
Learn about aortoiliac atherosclerosis, its main causes, symptoms, and treatment options explained clearly.
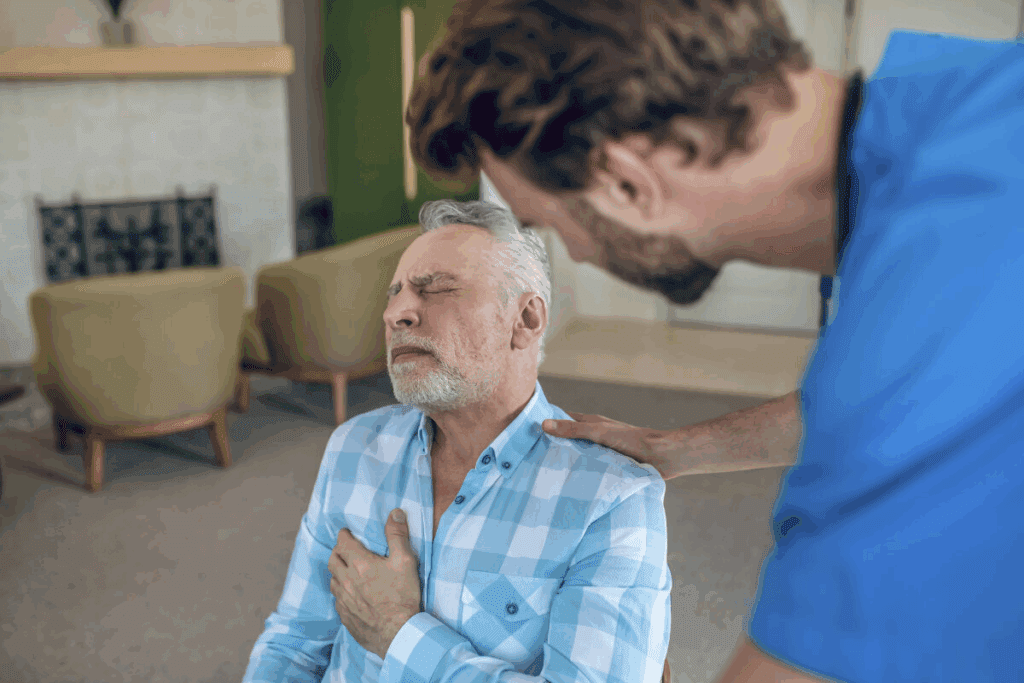
Aortoiliac atherosclerosis is a condition that affects the arteries in the lower part of the body. It can lead to reduced blood flow to the legs. At Liv Hospital, we know how much this condition can affect a person’s life.
Reduced blood flow can cause pain in the legs when walking or exercising. If not treated, it can lead to serious problems.
We offer effective treatments for this condition. These include lifestyle changes, medication, endovascular procedures, and surgery.
Key Takeaways
- Aortoiliac atherosclerosis is a form of peripheral artery disease that affects blood flow to the legs.
- Symptoms include leg pain when walking or exercising.
- Effective management can significantly improve quality of life.
- Treatment options range from lifestyle changes to surgery.
- Consult a healthcare professional for proper diagnosis and treatment.
Aortoiliac Atherosclerosis: Definition and Overview

Aortoiliac atherosclerosis is a condition where the abdominal aorta and iliac arteries narrow or block. This happens because of plaque buildup. It can cause reduced blood flow to the lower body, leading to symptoms.
What Happens in the Arteries
In aortoiliac atherosclerosis, the arteries narrow or block due to plaque. This plaque is made of fat, cholesterol, and other substances. As it builds up, it can harden and limit blood flow, causing pain during activity.
Prevalence and Demographics
This condition mainly affects older adults. The risk increases with age. About 3-14% of people are affected, rising to 14-20% in those over 70 and up to 23% in those over 80.
| Age Group | Prevalence |
| 50-59 | 3-5% |
| 60-69 | 8-12% |
| 70+ | 14-23% |
Types: Mild to Severe
Aortoiliac atherosclerosis can range from mild to severe. The severity depends on how much plaque builds up and how much the arteries narrow or block. Mild cases might not show symptoms, but severe cases can greatly affect quality of life.
Anatomy and Function of the Aortoiliac Region
The aortoiliac region is key for blood flow to the lower legs. It includes the abdominal aorta and iliac arteries. These parts are vital for blood to reach the legs.
The Abdominal Aorta Structure
The abdominal aorta runs through the belly. It starts from the thoracic aorta and goes through the diaphragm. It then splits into the common iliac arteries near the fourth lumbar vertebra (L4).
The aorta’s wall has three layers: intima, media, and adventitia. The intima is the innermost, the media has smooth muscle and elastic fibers, and the adventitia is the outermost layer.
Iliac Arteries and Their Branches
The common iliac arteries split into internal and external iliac arteries. The internal iliac arteries go to the pelvic organs. The external iliac arteries lead to the lower limbs.
The iliac arteries are important for blood to the lower legs. Problems with these arteries can cause serious issues.
Normal Blood Flow Patterns
Blood flow in the aortoiliac region is laminar, or in parallel layers. This flow is efficient and saves energy.
In a healthy person, blood flow starts fast in systole and slows down in diastole. Knowing this flow pattern helps in diagnosing and treating vascular diseases.
Pathophysiology of Aortoiliac Atherosclerotic Disease
Aortoiliac atherosclerotic disease is a complex condition. It involves many factors that lead to plaque buildup in the arteries. This affects blood flow in the aortoiliac area.
Plaque Formation and Progression
Plaque formation is key in aortoiliac atherosclerosis. It starts with LDL cholesterol buildup in the artery walls. This buildup causes inflammation and attracts macrophages.
The plaque grows over time. It includes smooth muscle cells, inflammatory cells, and calcium. This growth narrows the artery, reducing blood flow.
Aortoiliac Atherosclerotic Calcification Process
Calcification is a sign of advanced disease. It happens when calcium salts deposit in the plaque. This makes the arteries stiffer and complicates the disease.
Calcification makes arteries stiffer and less flexible. It raises the risk of heart problems. Factors like inflammation and certain minerals play a role in calcification.
Vascular Remodeling and Narrowing
Vascular remodeling changes the artery structure due to disease. In aortoiliac atherosclerosis, it can cause significant narrowing. This reduces blood flow to the legs.
This narrowing can cause pain and other symptoms. The severity and progression vary. Factors like smoking and diabetes play a role.
Risk Factors and Causes
It’s important to know the risk factors for aortoiliac atherosclerosis to prevent and manage it. This condition is caused by plaque buildup in the aorta and iliac arteries. It’s influenced by several factors, including things we can change and things we can’t.
Modifiable Risk Factors
Modifiable risk factors are things we can change. They include:
- Smoking: Smoking speeds up plaque formation by causing inflammation and damage to the arteries.
- Hypertension: High blood pressure can damage the arteries, making them more likely to develop plaque.
- Hyperlipidemia: High cholesterol and triglycerides can lead to atherosclerotic plaques.
- Diabetes: Diabetes increases the risk of atherosclerosis due to metabolic changes.
Changing these risk factors through lifestyle changes and medical treatment can slow down aortoiliac atherosclerosis.
Non-Modifiable Risk Factors
Non-modifiable risk factors are things we can’t change. They include:
- Age: The risk of aortoiliac atherosclerosis goes up with age.
- Family History: A family history of heart disease can increase the risk.
- Genetic Predisposition: Some genetic factors can affect the development of atherosclerosis.
Knowing these non-modifiable risk factors helps in assessing risk and planning management strategies.
Comorbid Conditions
Comorbid conditions can make managing aortoiliac atherosclerosis harder. Common ones include:
| Comorbidity | Impact on Aortoiliac Atherosclerosis |
| Chronic Kidney Disease | Increases cardiovascular risk and complicates management |
| Heart Disease | Can coexist with aortoiliac atherosclerosis, requiring more complex care |
| Peripheral Artery Disease | Often associated with aortoiliac atherosclerosis, indicating widespread atherosclerotic disease |
Managing comorbid conditions is key to improving outcomes in aortoiliac atherosclerosis.
Clinical Presentation and Symptoms
The symptoms of aortoiliac atherosclerosis vary a lot. Some people have no symptoms at all. Others face severe problems that could harm their limbs. It’s key to know these signs to get help early.
Early Symptoms and Warning Signs
Early signs include intermittent claudication. This is pain or cramping in the legs when you exercise. It goes away when you rest.
People might also feel tired, pain, or cramping in their buttocks, thighs, or calves. This happens when they walk.
Intermittent Claudication
Intermittent claudication is a big warning sign. It happens when blood flow to muscles is low during exercise. The pain goes away when you rest.
Advanced Symptoms in Severe Cases
As the disease gets worse, symptoms get more serious. Rest pain is one sign. It happens even when you’re not moving, showing the disease is advanced.
Complications of Untreated Disease
If not treated, aortoiliac atherosclerosis can cause big problems. Gangrene or lower limb ulcers can happen. Knowing these risks shows why early treatment is so important.
Diagnostic Approaches and Testing
To accurately diagnose aortoiliac atherosclerosis, healthcare professionals use many tools. These range from initial checks to advanced imaging.
Clinical Evaluation and Physical Examination
The first step is a detailed clinical evaluation and physical exam. This is key to spotting at-risk patients and deciding on further tests.
Clinical history taking is vital. It helps identify risk factors and symptoms linked to aortoiliac atherosclerosis.
A physical exam might show signs like weak pulses in the legs or sounds in the belly. These signs point to blocked arteries.
Non-Invasive Vascular Testing
Non-invasive vascular tests are critical in diagnosing aortoiliac atherosclerosis. They give important info about arterial disease without invasive methods.
- Ankle-Brachial Index (ABI): A simple test that compares blood pressure in the ankles and arms.
- Doppler Ultrasound: Uses sound waves to check blood flow in arteries, spotting blockages.
Advanced Imaging Techniques
Advanced imaging is used for a detailed look. It shows the exact state of the arteries and disease extent.
Computed Tomography Angiography (CTA) and Magnetic Resonance Angiography (MRA) are used. They provide detailed images for treatment planning.
Classification Systems and Staging
After diagnosis, aortoiliac atherosclerosis is classified and staged. This is based on disease severity. It helps choose the best treatment.
| Classification | Description | Treatment Approach |
| Mild | Minimal symptoms, slight arterial narrowing | Conservative management, lifestyle modifications |
| Moderate | Noticeable symptoms, significant arterial stenosis | Pharmacological treatment, possible endovascular intervention |
| Severe | Significant symptoms, substantial arterial obstruction | Surgical or endovascular revascularization |
Classifying and staging aortoiliac atherosclerosis is key. It guides treatment and predicts outcomes.
Conservative Management Strategies
Conservative management strategies are key in treating aortoiliac atherosclerosis. They aim to reduce symptoms, enhance quality of life, and stop the disease from getting worse. We will look at the main parts of conservative management.
Lifestyle Modifications
Lifestyle changes are vital in managing aortoiliac atherosclerosis. Smoking cessation is a must, as smoking speeds up atherosclerosis. Patients are urged to join exercise programs to boost circulation and heart health.
They are also advised to make dietary changes. This means eating a diet rich in fruits, vegetables, and whole grains, but low in saturated fats.
Pharmacological Treatments
Pharmacological treatments are essential in managing aortoiliac atherosclerosis. Antiplatelet agents help prevent blood clots. Statins are used to lower cholesterol, reducing artery plaque buildup.
Other medicines may be given to control hypertension, hyperlipidemia, and diabetes. These conditions increase the risk of atherosclerosis getting worse.
Managing Comorbidities
Managing comorbidities is critical in treating aortoiliac atherosclerosis. Patients with conditions like diabetes, hypertension, and hyperlipidemia need close monitoring. This helps prevent complications.
Effective management of comorbidities can greatly improve life quality. It also lowers the risk of the disease getting worse.
Interventional and Surgical Treatments
Interventional and surgical treatments offer many options for those with aortoiliac atherosclerosis. These methods aim to improve blood flow and reduce symptoms. They help patients live better lives.
Endovascular Procedures
Endovascular procedures are less invasive. They include angioplasty and stenting. These methods widen narrowed arteries and keep them open.
Angioplasty uses a balloon to push plaque against the artery walls. This improves blood flow. Stenting is often used with angioplasty to keep the artery open.
Open Surgical Options
For some, open surgical options are better. Aortobifemoral bypass is a common surgery. It bypasses the diseased parts of the aorta and iliac arteries with a graft.
This surgery can last a long time and is often suggested for severe cases.
Hybrid Approaches
Hybrid approaches mix endovascular and open surgery. They offer a customized treatment for complex cases. Hybrid methods combine the best of both worlds for better results.
Choosing the Right Procedure
Choosing the right treatment depends on several factors. These include disease severity, overall health, and anatomy. A vascular specialist must evaluate each case carefully.
We work with patients to understand their needs. We create a treatment plan that fits their situation and preferences.
Conclusion: Prognosis and Long-term Management
The outlook for those with aortoiliac atherosclerosis depends on the disease’s severity, treatment success, and how well patients follow advice. Keeping up with treatment and lifestyle changes is key. This ensures ongoing care and adjustments as needed.
Patients can improve their health and life quality by understanding their disease. A team approach is vital for managing aortoiliac atherosclerosis. This focuses on better treatment results.
Keeping the blood vessels healthy is essential for long-term management. Regular check-ups and managing risk factors are critical. These steps help prevent the disease from getting worse.
FAQ
What is aortoiliac atherosclerosis?
Aortoiliac atherosclerosis is a condition where the abdominal aorta and iliac arteries narrow or block. This happens due to plaque buildup. It reduces blood flow to the lower legs.
What are the risk factors for developing aortoiliac atherosclerosis?
Risk factors include smoking, high blood pressure, high cholesterol, and diabetes. Age, family history, and genetics also play a role.
What are the symptoms of aortoiliac atherosclerosis?
Symptoms range from pain or cramping in the legs during exercise to more severe symptoms. These include rest pain and tissue loss in advanced cases.
How is aortoiliac atherosclerosis diagnosed?
Diagnosis involves clinical evaluation and non-invasive tests like ABI and Doppler ultrasound. Advanced imaging like CTA and MRA are also used.
What are the treatment options for aortoiliac atherosclerosis?
Treatment includes lifestyle changes and medications. It also includes endovascular procedures and open surgery.
What is the prognosis for patients with aortoiliac atherosclerosis?
Prognosis depends on disease severity, treatment success, and patient adherence to treatment plans.
Can aortoiliac atherosclerosis be prevented?
While some risk factors are unchangeable, managing modifiable ones can prevent or slow the disease.
How is aortoiliac atherosclerosis related to peripheral artery disease (PAD)?
Aortoiliac atherosclerosis is a form of PAD. It involves narrowing or blockage of peripheral arteries, reducing blood flow to the lower extremities.
What is the role of lifestyle modifications in managing aortoiliac atherosclerosis?
Lifestyle changes like quitting smoking, exercising regularly, and eating healthy are key. They help manage the condition and prevent it from getting worse.
What are the possible complications of untreated aortoiliac atherosclerosis?
Untreated aortoiliac atherosclerosis can lead to severe complications. These include limb ischemia, gangrene, and cardiovascular events.
References
- Rau, C., & Joshi, P. H. (2024). Objective Methods to Assess Aorto-Iliac Calcifications: A Systematic Review. Frontiers in Cardiovascular Medicine, 11, 1234567. from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11119820/




































