Last Updated on November 26, 2025 by Bilal Hasdemir

Chronic pain affects millions worldwide. Effective pain management is key to better living. Interventional pain procedures are a fast, non-invasive way to help.
We lead in pain management with cutting-edge tools. Tools like R software, protection aprons, and lead drapes are vital. They help make treatments safer and more effective. These tools also reduce risks from radiation during procedures.
Key Takeaways
- Interventional pain procedures offer rapid and effective relief for chronic pain.
- Advanced tools enhance the safety and efficacy of pain management procedures.
- Integration of R software improves data analysis and decision-making.
- Protection aprons and lead drapes minimize radiation exposure risks.
- Effective pain relief procedures improve patient outcomes and quality of life.
The Rising Importance of Interventional Procedures in Pain Management
More people are turning to interventional pain management techniques due to chronic pain. This pain affects millions, crossing all age, gender, and economic lines. Healthcare is looking for new ways to help manage this pain.
Chronic pain is a big problem worldwide. It costs a lot in lost work, healthcare, and social services. The World Health Organization calls it a major public health issue, showing we need better ways to handle it.
The Global Impact of Chronic Pain
Chronic pain affects about 1 in 5 adults globally. It can come from injuries, infections, or diseases like arthritis. It deeply affects people’s lives, causing lower quality of life, mental health problems, and loneliness. Chronic pain medical procedures are becoming key in fighting this global health issue.
When Traditional Treatments Fall Short
Medicine and physical therapy don’t work for everyone. Some people don’t get enough relief or can’t handle medication side effects. That’s where pain management interventions help, using minimally invasive pain procedures. These procedures are very effective, with over 70% of patients being satisfied.
Healthcare providers are learning the limits of old treatments and the value of new ones. This knowledge helps them give better care to those with chronic pain. As the field grows, we’ll see even more ways to improve patient care.
Most Common Interventional Procedures for Chronic Pain
Interventional pain management has made big strides, helping those with chronic pain. Now, we have many effective methods that fit each patient’s needs. This brings hope to those who haven’t found relief with traditional treatments.
Interventional procedures are key in managing chronic pain. They help patients who have tried everything else. These methods aim to stop pain signals and help patients live better lives.
Epidural Steroid Injections and Nerve Blocks
Epidural steroid injections and nerve blocks are top choices for chronic pain. Epidural steroid injections put corticosteroids near the spinal cord to cut down inflammation and pain. Nerve blocks inject local anesthetics or steroids around nerves to block pain signals.
These methods work well for chronic back pain and radiculopathy. Studies show they can greatly reduce pain and improve function in patients with lumbar disc herniation.
Radiofrequency Ablation Techniques
Radiofrequency ablation (RFA) is a common procedure for chronic pain. It uses radiofrequency waves to heat up and damage nerves that carry pain signals. It’s great for treating facet joint and sacroiliac joint pain.
RFA can offer long-lasting pain relief. Some studies show pain relief can last up to a year or more after the treatment.
Spinal Cord Stimulation and Joint Injections
Spinal cord stimulation (SCS) involves implanting a device that sends electrical impulses to the spinal cord. This stops pain signals before they reach the brain. It’s for patients with severe, chronic pain that other treatments haven’t helped.
Joint injections, like intra-articular injections, are used for arthritis or joint degeneration pain. They can greatly reduce pain and improve joint function.
Emerging Procedures: Kyphoplasty and MILD
New techniques like kyphoplasty and MILD (Minimally Invasive Lumbar Decompression) are becoming more popular. Kyphoplasty treats vertebral compression fractures, while MILD is for lumbar spinal stenosis.
These new methods offer relief with less recovery time. Studies show they are safe and effective, with over 70% of patients very satisfied.
The Science Behind Effective Interventional Procedures
Effective interventional procedures need a deep understanding of pain and proven practices. As interventional pain specialists, we always aim to learn more about pain pathways. This knowledge helps us give our patients the best care.
Interrupting Pain Pathways
Interventional pain procedures target specific pain pathways to reduce pain signals to the brain. Techniques like nerve blocks and spinal cord stimulation are used to block these pathways. Knowing how pain is transmitted helps us choose the right procedure for each patient.
Evidence-Based Outcomes and Success Rates
Many studies show that interventional pain procedures work well for chronic pain. They help many patients feel better and live better lives. As an interventional pain specialist, keeping up with new research is key to providing top-notch care.
The success of these procedures depends on the condition and how each patient responds. But, with the right approach, many procedures are very effective. This makes them a valuable part of treating chronic pain.
Essential Equipment for Modern Interventional Pain Specialists
The world of interventional pain management has changed a lot. This is thanks to new tools and technology. These advancements have made it possible to do more in pain management.
The Evolution of Procedural Tools
Today, pain specialists use many different tools for pain clinic procedures. New tools have made these procedures more precise and safe. For example, better needles and delivery systems help with injections and lower risks.
Also, using R software in planning has helped analyze data better. This data-driven approach makes care more personalized and effective.
How Technology Has Improved Patient Outcomes
Technology has greatly improved patient results in pain management. New pain management procedures have better success rates and shorter recovery times. For instance, advanced imaging systems help guide procedures better.
Also, new radiation protection tools have lowered risks for staff and patients. This makes treatments safer for everyone involved in intervention pain management.
Looking ahead, technology and new equipment will keep changing pain management. By using these advancements, we can keep improving care and patient results.
Tool #1: Advanced Imaging Systems for Precision Guidance
Advanced imaging systems have changed the game in interventional pain management. They offer precise guidance during procedures. This is key for the accuracy and safety of many techniques.
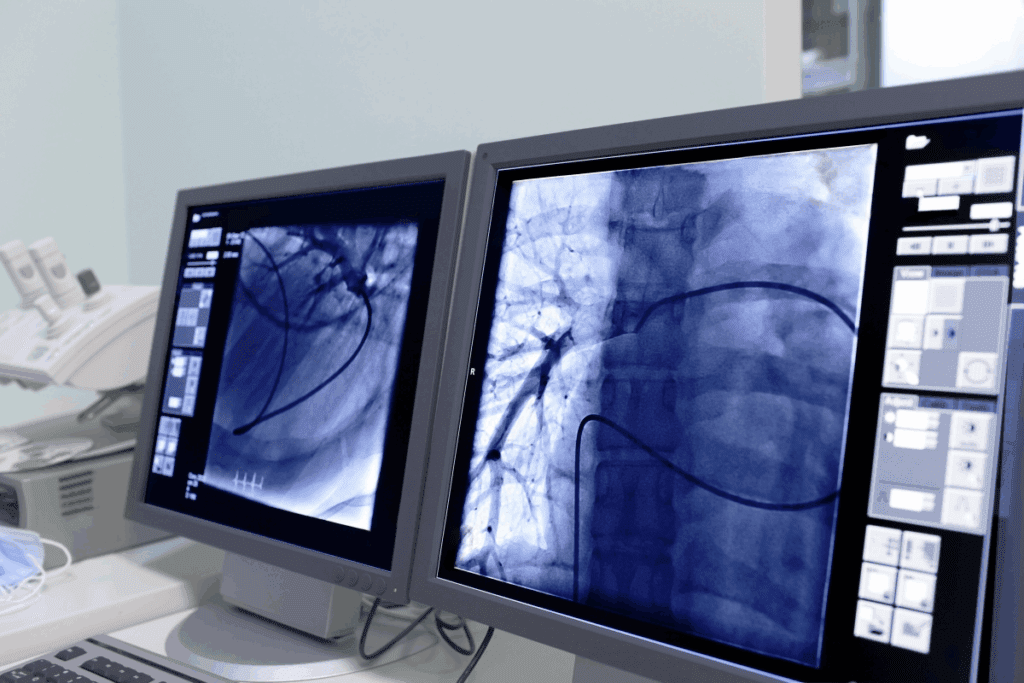
Fluoroscopy and Real-Time Visualization
Fluoroscopy is a top choice in interventional pain management. It shows what’s happening in real-time. This helps place needles and instruments exactly right.
For things like epidural steroid injections and nerve blocks, fluoroscopy is a game-changer. It lets us guide the needle to the right spot. This cuts down on risks and boosts patient results.
Ultrasound Guidance for Soft Tissue Procedures and Emerging Techniques
Ultrasound is a must-have for soft tissue procedures. It’s great for injections into muscles and tendons. Ultrasound gives a clear look at soft tissues, making it easy to target the right area.
New techniques like ultrasound-guided nerve blocks are gaining traction. They’re known for their accuracy and safety. We’re seeing more use of ultrasound with other imaging to up the precision.
CT and MRI Integration in Complex Cases
For tough cases, CT and MRI are invaluable. They give detailed views of the body’s inside. This helps plan and do procedures with great precision.
We use CT and MRI for precise tasks like spinal cord stimulator placements. Their detailed images help us navigate tricky anatomy with confidence.
| Imaging Modality | Primary Use | Benefits |
| Fluoroscopy | Real-time guidance for injections and needle placements | Real-time visualization, precise needle placement |
| Ultrasound | Soft tissue procedures, nerve blocks | Clear visualization of soft tissues, high accuracy |
| CT and MRI | Complex cases requiring detailed cross-sectional imaging | Detailed images, precise planning and execution |
Tool #2: Radiation Protection Aprons – Critical Safety Equipment
The need for radiation protection is huge for healthcare workers doing interventional procedures. As we move forward in pain management, keeping patients and doctors safe is key.
Types of Protection Aprons for Different Procedures
Radiation aprons are made for various procedures. Lead aprons are the classic choice, great at blocking radiation. But, new lead-free and lightweight aprons offer the same protection with more comfort and flexibility.
Research shows lead-free aprons work just as well as lead aprons. This makes them a good option for pain specialists.
| Type of Apron | Material | Radiation Protection Level | Comfort Level |
| Traditional Lead Apron | Lead | High | Moderate |
| Lead-Free Apron | Composite Materials | High | High |
| Lightweight Apron | Advanced Polymers | High | Very High |
Material Advancements in Radiation Protection
New materials in aprons have made them better and more comfortable. Today’s aprons use advanced composites and polymers. They block radiation well and are lighter and more flexible.
Proper Fitting and Maintenance for Maximum Protection
It’s important to fit and maintain aprons right for best protection. A good apron fits well, covering important areas without getting in the way. It’s also key to check for damage and store them properly.
Using the right aprons helps pain specialists stay safe from radiation. This lets them keep giving top-notch care to their patients.
Tool #3: Lead Drapes for Complete Radiation Shielding
Complete radiation shielding is key for lowering radiation exposure in complex medical procedures. Lead drapes play a big role in this, adding an extra layer of protection.
Strategic Placement of Lead Drapes During Procedures
Putting lead drapes in the right place is very important. We surround the patient and the X-ray source with them to cut down on scatter radiation. This not only keeps the patient safe but also lowers the risk for medical staff.
To place them effectively, we need to know the procedure’s layout and where radiation goes. By carefully setting up the lead drapes, we can greatly lessen the radiation dose to sensitive areas.
Combining Lead Drapes with Other Protection Methods
Lead drapes work best when paired with other radiation protection tools. Using them with personal protective equipment (PPE) like lead aprons, thyroid shields, and lead glasses gives full protection.
This layered approach keeps both patients and medical staff safe from radiation harm. We always check and update our safety measures to keep up with the highest standards.
Latest Innovations in Radiation Barrier Technology
New tech in radiation barriers has brought better and more flexible lead drapes. These advancements include lighter materials that offer the same or better protection than old lead drapes.
There are also new designs that are more flexible. This makes it easier to place them right during procedures. We keep up with these new developments to keep our safety practices leading.
Tool #4: Specialized Needles and Delivery Systems
Needle design and delivery systems have improved a lot. This has made interventional pain procedures more precise and safe. Specialized needles and systems are key to their success.
Needle Design for Specific Interventional Applications
Needles for pain management have changed a lot. They are now made for specific procedures. This ensures they work well and safely.
“Atraumatic needles” are made to cause less damage. Studies show they reduce pain after procedures. They are designed to be precise and safe.
Now, needles come in different shapes and sizes. They have adjustable lengths and tips. This helps doctors reach and treat pain spots better.
Catheter Systems for Continuous Medication Delivery
Catheter systems deliver medicine right to the pain site. They are great for long-term pain relief. This method keeps the medicine level steady, making treatment more effective.
Catheter systems have gotten better. They can adjust how fast they release medicine. Patients can even control it themselves. This makes treatment plans more personal.
Advancements in Needle Visibility and Control
New needle tech makes procedures safer. Tools like real-time ultrasound guidance and fluoroscopy let doctors see the needle as they work. This ensures it’s placed correctly.
“The integration of advanced imaging techniques with needle placement has revolutionized interventional pain management, making it safer and more precise.”
Needles that show up well under ultrasound are also new. They help doctors avoid mistakes. These changes make pain procedures safer and more effective.
Tool #5: Integrating R Software for Procedure Planning and Analysis
R software is changing the game in interventional pain management. It makes planning and analyzing procedures better. This is thanks to R programming, which brings advanced data analysis and personalized treatment plans to the table.
How R Programming Enhances Interventional Procedures
R programming boosts interventional procedures with its top-notch statistical analysis and data visualization. Clinicians can now better understand patient data and spot trends. This helps them make smarter treatment choices.
Key benefits of using R in interventional procedures include:
- Advanced data analysis and modeling
- Improved outcome prediction
- Personalized treatment planning
- Enhanced data visualization
Data Analysis and Outcome Prediction Using R
R software shines when it comes to complex data analysis in pain management. It uses statistical models and machine learning to forecast patient outcomes. This way, clinicians can tailor treatments for better results.
| Analysis Type | R Package Used | Outcome |
| Regression Analysis | stats | Predicting pain relief duration |
| Survival Analysis | survival | Estimating time to pain recurrence |
| Cluster Analysis | cluster | Identifying patient subgroups |
Case Studies: R Integration Success Stories
Many case studies show R software’s success in pain management. For example, a study in the Journal of Pain Research used R to study spinal cord stimulation. It found key factors for success.
Another study used R to analyze radiofrequency ablation outcomes. R’s data visualization helped find the best treatment settings.
By using R software, doctors can make interventional pain management more precise and effective. This leads to better patient outcomes.
Tool #6: Radiofrequency Generators and Probes
In the world of pain management, radiofrequency generators and probes are key. They help us give targeted pain relief. We use these tools to help patients with chronic pain in a way that’s less invasive.
Principles of Radiofrequency Technology in Pain Management
Radiofrequency (RF) technology uses electrical energy to heat nerves. This stops pain signals from reaching the brain. It’s a mainstay in pain management.
We use RF to treat chronic pain like arthritis, back pain, and neck pain. It’s precise, so we can target pain without harming other tissues.
Selecting the Right RF System for Different Procedures
Choosing the right RF system is key for success. The type of pain, where it is, and the patient’s health matter. These factors help us pick the best system.
| Procedure | RF System Characteristics | Benefits |
| Facet Joint Denervation | High-frequency RF, precise temperature control | Effective for long-term pain relief |
| Painful Neuroma | Pulsed RF, lower temperatures | Minimizes risk of nerve damage |
| Chronic Back Pain | Continuous RF, high-temperature capability | Provides significant pain reduction |
Safety Protocols for RF Procedures
Safety is top priority in RF procedures. We follow strict rules to keep patients safe. This includes choosing the right patients, using careful techniques, and watching them closely before and after.
Key safety measures include:
- Using sterile equipment to prevent infection
- Monitoring patient vital signs during the procedure
- Employing imaging guidance for precise needle placement
- Providing clear post-procedure instructions to patients
By sticking to these safety steps and choosing the right RF system, we make sure radiofrequency ablation works well. We also keep risks low.
Tool #7: Contrast Media and Medication Delivery Systems
Contrast media and precise medication delivery are key in modern interventional procedures. They make treatments safer and more effective. This allows for better diagnoses and targeted therapies.
Types of Contrast Agents Used in Interventional Procedures
Different contrast agents are used to see inside the body during procedures. The right agent depends on the procedure and the patient’s health history.
- Iodine-based contrast agents are often used for vascular procedures because they improve X-ray images.
- Gadololinium-based agents are best for MRI procedures, showing soft tissues clearly.
- Barium sulfate is used for some GI studies, giving detailed views of the digestive system.
Precision Medication Delivery Technologies
New technologies in medication delivery have made procedures more precise and effective. These technologies help deliver medications directly to the right place. This reduces side effects and improves patient results.
- Catheter-based delivery systems allow for direct medication administration, boosting treatment success.
- Programmable infusion pumps offer controlled medication delivery, meeting each patient’s needs.
- Nanoparticle-based delivery systems are being developed to target specific cells or tissues, promising more precise treatments.
Managing Contrast Reactions and Complications
While contrast media and medication delivery systems are mostly safe, there are risks of adverse reactions and complications. It’s important to have strategies in place to manage these risks.
- Pre-procedure assessment is key to identify patients at risk of contrast reactions, allowing for preventive steps.
- Monitoring during and after the procedure helps catch and manage any adverse reactions early.
- Emergency preparedness includes having plans for severe reactions, like anaphylaxis.
Understanding contrast agents, using precise medication delivery technologies, and being ready for complications helps healthcare providers. This ensures the safety and success of interventional procedures.
Conclusion: The Future of Interventional Pain Management Tools
The field of interventional pain management is growing fast. New tools and technologies are changing how we handle pain. The future looks bright, with better safety and results for these treatments.
Tools like R software, protection aprons, and lead drapes are already helping a lot. R software helps plan and analyze procedures. Aprons and drapes protect against radiation. We can expect even better tools to help manage chronic pain in the future.
These tools will likely lead to better results for patients. They will help make treatments more tailored to each person. With these advancements, we’re getting closer to a world where chronic pain is better managed. This will improve life for people everywhere.
FAQ
What are interventional pain procedures?
Interventional pain procedures are treatments that help manage chronic pain. They work by stopping pain signals and helping the body function better.
What is the role of R software in interventional pain management?
R software helps plan and analyze procedures. It predicts outcomes and improves data analysis. This makes pain management more effective.
Why are radiation protection aprons important in interventional procedures?
Radiation protection aprons keep healthcare workers safe from radiation. They are essential for protecting their health during procedures.
What are lead drapes used for in interventional pain management?
Lead drapes shield against radiation during procedures. They help reduce exposure and keep patients and providers safe.
What are some common interventional procedures for chronic pain?
Common procedures include epidural steroid injections and nerve blocks. Radiofrequency ablation, spinal cord stimulation, and joint injections are also used.
How do advanced imaging systems improve interventional procedures?
Systems like fluoroscopy and ultrasound offer real-time views. This makes procedures more precise and safe.
What is radiofrequency ablation used for in pain management?
Radiofrequency ablation uses electrical currents to heat and damage nerves. It helps relieve chronic pain.
What are the benefits of integrating R software in interventional pain management?
R software improves planning and data analysis. It helps predict outcomes, leading to better patient care and treatment success.
What are some emerging interventional procedures for chronic pain?
New procedures like kyphoplasty and MILD offer hope for chronic pain sufferers. They are part of the evolving treatment landscape.
How do interventional pain specialists select the right tools for procedures?
Specialists choose tools based on patient needs and procedure type. They aim for the best outcome.
What is the importance of proper fitting and maintenance of radiation protection aprons?
Proper fitting and care of aprons are key. They ensure healthcare workers are fully protected from radiation.
How do contrast media and medication delivery systems enhance interventional pain management?
Contrast media and delivery systems improve precision in medication. They make procedures safer and more effective.
What is the future of interventional pain management tools?
Future tools will likely include more advanced technology. This includes R software, better protection gear, and improved delivery systems. These advancements will enhance procedure safety and success.
References
Bamias, A., et al. (2017). Current clinical practice guidelines for the treatment of renal cell carcinoma: A systematic review. Cancer Treatment Reviews, 53, 107-116. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5469586






