Last Updated on November 25, 2025 by Ugurkan Demir

Atrial fibrillation (AFib) is a common heart rhythm problem. It makes the heart beat fast and irregularly. At Liv Hospital, we focus on top-notch healthcare for patients from around the world.Discover 4 key features of A Fib EKG patterns and how they help in diagnosing atrial fibrillation accurately.
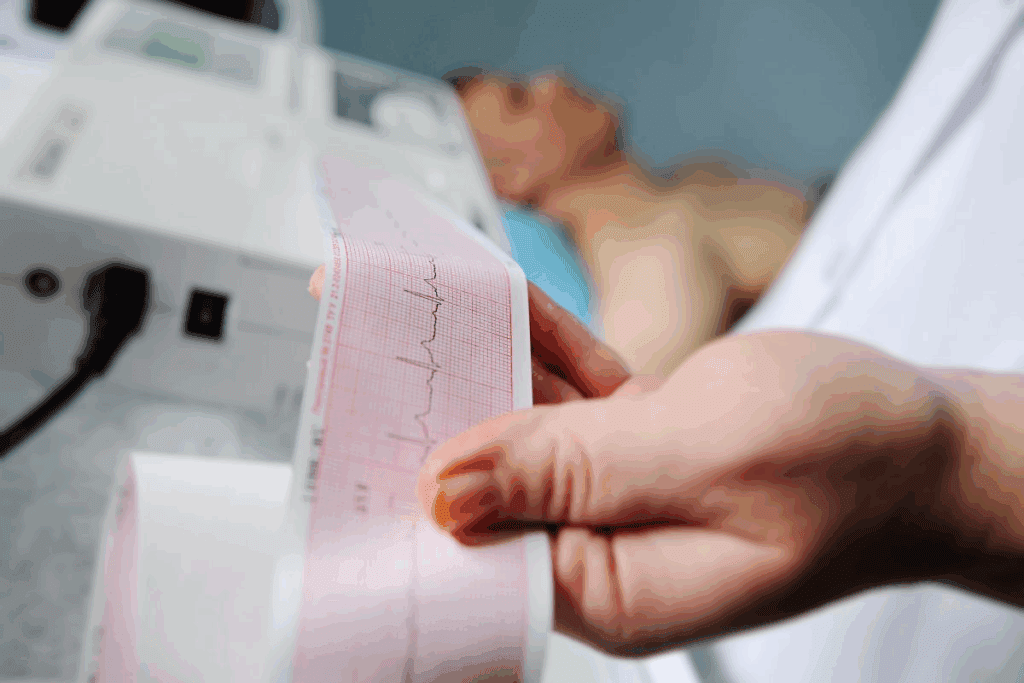
Getting AFib right on an ECG is key for good care. The ECG for AFib looks different because it’s not regular. It also doesn’t have the usual P waves. We’re all about putting patients first and using the latest medical knowledge to manage AFib well.
Atrial fibrillation (AFib) is a common heart rhythm disorder affecting millions. It happens when the heart’s upper chambers get chaotic electrical signals. This can lead to an irregular heartbeat, affecting how well the heart works and increasing the risk of blood clots.
AFib disrupts the heart’s normal electrical activity in the atria. The electrical signals in the upper chambers are chaotic. This means the AV node can’t stop all these signals from reaching the lower chambers. This results in a fast and irregular heartbeat.
Key factors contributing to the pathophysiology of AFib include:
The irregular and rapid heartbeat in AFib can harm the heart. The loss of coordinated atrial contractions reduces ventricular filling. This can lead to a decrease in cardiac output, which is worse in patients with heart disease.
The hemodynamic consequences of AFib can include:
Understanding AFib’s pathophysiology and hemodynamic impact is key to managing it. Clinicians must consider these factors when treating AFib patients. This helps improve outcomes and reduce complications.
Understanding AFib EKGs is key for clinicians. They need to know the basics of ECG interpretation to spot atrial fibrillation. We’ll cover the essential knowledge they must have.
ECG interpretation is a must-have skill for doctors. Knowing the basics is vital. It involves looking at the heart’s electrical activity on the ECG machine. Accurate lead placement is essential for good data.
The ECG shows the heart’s rhythm, rate, and electrical activity. Clinicians should look for signs of atrial fibrillation. This includes an irregular rhythm and no P waves.
| ECG Feature | Normal Sinus Rhythm | Atrial Fibrillation |
| Rhythm | Regular | Irregularly Irregular |
| P Waves | Present | Absent |
| Fibrillatory Waves | Absent | Present |
Right equipment and lead placement are key for accurate ECGs. The 12-lead ECG is often used for atrial fibrillation diagnosis. Lead placement must follow guidelines for accurate readings.
When doing an ECG, correct lead placement is critical. Wrong placement can lead to errors or misreads.
By grasping ECG basics and ensuring proper equipment and lead placement, clinicians can accurately diagnose atrial fibrillation. This knowledge is vital for effective patient care.
Atrial fibrillation on an ECG is known for its irregularly irregular rhythm. This is what sets it apart from other heart rhythm problems. The ECG shows this by the changing R-R intervals.
In atrial fibrillation, the R-R intervals change because the heart’s rhythm is unpredictable. This makes the heart’s beat irregular. Here are some important points to understand:
Irregularly irregular rhythm is a term used to describe this unique characteristic of AFib on ECG. It is a critical feature that helps differentiate AFib from other types of arrhythmias.
While other arrhythmias may have irregular rhythms, AFib’s rhythm is unique. To tell AFib apart from other irregular rhythms, we look for:
By examining these features, doctors can accurately diagnose atrial fibrillation on an ECG. The irregularly irregular rhythm is a key sign.
Atrial fibrillation, the most common sustained arrhythmia, is characterized by four key ECG features that we will explore in detail. These features are critical for accurate diagnosis and management of this condition.
The four key features include an irregularly irregular rhythm, the absence of P waves, fibrillatory baseline waves, and a variable ventricular response rate. Understanding these characteristics is essential for clinicians to diagnose and manage atrial fibrillation effectively.
To better understand how these features manifest on an ECG, let’s examine a comparison of normal sinus rhythm and atrial fibrillation characteristics:
| ECG Feature | Normal Sinus Rhythm | Atrial Fibrillation |
| Rhythm | Regular | Irregularly Irregular |
| P Waves | Present and consistent | Absent |
| Baseline | Isoelectric | Fibrillatory waves |
| Ventricular Rate | Typically 60-100 bpm | Variable, often rapid |
This comparison highlights the distinct differences between a normal heart rhythm and atrial fibrillation on an ECG. It shows why recognizing these key features is vital for accurate diagnosis.
Atrial fibrillation (AFib) is marked by the lack of P waves on an electrocardiogram (ECG). P waves usually show the electrical activity of the atria before the heart beats. But in AFib, the chaotic signals in the atria mean no clear P waves are seen.
In a normal heartbeat, P waves are seen in lead II and show how the atria depolarize. The regularity of P waves is key to diagnosing a normal heart rhythm. The shape of P waves tells us about how the atria depolarize.
P waves start the contraction of the atria. They are small deflections on the ECG before the QRS complex. This shows the atria are depolarizing.
The lack of P waves in AFib is a key sign that sets it apart from other heart rhythms. This is because the atria’s electrical activity is chaotic and disorganized. This sign helps doctors tell AFib apart from other conditions.
When looking at an ECG for AFib, doctors check for the absence of P waves among other signs. These signs together give a full picture of the heart’s rhythm.
Knowing about the absence of P waves in AFib is vital for correct diagnosis and treatment. It helps doctors manage patients with AFib better.
Atrial fibrillation is marked by fibrillatory baseline waves. These waves show the chaotic electrical activity in the atria. They are key to diagnosing atrial fibrillation and distinguishing it from other heart rhythm issues.
Fibrillatory waves, or f-waves, on an ECG look like a wavy or undulating baseline. To spot f-waves, look for these signs:
Leads V1 and V2 are best for spotting f-waves because they’re close to the atria.
Fibrillatory waves can look different from one patient to another and even change in the same patient over time. Some common differences include:
Knowing about these differences is key to accurately diagnosing atrial fibrillation with an ECG. By recognizing the various ways fibrillatory waves can appear, doctors can better detect and manage this common heart rhythm problem.
Atrial fibrillation (AFib) is known for its variable ventricular response rate. This rate can greatly affect how patients feel and how they are treated. It’s a big challenge for doctors to find the right treatment.
The heart rate in AFib can be slow or very fast. A controlled ventricular rate is between 60 to 100 beats per minute (bpm). An uncontrolled rate is over 100 bpm, sometimes reaching 150 bpm or more.
Having a controlled rate means a patient might not feel symptoms or only feel a little bit of them. But, an uncontrolled rate can cause serious symptoms like palpitations, shortness of breath, and tiredness.
Many things can change the ventricular response rate in AFib, including:
Knowing these factors is key to managing AFib well. By controlling the ventricular rate, doctors can help patients feel better, live better, and avoid serious problems.
Being able to spot atrial fibrillation on an ECG is key for correct diagnosis and care. Atrial fibrillation (AFib) is the most common lasting heart rhythm problem. Doctors use ECGs to figure out if someone has AFib.
Classic AFib ECGs show an irregularly irregular rhythm. They don’t have P waves and have fibrillatory waves instead. The heart rate can be slow or fast, which helps doctors tell it’s AFib.
In a typical AFib ECG, the fibrillatory waves look different in size and speed. This makes the ECG look chaotic. This is unlike atrial flutter, where the heart’s activity is more regular.
While classic AFib ECGs are clear, some cases are harder to spot. These tricky cases might have waves that are hard to see or don’t look right. This makes diagnosing AFib a bit tougher.
It’s important to know how to spot these tricky cases. This helps doctors give the right treatment to patients with atrial fibrillation.
Distinguishing atrial fibrillation on an ECG from a normal sinus rhythm is key for patient care. Atrial fibrillation (AFib) shows an irregular rhythm, no P waves, and a changing heart rate. These are different from a normal heart rhythm.
A normal heart rhythm has a steady beat, usually between 60-100 beats per minute. It has a consistent PR interval and P waves before each QRS complex. The P wave is usually upright in certain leads, showing normal heart function.
Key features of normal sinus rhythm include:
Looking at atrial fibrillation ECGs and normal sinus rhythm shows what makes AFib different. The table below highlights the main differences:
| Characteristic | Normal Sinus Rhythm | Atrial Fibrillation |
| Rhythm | Regular | Irregularly irregular |
| P Waves | Present before each QRS | Absent; replaced by fibrillatory waves |
| PR Interval | Consistent | Variable; not measurable |
| Ventricular Rate | 60-100 bpm | Variable; often rapid |
Knowing these differences is vital for accurate diagnosis and treatment. By spotting the signs of atrial fibrillation on an ECG and comparing them to normal rhythm, doctors can better care for their patients.
Atrial fibrillation (AFib) detection and monitoring are key parts of patient care. They need precise lead placement and constant watch. We use electrocardiogram (ECG) monitoring to spot AFib’s unique signs. This is important for making treatment plans and better patient results.
Getting leads in the right spot is key for catching AFib’s chaotic heart activity. We put electrodes on the chest and limbs to get a full view of the heart’s activity. This helps us see AFib clearly.
By placing leads carefully, doctors can watch AFib better. For example, leads in the precordial area can catch the fibrillatory waves of AFib. This makes detecting AFib more accurate.
Keeping an eye on AFib is vital for managing it. We use Holter monitors, implantable loop recorders, and remote monitoring systems for this. These tools help us watch AFib closely.
These methods let doctors track AFib changes and see if treatments work. They help make better care plans. Using these technologies can also lower the risk of AFib problems.
Good AFib monitoring also means teaching patients about their condition. When patients know what’s going on, they can help with their care. They can report symptoms and follow monitoring plans.
Advanced ECG analysis is changing how we diagnose and manage atrial fibrillation. It helps doctors understand the condition better. This leads to better care for patients.
Computer-assisted ECG interpretation is a big help in cardiology. It uses smart algorithms to make ECG analysis more accurate and quick. This tool helps spot atrial fibrillation and understand its risks.
Benefits of Computer-Assisted ECG Interpretation:
New ECG parameters are being studied to measure atrial fibrillation’s severity. These include atrial fibrillatory frequency, heart rate variability, and more.
| ECG Parameter | Description | Clinical Significance |
| Fibrillatory Frequency | Measures the frequency of atrial fibrillatory waves | Indicates AFib severity and possible thromboembolic risks |
| Heart Rate Variability | Looks at the change in ventricular response rate | Helps decide on rate control treatments |
Using these advanced ECG analysis methods in practice can greatly improve atrial fibrillation management. It leads to more accurate diagnoses, better risk assessment, and personalized treatments.
Atrial fibrillation ECG findings have big impacts on patient care and treatment results. The info from ECG analysis is key for deciding on treatment and risk levels.
We use ECG findings to sort patients by their risk of stroke and other issues. Important ECG signs that help us include:
By looking at these ECG signs, we can spot patients at higher risk. They might need more intense treatment plans.
The choice of treatment for atrial fibrillation depends a lot on ECG findings. We look at several things when picking a treatment:
By carefully looking at ECG findings, we can make treatment plans that are just right for each patient.
Getting atrial fibrillation (AFib) right means knowing how to read ECGs well. We’ve looked at what makes an AFib ECG stand out. This includes an irregular rhythm, no P waves, and different heart rates.
Learning to spot these signs is key to treating AFib right. At Liv Hospital, we focus on top-notch care for international patients. Our team is skilled in diagnosing and treating AFib.
Understanding ECGs is vital for managing AFib. When healthcare pros get good at reading these tests, they can make better choices. This leads to better health and happiness for those with AFib.
Atrial fibrillation on an ECG shows an irregular rhythm. It lacks distinct P waves and has fibrillatory waves. The ventricular response rate also varies.
Atrial fibrillation can harm the heart’s function and blood flow. It might lower the heart’s output and increase the risk of blood clots. This is due to the heart’s irregular and fast beats.
Proper lead placement is key for spotting AFib’s signs on an ECG. It helps doctors to manage and detect the condition well.
AFib shows an irregular rhythm and no clear P waves on an ECG. Normal sinus rhythm, on the other hand, has a regular rhythm and clear P waves before each QRS complex.
Fibrillatory waves, or f-waves, show the atria’s chaotic electrical activity. They can look different on an ECG, sometimes being hard to spot.
Doctors tell AFib apart from other irregular rhythms by looking at the ECG. They look for the irregular rhythm and no P waves.
The lack of P waves is a key sign of AFib. It shows the atria’s chaotic activity. This is important for diagnosing AFib and differentiating it from other heart issues.
New ECG analysis methods help better diagnose and manage AFib. They include computer-assisted readings and new ECG markers. These tools guide treatment and improve patient care.
ECG findings in AFib are very important. They help doctors figure out the risk and choose the right treatment. This includes checking for stroke risk and picking the best treatment options.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!