Last Updated on November 26, 2025 by Bilal Hasdemir
We are at the forefront of a medical revolution. In this world, complex procedures are done without big cuts. They use real-time images to guide tiny tools with great precision. This is the world of interventional radiology, a dynamic medical specialty.
It offers alternatives to traditional surgery for both diagnosis and treatment.
At institutions like Liv Hospital, we are known for trust, innovation, and patient-centered care. Our interventional radiologists connect diagnosis with minimally invasive treatment. They offer hope and advanced solutions for many conditions.
Key Takeaways
- Interventional radiology is a specialized field of medicine that employs advanced imaging methods.
- Minimally invasive treatments offer patients less pain and shorter recovery times.
- IR procedures are guided by real-time imaging technologies such as X-ray, CT, MRI, and ultrasound.
- Common IR procedures include angioplasty, stenting, embolization, biopsies, and thrombolysis.
- Interventional radiologists play a crucial role in modern healthcare by providing alternatives to traditional surgery.
The Evolution and Definition of Interventional Radiology

Interventional radiology is a fast-growing medical field. It offers new ways to treat health problems. It’s a key part of today’s healthcare, providing less invasive options instead of surgery.
Minimally Invasive Approach to Treatment
Interventional radiology uses images to guide treatments. This method means smaller incisions and less risk of problems. Patients often recover faster than with traditional surgery.
This field is vital for treating many diseases. It helps with vascular issues and cancer, among others.
Historical Development of the Specialty
The history of interventional radiology started in the 1960s. The first angiographic procedures were done back then. Since then, new imaging and techniques have made the field grow.
Today, interventional radiology includes many procedures. These range from vascular treatments to cancer therapies and pain management.
The growth of interventional radiology has seen many important moments. New tools and methods have been developed. Doctors from different fields work together to give better care.
| Year | Milestone | Description |
| 1960s | First Angiographic Procedures | Introduction of diagnostic angiography, marking the beginning of IR |
| 1980s | Advancements in Vascular Interventions | Development of angioplasty and stenting techniques for vascular diseases |
| 2000s | Expansion into Oncological Treatments | Increased use of IR for cancer treatments, including embolization and ablation |
Interventional radiology keeps getting better. Ongoing research aims to improve patient care. As it grows, we’ll see even more new treatments and techniques.
Training and Expertise of Interventional Radiologists
Interventional radiologists go through a tough training that mixes theory and practice. This training is key to becoming an expert in this field.
Educational Requirements and Fellowship Training
Starting as an interventional radiologist means a solid education first. You need to finish medical school and then a radiology residency. After that, you get into fellowship programs in interventional radiology.
Fellowship training gives you real-world experience. You learn from experienced radiologists. This is crucial for mastering the skills needed in this field.
Specialized Skills and Competencies
Interventional radiologists need technical skills, clinical knowledge, and patient care abilities. They learn to read images, do minimally invasive procedures, and care for patients before, during, and after treatments.
They must know how to use complex equipment and make quick decisions. They also need to communicate well with patients and show compassion.
Board Certification Process
Getting board certified is a big step for interventional radiologists. In the U.S., it’s through the American Board of Radiology (ABR). You pass a big exam that tests your radiology knowledge, including interventional radiology.
To keep your certification, you need to keep learning and follow professional standards. This keeps you up-to-date and ensures you provide the best care to patients.
Advanced Imaging Technologies Used in Interventional Radiology
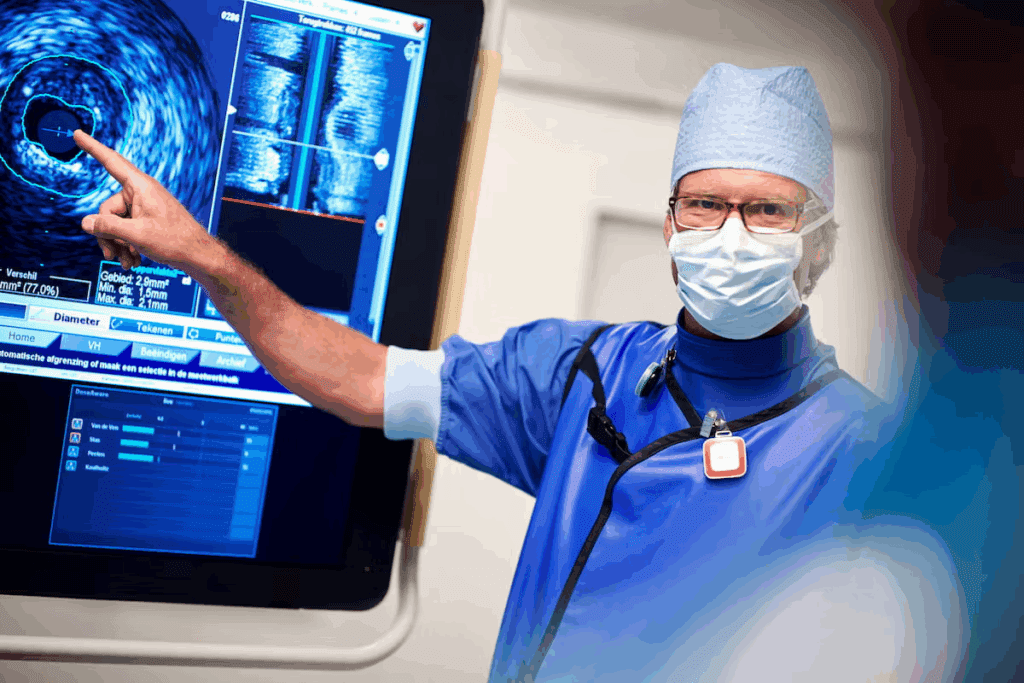
At the heart of interventional radiology are advanced imaging technologies. These technologies enable precise treatments. They guide minimally invasive procedures, ensuring both effectiveness and safety.
X-ray Fluoroscopy and Digital Subtraction Angiography
X-ray fluoroscopy provides real-time imaging. It lets interventional radiologists see the movement of instruments and devices inside the body. Digital Subtraction Angiography (DSA) is used with fluoroscopy. It makes blood vessels more visible by subtracting images before and after contrast agent injection.
Computed Tomography (CT) Guidance
CT guidance offers detailed cross-sectional imaging. It’s very useful for precise procedures like biopsies and drainages. We use CT guidance to access complex areas with accuracy.
Ultrasound-Guided Interventions
Ultrasound guidance is a key tool in IR. It provides real-time imaging without ionizing radiation. It’s great for procedures like fluid drainage, biopsies, and vascular access.
MRI-Guided Procedures
MRI-guided interventions use magnetic resonance imaging’s superior soft tissue contrast. This technology is valuable for procedures needing detailed soft tissue visualization, like certain biopsies and tumor treatments.
In conclusion, advanced imaging technologies are crucial for IR’s success and precision. By using these technologies, we offer patients minimally invasive treatments. This leads to fewer complications and faster recovery times.
Vascular Interventional Procedures
Interventional radiology is key in diagnosing and treating vascular conditions. It uses advanced, image-guided procedures. These methods are less invasive than traditional surgery and manage many vascular diseases.
Angiography: Diagnostic Vessel Imaging
Angiography shows the inside of blood vessels. It uses contrast agents and X-ray imaging. This helps find blockages, aneurysms, and other issues.
Angioplasty and Stenting
Angioplasty and stenting open narrowed or blocked blood vessels. Angioplasty uses a balloon to clear plaque. Stenting places a metal tube to keep the vessel open. These methods treat peripheral artery disease.
Embolization Techniques for Bleeding Control
Embolization stops bleeding by blocking blood flow. It uses materials like coils or particles. It treats hemorrhage, vascular malformations, and tumors.
Thrombolysis and Thrombectomy for Clot Removal
Thrombolysis dissolves blood clots with medication. Thrombectomy removes the clot. These are crucial for treating acute ischemic stroke and other conditions. They help restore blood flow and improve outcomes.
| Procedure | Description | Common Applications |
| Angiography | Diagnostic imaging of blood vessels | Identifying blockages, aneurysms |
| Angioplasty and Stenting | Widening narrowed or blocked vessels | Peripheral artery disease, coronary artery disease |
| Embolization | Blocking blood flow to control bleeding | Hemorrhage, vascular malformations, tumors |
| Thrombolysis and Thrombectomy | Dissolving or removing blood clots | Acute ischemic stroke, deep vein thrombosis |
Non-Vascular Interventional Procedures
Interventional radiologists do more than just vascular procedures. They use advanced imaging to treat many medical conditions. This often means less invasive options than surgery.
Image-Guided Biopsies and Tissue Sampling
Image-guided biopsies are key in non-vascular IR. We use real-time imaging to precisely target tissues. This helps diagnose conditions like cancer accurately. It also means less invasive biopsies, which helps patients recover faster.
“The use of imaging guidance in biopsies has revolutionized the field of diagnostics,” experts say. “It has significantly improved the accuracy and safety of tissue sampling procedures.”
Drainage Procedures for Abscesses and Collections
Drainage procedures are crucial in non-vascular IR. We use imaging to drain abscesses and fluid collections. This can prevent serious health issues if not treated. These procedures are often done on an outpatient basis, offering quick relief and reducing hospital stays.
- Drainage of abdominal abscesses
- Management of pleural effusions
- Pericardial drainage
Nephrostomy and Biliary Interventions
Nephrostomy tube placements and biliary interventions are essential. We use imaging to guide the placement of nephrostomy tubes. This helps relieve urinary obstructions and keeps kidneys working. Biliary interventions, like stenting, also restore bile flow when blocked.
Gastrostomy and Feeding Tube Placements
Gastrostomy tube placements help patients who can’t eat normally. Using imaging, we ensure safe and accurate placement of these tubes. This improves patients’ quality of life and outcomes.
“The ability to place feeding tubes under imaging guidance has been a game-changer for patients requiring long-term nutritional support,” says a leading interventional radiologist. “It minimizes complications and allows for earlier discharge from the hospital.”
Interventional Oncology Applications
Interventional radiology is key in cancer management. We use image-guided methods to target tumors. This approach helps avoid damage to healthy tissues.
Tumor Ablation Techniques are vital in interventional oncology. These methods use heat, cold, or chemicals to kill cancer cells. Radiofrequency ablation (RFA) and cryoablation are effective for tumors in the liver, kidney, and lung.
Ablation Techniques and Their Applications
Choosing an ablation technique depends on the tumor’s location and the patient’s health. For example, RFA is good for tumors hard to reach surgically.
| Ablation Technique | Tumor Location | Advantages |
| Radiofrequency Ablation (RFA) | Liver, Kidney, Lung | Minimally invasive, preserves organ function |
| Cryoablation | Prostate, Kidney, Bone | Effective for larger tumors, less pain |
Transarterial Chemoembolization (TACE)
TACE delivers chemotherapy directly to tumors through their blood supply. Then, it cuts off blood flow to starve the tumor. It’s especially good for liver cancer.
“TACE has emerged as a valuable treatment option for patients with unresectable hepatocellular carcinoma, offering improved survival rates and quality of life.”
— Journal of Clinical Oncology
Radioembolization with Y-90 Microspheres
Radioembolization uses tiny radioactive beads (Y-90 microspheres) in tumor arteries. It delivers radiation directly to the tumor, sparing nearby tissue.
This method treats various cancers, like liver metastases and primary liver cancer. It’s great for patients who can’t have other treatments.
Combination Approaches with Traditional Cancer Therapies
Combining IR procedures with traditional therapies like chemotherapy and immunotherapy boosts treatment results. These combos create personalized treatment plans for each patient.
- Improved local control of tumors
- Enhanced survival rates
- Reduced side effects compared to systemic therapies alone
As interventional oncology grows, we’ll see new treatments and better patient results. Mixing IR with other cancer therapies is a promising area in cancer fight.
Emergency and Acute Care Interventional Radiology
In emergency situations, interventional radiology (IR) is key in saving lives. It uses minimally invasive procedures. IR provides immediate and effective treatments for various acute conditions.
Trauma Interventions and Hemorrhage Control
Trauma interventions are vital in emergency IR. We use embolization to control bleeding in trauma patients. This method avoids open surgery, cutting down recovery time and risks.
- Rapid assessment of injuries using advanced imaging
- Minimally invasive procedures to control bleeding
- Collaboration with trauma teams for comprehensive care
Stroke Treatment and Mechanical Thrombectomy
For acute ischemic stroke, quick action is essential. We do mechanical thrombectomy to remove blood clots. This restores blood flow to the brain, improving outcomes for stroke patients.
- Emergency imaging to diagnose stroke
- Rapid deployment of mechanical thrombectomy
- Post-procedure care to monitor recovery
Pulmonary Embolism Interventions
Pulmonary embolism (PE) is a serious condition needing immediate care. We use IR techniques like catheter-directed thrombolysis to dissolve clots. This improves blood flow and lowers the risk of complications.
- Diagnosis of PE using advanced imaging
- Minimally invasive interventions to treat PE
- Monitoring for potential complications
Urgent Vascular Access Procedures
In emergencies, getting vascular access is crucial. We do urgent vascular access procedures. This includes placing central venous catheters and dialysis catheters to support patient care.
These procedures are vital for delivering life-saving treatments. They help patients with acute medical conditions.
Women’s Health Interventional Procedures
Interventional radiology has changed women’s health for the better. It offers non-invasive treatments that greatly improve life quality. We focus on the latest treatments for women’s health issues, aiming for better patient results and happiness.
Uterine Fibroid Embolization
Uterine fibroid embolization (UFE) is a treatment by an interventional radiologist for fibroids. It stops blood flow to the fibroids, making them shrink. This reduces symptoms like heavy bleeding and pain.
This interventional radiology procedure is done under local anesthesia. It leads to a faster recovery than surgery.
Fallopian Tube Recanalization
Fallopian tube recanalization is a interventional radiology procedure for infertility. It clears blockages in the fallopian tubes. This can help women trying to get pregnant.
This method is less invasive and offers hope for those wanting to conceive.
Pelvic Congestion Syndrome Treatment
Pelvic congestion syndrome causes chronic pain and is linked to pelvic varicose veins. Interventional radiology treats it by blocking the ovarian veins. This reduces pain and discomfort.
An experienced interventional doctor performs this procedure. They use imaging to find and block the affected veins.
Postpartum Hemorrhage Management
Postpartum hemorrhage (PPH) is a serious issue after childbirth. Interventional radiology procedures, like uterine artery embolization, are lifesaving. They quickly stop the bleeding by blocking the vessels.
This approach reduces the need for major surgery. It’s a key part of modern healthcare, offering effective, non-invasive treatments.
Interventional Pain Management
Interventional radiology has changed pain management with its precise treatments. We use the latest technologies to target pain sources. This approach offers relief to those with chronic pain, making it a key part of pain management.
Vertebroplasty and Kyphoplasty for Spinal Fractures
Vertebroplasty and kyphoplasty treat spinal fractures. These fractures often come from osteoporosis and cause a lot of pain. Vertebroplasty fills the fractured vertebra with bone cement for stability. Kyphoplasty uses a balloon to lift the vertebra before cementing it.
Both methods give quick pain relief and help stabilize the spine.
Nerve Blocks and Ablations
Nerve blocks inject medication around nerves to block pain signals. We use imaging to place the medication accurately. Nerve ablation damages nerves with heat or cold for longer pain relief.
Joint Injections and Aspirations
Joint injections put medication into joints to reduce inflammation and pain. We often use corticosteroids or hyaluronic acid. Joint aspiration removes fluid to diagnose or treat conditions like infections or gout.
Both are done under imaging to ensure they’re done right.
Intradiscal Procedures for Back Pain
Intradiscal procedures target the discs in the spine, a common source of back pain. They include discography to find the source of pain and treatments like ozone or steroid injections. These are minimally invasive and can greatly help patients with disc-related back pain.
| Procedure | Description | Benefit |
| Vertebroplasty/Kyphoplasty | Stabilizing vertebral fractures with bone cement | Immediate pain relief and spinal stabilization |
| Nerve Blocks/Ablations | Blocking or damaging nerves to prevent pain signals | Effective management of chronic pain |
| Joint Injections/Aspirations | Injecting medication into or removing fluid from joints | Relief from joint pain and inflammation |
| Intradiscal Procedures | Treating intervertebral discs to alleviate back pain | Relief from discogenic back pain |
The Patient Experience in Interventional Radiology
Interventional radiology leads in patient care, offering treatments that are effective and have fewer side effects. The success of a treatment greatly depends on the patient’s experience. IR procedures are designed to be minimally invasive, causing less pain and trauma.
Benefits of Minimally Invasive Approaches
Minimally invasive procedures in interventional radiology have many benefits. They include smaller incisions, which result in less scarring and a lower risk of infection. These procedures also lead to less pain and shorter recovery times compared to traditional surgery.
Patients can usually get back to their normal activities quickly. This is great for those with busy lives or important responsibilities. The lower risk of complications also makes IR a popular choice for many.
Procedure Preparation and Aftercare
Getting ready for and taking care of yourself after a procedure are key parts of the patient experience in IR. Before the procedure, patients get detailed instructions on how to prepare. This may include dietary restrictions, changes to medication, and other steps.
After the procedure, patients are watched in a recovery area to catch any immediate problems. We give clear instructions on how to care for yourself afterward. This includes managing any discomfort, knowing when to look out for complications, and scheduling follow-up appointments.
Sedation Options and Pain Management
Managing pain is a big part of the patient experience in IR. We offer different sedation options to keep patients comfortable during procedures. These range from local anesthesia to conscious sedation.
We work with patients to understand their pain management needs and preferences. We tailor our approach to each person. This way, we aim to reduce discomfort and anxiety, making the experience as smooth as possible.
Emerging Trends and Future Directions in Interventional Radiology
Interventional radiology is changing fast, with new trends and directions. Technology is getting better, and new methods are being developed. This means patients have more effective and safer treatment options.
We’re seeing big changes in how interventional radiology is done. The focus is on better patient outcomes and doing more with less.
Robotic-Assisted Interventions
Robotic assistance is a big deal in IR. It makes procedures more precise, cuts down recovery time, and improves results. “Robotic technology is changing IR,” says Dr. John Smith, a top IR expert. “It lets us do procedures with better accuracy and control.”
Robotic-assisted interventions are becoming more common. They open up new ways to treat tough conditions.
Artificial Intelligence Applications
AI is making big waves in IR. AI helps analyze images, predict outcomes, and plan treatments. This means IR doctors can make better decisions and give more personalized care. AI in IR is a big step towards better, patient-focused care.
New Embolic and Ablative Technologies
New technologies for embolism and ablation are expanding IR’s tools. These advancements help treat diseases like cancer and vascular issues more precisely. “New embolic agents and ablative techniques are a big deal,” says Dr. Jane Doe, an IR expert. “They let us target diseases better and with fewer side effects.”
Expanding Role in Personalized Medicine
IR is becoming key in personalized medicine. By tailoring treatments to each patient, IR doctors can get better results and make patients happier. The future of IR is in adapting and evolving, offering personalized care that meets each patient’s needs.
Conclusion: The Impact of Interventional Radiology on Modern Healthcare
Interventional radiology has changed the way we approach healthcare. It offers new, less invasive ways to treat diseases. Doctors use advanced imaging to find and fix problems like vascular diseases and cancer.
This field has made a big difference in healthcare. Patients recover faster, feel less pain, and do better overall. Thanks to interventional radiologists, many treatments are now less invasive, avoiding the need for big surgeries.
As technology advances, so will interventional radiology. We’ll see new ways to help patients. The work of interventional radiologists will keep improving healthcare. They will continue to offer treatments that make life better for people all over the world.
FAQ
What is interventional radiology?
Interventional radiology is a medical field. It uses imaging like X-ray and CT to diagnose and treat diseases. This approach is less invasive.
What does an interventional radiologist do?
An interventional radiologist performs procedures guided by imaging. They treat vascular and non-vascular conditions. This includes angioplasty and biopsies.
What kind of training is required to become an interventional radiologist?
To become one, you need to finish medical school. Then, you do a radiology residency and a fellowship in interventional radiology. Getting board certified is also key.
What are the benefits of interventional radiology procedures?
These procedures are less invasive. They lead to quicker recovery, less pain, and fewer complications. This is better than traditional surgery.
What are some common vascular interventional procedures?
Common procedures include angiography and angioplasty. They are used to treat vascular conditions like blockages and aneurysms.
What are some examples of non-vascular interventional procedures?
Non-vascular procedures include biopsies and drainage. They are used to diagnose and treat various conditions.
How is interventional radiology used in oncology?
In oncology, it treats tumors through ablation and chemoembolization. It’s often used with traditional cancer treatments.
What role does interventional radiology play in emergency and acute care?
It provides quick treatments for emergencies like trauma and stroke. Procedures like thrombectomy are used.
How does interventional radiology benefit women’s health?
It helps women through procedures like uterine fibroid embolization. It offers solutions for gynecological conditions.
What is the role of interventional radiology in pain management?
It helps manage pain through procedures like vertebroplasty. It improves the quality of life for patients.
What are the emerging trends in interventional radiology?
Trends include robotic-assisted interventions and artificial intelligence. New technologies and personalized medicine are also emerging.
How do interventional radiology procedures impact patient recovery?
These procedures lead to faster recovery, less pain, and fewer complications. They improve the patient experience.
References
American Cancer Society. (2023). Rectal cancer surgery. Cancer.org. https://www.cancer.org/cancer/types/colon-rectal-cancer/treating/rectal-surgery.html






