be inserted into the coronary arteries to keep them open.
The mesh structure makes the stent flexible and expandable. This makes it suitable for the heart’s dynamic environment.
The Function of Stents in Restoring Blood Flow
The main job of a stent is to restore blood flow to the heart. It keeps the coronary artery open. When plaque builds up, it can block the artery, reducing blood flow.
By placing a stent, we can push the plaque aside. This ensures the artery stays open, improving blood flow.
Types of Heart Stents Available Today
There are several types of heart stents available. Bare metal stents are made from metal mesh. They are designed to keep the artery open.
Drug-eluting stents are coated with medication. This helps prevent the artery from becoming blocked again. Biodegradable stents are made from materials that dissolve over time. This reduces the risk of long-term complications.
It’s important to understand the different types of stents. This helps us choose the best treatment for coronary artery disease. We consider the patient’s health, the blockage’s severity, and their medical history.
Coronary Artery Disease: The Primary Reason for Heart Stents
Coronary artery disease (CAD) is the main reason for heart stents. It happens when plaque builds up in the arteries. This buildup narrows the arteries and cuts down blood flow to the heart.
Plaque Buildup in Arteries
Plaque buildup, or atherosclerosis, starts early in life. High levels of low-density lipoprotein (LDL) cholesterol, smoking, and hypertension help it grow.
As plaque grows, it narrows the arteries. This is called stenosis. It limits blood flow to the heart muscle. This can cause chest pain or angina.
Progression of Coronary Artery Disease
CAD’s progression varies among people. Lifestyle, genetics, and other health conditions affect how fast it moves.
Some people may not show symptoms for years. Others may see rapid progression, leading to severe symptoms or heart attacks.
When CAD Becomes Severe Enough for Intervention
Doctors decide on stents when CAD severely limits blood flow. They use symptoms, stress tests, and imaging studies to make this decision.
When medication can’t manage symptoms, or there’s a high risk of heart attack, stents are considered. They help restore blood flow.
Understanding CAD’s progression helps doctors choose the right treatment. This includes knowing when a stent is needed.
Acute Heart Attacks: Emergency Stent Placement
During a heart attack, a stent can greatly improve outcomes. It quickly re-establishes blood flow to the heart muscle. We will explore how stents manage acute heart attacks, including recognizing symptoms and the need for quick medical action.
Recognizing a Heart Attack
It’s vital to recognize heart attack symptoms for quick medical help. Common signs include chest pain or discomfort, feeling like pressure or squeezing. Other symptoms include pain in arms, back, neck, jaw, or stomach, shortness of breath, lightheadedness, or cold sweats.
Not all heart attacks show chest pain. Women might feel nausea or fatigue instead. Spotting these signs early can lead to timely treatment, potentially saving lives.
How Stents Save Lives During Heart Attacks
Stents are small, mesh tubes that keep arteries open. They restore blood flow to the heart muscle during a heart attack. A stent can be placed as an emergency intervention to:
- Restore blood flow to the affected area of the heart
- Reduce damage to the heart muscle
- Improve survival chances
- Reduce the risk of further complications
Stents, specially drug-eluting stents, have changed acute heart attack treatment. They offer a minimally invasive procedure that greatly improves patient outcomes.
Time-Critical Nature of Intervention
The success of stent placement in treating a heart attack depends on time. The sooner the intervention, the better the outcome. Time is muscle; the longer the heart muscle is without blood, the more damage it suffers.
| Time from Symptom Onset | Impact on Heart Muscle | Outcome with Stent Placement |
| 0-90 minutes | Minimal damage | Excellent survival and recovery |
| 90-360 minutes | Moderate damage | Good survival, some heart damage |
| Beyond 360 minutes | Significant damage | Survival possible, but with substantial heart damage |
Understanding the urgency of heart attack treatment is key. Stent placement is a critical part of emergency care. It offers a lifeline to those experiencing a heart attack.
Persistent Angina: When Medication Isn’t Enough
When angina symptoms don’t go away with treatment, patients and doctors look for other ways to manage it. Angina is chest pain or discomfort caused by a temporary lack of blood flow to the heart.
Understanding Angina Symptoms
Angina symptoms can differ from person to person. They often include chest pain or discomfort. This pain can spread to the arms, back, neck, jaw, or stomach.
These symptoms usually happen when you exert yourself or feel stressed. They often get better when you rest or take medication.
Common symptoms of angina include:
- Chest pain or discomfort
- Pain or discomfort in one or both arms
- Pain or discomfort in the back, neck, jaw, or stomach
- Shortness of breath
- Fatigue
- Lightheadedness
Failed Medical Management
If medication doesn’t control angina symptoms, it’s time to rethink the treatment plan. This might mean trying more invasive procedures like stent placement.
Doctors decide on stent placement after careful evaluation. This includes tests like stress tests, echocardiograms, or coronary angiography.
Quality of Life Considerations
Persistent angina can greatly affect a patient’s quality of life. It can limit physical activity and impact mental health. Improving quality of life is key when considering stent placement.
Key quality of life considerations include:
- Ability to perform daily activities without symptoms
- Mental health and well-being
- Physical limitations due to angina
- Overall satisfaction with life
Understanding angina symptoms, recognizing when treatment fails, and considering quality of life helps doctors make informed decisions about stent placement.
Why Would Someone Need a Stent? Common Indications
Knowing when a stent is needed can help patients understand their heart health better. We suggest a stent when lifestyle changes and medicines don’t help enough.
A stent is often needed for big blockages in arteries, usually over 70%. This can cut down blood flow to the heart, causing pain or other symptoms.
Significant Artery Narrowing (70% or Greater)
Big blockages in arteries are a main reason for stent use. A stent can keep the artery open, improve blood flow, and ease pain. This usually happens because of plaque buildup in the arteries.
Doctors use a cardiac catheterization to check how narrow the artery is. They then decide if a stent is needed. The procedure involves a catheter, a balloon, and a stent to keep the artery open.
Unstable Cardiac Symptoms
Unstable heart symptoms, like sudden chest pain or pain when resting, also mean a stent might be needed. These signs show the heart isn’t getting enough blood, and quick action is required.
A stent can help get blood flowing to the heart muscle again. This lowers the chance of a heart attack. We look at how often and how severe these symptoms are to decide the best treatment.
Risk Factor Assessment
Looking at risk factors is key in deciding if a stent is needed. Things like age, health, and other medical conditions are important. For example, people with diabetes or heart disease history might need a stent.
By looking at these factors, we can give treatment plans that fit each person. Our aim is to improve heart health and lower the risk of future heart problems.
Diagnostic Process: How Doctors Determine Stent Necessity
Doctors decide if a heart stent is needed after a detailed check. This includes looking at symptoms, doing non-invasive tests, and sometimes invasive ones. We follow a clear path to see if a stent is required.
Initial Symptom Evaluation
The first step is to carefully check the patient’s symptoms. We look at the type, how bad it is, and how long it lasts. This helps us figure out what might be causing it and what tests to do next.
Symptom evaluation is key. It gives us our first hints about heart problems that might need a stent.
Non-Invasive Testing Methods
Next, we use non-invasive tests. These include:
- Stress tests to see how the heart works when stressed
- Electrocardiograms (ECGs) to check the heart’s rhythm
- Echocardiograms to see the heart’s structure and how it works
These tests help us understand the heart’s state and find any issues that need more looking into.
Cardiac Catheterization and Angiography
Cardiac catheterization and angiography are key for many patients. A catheter is put into an artery and guided to the heart. This lets us see the coronary arteries and find blockages.
Angiography, done during catheterization, gives clear pictures of the arteries. It shows where and how bad any blockages are. This info is vital for deciding if a stent is needed and where to put it.
By looking at all the test results, we can decide if a stent is needed. Then, we create a treatment plan that fits the patient’s specific situation.
Recognizing Symptoms That May Indicate Need for a Stent
Knowing when you might need a stent is key to getting the right care. Some symptoms can mean your heart health is at risk. A stent might be needed to fix blood flow problems.
Chest Pain Patterns That Suggest Intervention
Chest pain, or angina, is a common sign you might need a stent. It feels like pressure or pain in the chest, often when you’re active or stressed. The pain can spread to your arms, back, neck, jaw, or stomach.
If your chest pain is constant or gets worse, see a doctor right away. Some people have stable angina, which follows a pattern and gets better with rest or medicine. Others have unstable angina, which is severe and unpredictable. This is a serious emergency.
Shortness of Breath and Exertional Limitations
Shortness of breath, or dyspnea, can also mean you might need a stent. If your heart isn’t getting enough blood, you might find it hard to breathe. Even simple tasks can leave you tired.
If you get winded easily or feel tired all the time, talk to your doctor. They can check if your symptoms are heart-related and if a stent is needed.
Unusual Symptoms in Women, Elderly, and Diabetics
Some groups might have different symptoms. Women might feel sharp pain in their neck, jaw, or back, or stomach discomfort. Older people might feel confused, dizzy, or faint because of heart issues.
Diabetics might not feel pain in the usual way because of nerve damage. So, any strange symptoms should be checked by a doctor.
| Symptom | Description | Population Most Affected |
| Chest Pain (Angina) | Pressure or squeezing in the chest, often triggered by exertion or stress | General Population |
| Shortness of Breath (Dyspnea) | Difficulty breathing at rest or during light activities | Elderly, Heart Failure Patients |
| Unusual Pain Locations | Pain in the neck, jaw, back, or abdomen instead of or in addition to chest pain | Women |
| Fatigue and Exertional Limitations | Unusual tiredness or inability to perform daily tasks without fatigue | General Population, Diabetics |
Age Considerations: Is There an Age Limit for Heart Stents?
Whether or not a heart stent is right for you depends on your health, not just how old you are. Many people over 50 get heart stents. But, more and more younger people are getting them too because heart disease is becoming more common among them.
Stent Placement in Older Adults
Older adults often face more health challenges, like many blockages and other health issues. Being older doesn’t mean you can’t get a stent. But, doctors carefully think about your health and risks before deciding.
When considering stents for older adults, doctors look at:
- Other serious health problems
- The seriousness and location of blockages
- How well you can recover
Younger Patients and Heart Stents
Even younger people can benefit from heart stents, if they have big blockages or symptoms like chest pain or trouble breathing. Doctors carefully think about the long-term effects, like if more treatments will be needed.
For younger patients, things like lifestyle, family history, and other risk factors are important in making decisions.
Health Status vs. Chronological Age
The choice to get a heart stent really depends on your health, not just how old you are. Comprehensive evaluations help doctors decide the best treatment.
Doctors look at:
- The severity of heart disease
- How symptoms affect your life
- How well you respond to other treatments
By looking at your health, not just your age, doctors can make better choices about heart stents.
Risks and Benefits of Heart Stent Procedures
Choosing to get a heart stent is a big decision. It’s about looking at the good sides and the possible downsides. Heart stents help keep blood flowing well to the heart. They also help ease symptoms of coronary artery disease.
Potential Complications During Placement
Stent placement is usually safe, but there are risks. These include bleeding, blood clots, and restenosis (when arteries narrow again). These issues are rare but serious.
Long-Term Risks to Consider
There are also long-term risks with heart stents. Patients might face stent thrombosis (a blood clot in the stent). Another risk is restenosis inside the stent. These need to be watched over time.
Weighing Benefits Against Possible Risks
Despite risks, heart stents offer big benefits for many. They improve blood flow, reduce chest pain, and boost life quality. It’s key to talk to your doctor about your specific situation.
Deciding on a heart stent means looking at your condition, the success rate of the procedure, and how it affects your life. Knowing these details helps you choose the best treatment for you.
Alternatives to Stenting: When Other Treatments Are Considered
There are other treatments for coronary artery disease (CAD) aside from stenting. These include medication, coronary artery bypass grafting (CABG), and lifestyle changes. The right treatment depends on the disease’s severity, the patient’s health, and their medical history.
Medication-Only Approaches
For some, just using medicine is the best option. This involves a mix of drugs to manage symptoms and slow disease growth. Drugs like antiplatelets, beta-blockers, ACE inhibitors, and statins are used. The aim is to control symptoms and improve life quality without surgery.
Effective medication management can greatly help patients with CAD. It’s important to regularly check and adjust the treatment to keep it working well and manage side effects.
Coronary Artery Bypass Grafting (CABG)
CABG is a surgery that bypasses blocked arteries with grafts. These grafts are usually from the patient’s own veins or arteries. It helps improve blood flow to the heart, reducing symptoms and potentially improving long-term health.
CABG is often suggested for those with complex or multi-vessel disease, like those with diabetes. It’s a more invasive option than stenting but can offer big benefits for the right patients.
Lifestyle Modifications as Treatment
Lifestyle changes are key in managing CAD, whether stenting or other treatments are used. Eating a heart-healthy diet, being more active, quitting smoking, and managing stress are important. These changes can slow disease growth, improve symptoms, and boost heart health.
Patient education and support are vital to help people stick to these lifestyle changes.
In summary, while stenting is a common treatment for CAD, other options like medication, CABG, and lifestyle changes are also important. The best treatment plan is one that fits the patient’s specific needs and situation.
Life After a Heart Stent: Recovery and Long-Term Management
Recovering after a heart stent involves taking medicine, making lifestyle changes, and regular check-ups. Knowing what’s needed can greatly help your heart health and the stent’s success.
Medication Requirements
Patients often take medicines to stop blood clots and manage heart issues after a stent. Antiplatelet therapy, like aspirin and P2Y12 inhibitors, is key to prevent clots on the stent. The time needed for these medicines can be 6 to 12 months, based on the stent type and patient’s health.
Other drugs help control cholesterol, blood pressure, and heart risks. Taking your medicines as directed is essential for the stent’s success and heart health.
| Medication Type | Purpose | Typical Duration |
| Antiplatelet Therapy (e.g., Aspirin, P2Y12 inhibitors) | Prevent blood clots on the stent | 6 to 12 months |
| Statins | Lower cholesterol levels | Ongoing |
| Beta-blockers | Manage blood pressure and heart rate | Ongoing |
Activity Restrictions and Resumption
Right after the stent, you might need to avoid hard work and heavy lifting for a few days to a week. Slowly getting back to normal activities with your doctor’s advice is best. Most people can get back to their usual routine in a week, but it depends on your health and the procedure details.
Lifestyle Changes for Heart Health
After a heart stent, making long-term lifestyle changes is key to keep your heart healthy and prevent more artery disease. Eating a heart-healthy diet with lots of fruits, veggies, whole grains, and lean proteins is important. Regular exercise, like walking, is good, but talk to your doctor about how much and how hard.
Other lifestyle changes include quitting smoking, managing stress with meditation or yoga, and keeping a healthy weight. These steps help the stent work well and improve your heart health.
By following these recovery and long-term management tips, patients can greatly improve their outcomes after a heart stent.
Conclusion: Making Informed Decisions About Heart Stents
Understanding heart stents is key for patients to make smart choices about their health. We’ve looked at what heart stents are, how they work, and what they treat. This includes coronary artery disease and acute heart attacks.
Knowing how doctors diagnose heart stent needs is important. This includes checking symptoms, using non-invasive tests, and doing cardiac catheterization and angiography. Spotting symptoms like chest pain and shortness of breath is also critical.
Patients should think about the good and bad sides of heart stent procedures. Age, health, and lifestyle changes matter in making choices. This way, patients can work with doctors to find the best treatment, improving their life and health.
Getting to know about heart stents is essential for patients. Being informed helps them take charge of their health. This ensures they get the right treatment for their condition.
FAQ
What is a heart stent and why is it used?
A heart stent is a small, mesh-like device. It’s placed in a coronary artery to keep it open. This improves blood flow to the heart. We use stents to treat coronary artery disease and acute heart attacks.
What are the symptoms that may indicate the need for a stent?
Symptoms like chest pain or discomfort, shortness of breath, and exertional limitations may mean you need a stent. We also look at unusual symptoms in specific groups like women, the elderly, and diabetics.
How do doctors determine if a stent is necessary?
To decide if a stent is needed, we go through a diagnostic process. This includes checking symptoms, using non-invasive tests, and doing cardiac catheterization and angiography.
What are the common indications for needing a stent?
Common reasons for needing a stent include artery narrowing of 70% or more. We also consider unstable cardiac symptoms and risk factors.
Is there an age limit for heart stent placement?
Age isn’t as important as health status when deciding on stent placement. Both older adults and younger patients can get stents.
What are the risks and benefits associated with heart stent procedures?
Heart stent procedures have risks during and after placement. But, they also offer benefits like improved blood flow and reduced symptoms.
What are the alternatives to stent placement?
Alternatives include medication-only approaches, coronary artery bypass grafting (CABG), and lifestyle changes.
What happens after a heart stent is placed?
After a stent is placed, we require medication to prevent clotting. There may be activity restrictions. We also recommend lifestyle changes for long-term heart health.
Can lifestyle changes prevent the need for a stent?
Lifestyle modifications can manage coronary artery disease and potentially prevent stent need. We suggest a healthy diet, regular exercise, and stress management.
How do stents save lives during heart attacks?
Stents can restore blood flow during heart attacks. This reduces damage to the heart muscle and improves outcomes.
Why do people get stents?
People get stents to treat coronary artery disease, acute heart attacks, and persistent angina. Stents improve blood flow and reduce symptoms.
What are the different types of heart stents available?
There are different types of heart stents, including bare metal, drug-eluting, and biodegradable stents. We choose the best type based on individual patient needs.
How do I know if I need a stent?
We evaluate symptoms, medical history, and test results to decide if a stent is needed. If you’re experiencing symptoms or concerns, consult a healthcare professional.
References
Bicket, M. C., et al. (2013). Epidural injections for spinal pain: A systematic review and meta-analysis. Pain Physician, 16(5), E453-E470. https://pubmed.ncbi.nlm.nih.gov/24195874/








