Learn the arteriosclerosis definition, its causes, symptoms, and how it affects blood vessels.
Arteriosclerosis is when the arteries get hard. This can cause serious heart problems. We will look into what arteriosclerosis is and how it affects the body.
This term covers several types, like atherosclerosis and arteriolosclerosis. Knowing the causes, symptoms, and treatments for arteriosclerosis is key to keeping your heart healthy.
Key Takeaways
- Arteriosclerosis is a broad term describing the hardening of arteries.
- The condition can lead to various cardiovascular complications.
- Understanding the causes and symptoms is key for early detection.
- Modern treatments offer hope for managing arteriosclerosis and related heart disease.
- Liv Hospital provides the latest expertise and caring for arteriosclerosis.
Arteriosclerosis Definition: Understanding the Condition

Arteriosclerosis is a group of conditions that harden and lose elasticity in arteries. It includes many different changes that affect how arteries work.
The Pathophysiology of Arterial Hardening
Arterial hardening comes from complex changes in cells and molecules. Important factors are inflammation, damage to the inner lining of arteries, and buildup of lipids and calcium. These changes make arteries less flexible and harder to move blood through.
Looking into arteriosclerosis shows it’s caused by many things. Genetics, lifestyle, and the environment all play a role in how it develops and grows.
Arteriosclerosis vs. Atherosclerosis: Important Distinctions
Arteriosclerosis and atherosclerosis are often confused, but they’re not the same. Atherosclerosis is when plaques build up inside arteries. Arteriosclerosis is a wider term that includes hardening of arteries, like arteriolosclerosis and vascular sclerosis.
- Atherosclerosis involves plaque formation and lipid accumulation.
- Arteriolosclerosis affects the small arteries and arterioles.
- Vascular sclerosis refers to the hardening of blood vessels.
Types of Arteriosclerosis and Their Characteristics

Arteriosclerosis comes in several forms, each with its own traits and health impacts. Knowing these differences is key for the right diagnosis and treatment.
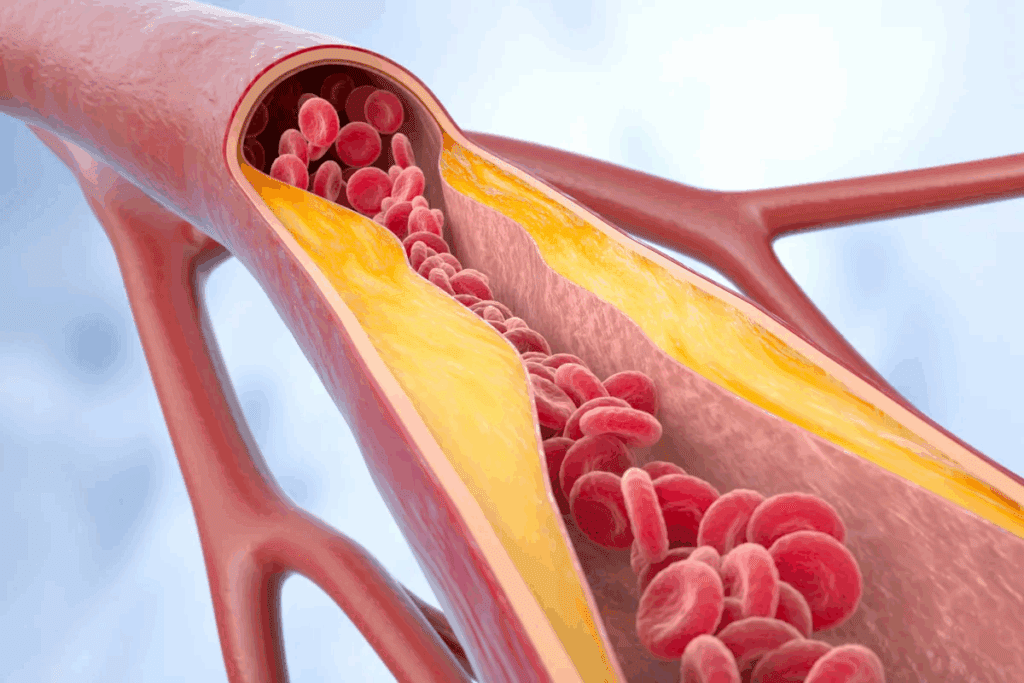
Atherosclerosis: Plaque Buildup in Arteries
Atherosclerosis is the most common arteriosclerosis type. It’s marked by plaque buildup in artery walls. This plaque is made of fat, cholesterol, calcium, and blood substances. Over time, it can harden or burst, causing blood clots that block blood flow.
Key features of atherosclerosis include:
- Plaque buildup in large and medium-sized arteries
- Risk factors such as high cholesterol, hypertension, and smoking
- Potential complications like heart attack and stroke
Arteriolosclerosis: Small Artery Thickening
Arteriolosclerosis is when arteriole walls thicken. This can cut down blood flow to important organs. It’s often linked to high blood pressure and diabetes.
Characteristics of arteriolosclerosis:
- Thickening of arteriolar walls
- Association with hypertension and diabetes
- Potential impact on kidney function and other organs
Vascular Sclerosis and Arthrostenosis
Vascular sclerosis is a term for different arteriosclerosis types, including medial arterial calcification. Arthrostenosis, while not a direct arteriosclerosis type, refers to joint stiffening. Yet, in vascular health, it’s sometimes linked to blood vessel stiffening or narrowing.
The table below outlines the main arteriosclerosis types and their characteristics:
| Type | Characteristics | Risk Factors |
| Atherosclerosis | Plaque buildup in large and medium-sized arteries | High cholesterol, hypertension, smoking |
| Arteriolosclerosis | Thickening of arteriolar walls | Hypertension, diabetes |
| Medial Arterial Calcification | Calcification of the medial layer of arteries | Age, diabetes, kidney disease |
Knowing these types is vital for creating effective treatment plans and managing the condition well.
What Causes Arteriosclerosis Disease?
Arteriosclerosis is caused by many risk factors. Some can be changed through lifestyle. Knowing these factors is key to preventing and managing the disease.
Modifiable Risk Factors
Several risk factors can be changed. These include high cholesterol, hypertension, diabetes, smoking, and obesity. By controlling these, people can lower their risk of arteriosclerosis.
High cholesterol causes plaque buildup in arteries, making them hard and narrow. Hypertension strains the arteries, speeding up hardening. Diabetes damages blood vessels and nerves that control the heart.
- Smoking: Damages the inner lining of blood vessels, making them more susceptible to blockage.
- Obesity: Often associated with other risk factors like high blood pressure, diabetes, and high cholesterol.
Non-Modifiable Risk Factors
Some risk factors can’t be changed, but knowing them is important. Age is a big risk factor, as arteriosclerosis risk grows with age. Family history also matters; those with a family history are more likely to get it.
Also, genetic predispositions affect how the body handles lipids and responds to risks. Knowing these helps in making a prevention plan that fits you.
Signs and Symptoms of Arteriosclerosis
Arteriosclerosis often starts quietly, but knowing its signs is key. As it gets worse, symptoms can show up. These depend on the arteries and how severe the disease is.
Early Warning Signs and Mild Arteriosclerosis
In the early stages, arteriosclerosis might not show symptoms. But some people might feel:
- Fatigue or weakness, mainly in the legs
- Mild chest discomfort or pain when active
- Shortness of breath
- Dizziness or feeling lightheaded
These early signs can be hard to notice and might seem like other issues. It’s important to watch for them and see a doctor if they don’t go away or get worse.
Advanced Symptoms by Affected Area
As arteriosclerosis gets worse, symptoms can get clearer. They often match the arteries affected:
- Coronary Arteries: Chest pain (angina), heart attack, or odd heart rhythms
- Carotid Arteries: TIAs or stroke, with symptoms like sudden weakness, vision changes, or trouble speaking
- Peripheral Arteries: Leg pain when walking (claudication), coldness, or numbness in the legs
- Renal Arteries: High blood pressure, kidney failure, or fluid buildup
Spotting these symptoms is key to getting the right medical help.
When to Seek Medical Attention
If you notice any of these, get help right away:
- Severe chest pain or pressure
- Sudden weakness or numbness in the face, arm, or leg
- Difficulty speaking or understanding speech
- Sudden vision changes
- Severe leg pain or cramping
Quick medical check-ups can greatly improve treatment and prevent serious issues. If you’re feeling mild or ongoing symptoms, talk to your doctor for a full check-up and advice.
Diagnosing Arteriosclerosis
Healthcare professionals use many methods to diagnose arteriosclerosis. These include physical exams, lab tests, and imaging studies. This detailed approach helps find out how much the arteries are hardened. It also guides the treatment needed.
Physical Examination Findings
A thorough physical exam is the first step. We look for signs like weak or absent pulses in the limbs. We also check for abnormal heart sounds and evidence of poor circulation. These signs can show if arteriosclerosis is present and how severe it is.
We also check for risk factors like high blood pressure, high cholesterol, and diabetes. Finding these risk factors helps us create a good treatment plan.
Laboratory Tests and Biomarkers
Laboratory tests are key in diagnosing arteriosclerosis. These tests measure biomarkers that show the disease’s presence and how it’s progressing. Some important tests include:
- Lipid profiles: To check cholesterol levels and find risk factors.
- Blood glucose tests: To diagnose and keep track of diabetes.
- C-reactive protein (CRP) tests: To see inflammation levels, linked to arteriosclerosis.
- Kidney function tests: To see how arteriosclerosis affects the kidneys.
Imaging Studies and Specialized Tests
Imaging studies are vital for seeing how much arteriosclerosis affects different organs. Common imaging techniques include:
- Ultrasound: To check blood flow and find blockages or narrowings in arteries.
- Computed Tomography (CT) scans: To see the arteries and find calcification or plaque buildup.
- Magnetic Resonance Imaging (MRI): To look at the heart and blood vessels’ structure and function.
- Angiography: To see inside blood vessels and find blockages or abnormalities.
These methods help doctors accurately diagnose arteriosclerosis. They can see how severe it is and create a treatment plan that fits the patient’s needs.
Arteriosclerosis Treatment Options
Managing arteriosclerosis needs a mix of lifestyle changes, medical treatments, and sometimes surgery. Each person’s situation is different. So, treatment plans are made to fit their specific needs and how severe their condition is.
Lifestyle Modifications as First-Line Therapy
Changing your lifestyle is often the first step against arteriosclerosis. Eating a diet full of fruits, veggies, whole grains, and lean meats is key. Also, regular exercise like walking is important.
Quitting smoking and managing stress through meditation or yoga can also help a lot. Quitting smoking and managing stress are big steps in fighting the disease.
As “The American Heart Association emphasizes the importance of lifestyle changes in managing cardiovascular diseases, including arteriosclerosis.” Making these lifestyle changes can slow down the disease and lower the risk of heart problems.
Medication Approaches
If lifestyle changes aren’t enough, medicine might be needed. We might suggest:
- Statins to lower cholesterol
- Antiplatelet agents to stop blood clots
- Beta-blockers to control blood pressure and heart rate
- ACE inhibitors to relax blood vessels
These medicines can help manage symptoms, slow the disease, and lower the risk of serious problems.
Surgical and Interventional Procedures
In severe cases, surgery or interventional procedures might be needed. We might look at:
- Angioplasty and stenting to open blocked arteries
- Endarterectomy to remove plaque
- Bypass surgery to bypass blocked arteries
These methods can improve blood flow, ease symptoms, and prevent serious issues.
Dealing with arteriosclerosis requires a detailed plan. By combining lifestyle changes, medicines, and sometimes surgery, we can manage the condition well. This approach can greatly improve a person’s quality of life.
Complications of Arteriosclerosis Cardiovascular Disease
It’s important to know the complications of arteriosclerosis to manage the disease well. Arteriosclerosis can cause severe problems, affecting many parts of the body. This can really lower your quality of life.
Arteriosclerotic Heart Disease
Arteriosclerotic heart disease is a big problem caused by arteriosclerosis. It happens when the heart’s blood supply arteries get blocked by plaque. This can cause:
- Angina Pectoris: Pain or discomfort in the chest due to less blood to the heart.
- Myocardial Infarction: Known as a heart attack, it happens when a heart part doesn’t get enough blood, causing damage or death.
Cerebrovascular Complications
When arteriosclerosis affects the brain’s blood supply arteries, it leads to:
- Transient Ischemic Attack (TIA): A short period of symptoms like a stroke, called a “mini-stroke.”
- Stroke: Happens when brain blood supply is cut off or reduced, causing brain tissue damage.
Peripheral Artery Disease and Other Complications
Peripheral artery disease (PAD) is another issue caused by arteriosclerosis. It narrows arteries, reducing blood flow to limbs. Symptoms include:
- Leg pain when walking (claudication)
- Coldness or weakness in the legs
- Sores or wounds on the legs or feet that won’t heal
Other problems can be kidney disease and aneurysms. It’s key to manage arteriosclerosis well to avoid these issues and keep your heart healthy.
Living With and Preventing Arteriosclerosis
Managing arteriosclerosis requires smart choices about diet, exercise, and stress. It’s not easy, but the right steps can greatly improve your life.
Heart-Healthy Diet Strategies
Eating right is key to managing arteriosclerosis. Focus on foods full of nutrients but low in bad fats, cholesterol, and salt. Eat lots of fruits, veggies, whole grains, and lean proteins to help.
Here are some diet tips:
- Eat fatty fish like salmon and mackerel for omega-3s
- Choose healthy fats like avocado and nuts
- Reduce processed and red meats
- Go for low-fat dairy and whole grains
“A healthy diet is not just about cutting out certain foods, but also about incorporating a variety of nutrient-dense foods that support overall cardiovascular health.”
Exercise and Stress Management
Exercise keeps your heart healthy. Aim for 150 minutes of moderate exercise, or 75 minutes of vigorous exercise, or a mix of both, each week. Good choices include brisk walking, cycling, and swimming.
Managing stress is also critical. Stress can worsen arteriosclerosis. Try meditation, deep breathing, and yoga to lower stress.
| Exercise Type | Benefits | Examples |
| Aerobic Exercise | Improves cardiovascular health, reduces blood pressure | Brisk walking, jogging, cycling |
| Resistance Training | Builds muscle, improves metabolism | Weight lifting, bodyweight exercises |
| Flexibility Exercises | Enhances flexibility, reduces injury risk | Yoga, stretching exercises |
Regular Screenings and Monitoring
Regular health checks are essential for managing arteriosclerosis. Keep an eye on blood pressure, cholesterol, and blood sugar. Regular visits to your doctor can catch problems early.
Support Resources and Community
Dealing with arteriosclerosis is tough, but support helps a lot. Join online or in-person support groups to connect with others facing similar challenges.
Also, get advice from health experts, nutritionists, and fitness coaches. They can offer personalized tips for you.
Conclusion
Arteriosclerosis is a big problem for heart health. Knowing its causes, signs, and symptoms is key to catching it early. Eating right and exercising can help a lot in preventing heart issues.
Preventing arteriosclerosis is very important. Knowing what increases your risk helps you take action. Doctors may also use medicines or surgery to help manage it.
Combining healthy living, medical care, and support can make a big difference. Regular check-ups are also essential. This way, we can catch any changes early and act fast. Working with doctors is the best way to manage arteriosclerosis and stay healthy.
FAQ
What is arteriosclerosis?
Arteriosclerosis is when arteries get hard. This can cause heart problems. It includes atherosclerosis, arteriolosclerosis, and vascular sclerosis.
What is the difference between arteriosclerosis and atherosclerosis?
Arteriosclerosis is a wide term for artery hardening. Atherosclerosis is a specific case of it, caused by plaque buildup. They’re often mixed up, but atherosclerosis is a part of arteriosclerosis.
What are the risk factors for developing arteriosclerosis?
Risk factors include high cholesterol, high blood pressure, and smoking. Age and family history also play a role.
What are the symptoms of arteriosclerosis?
Symptoms vary based on where the arteries are affected. Early signs might be mild discomfort. Severe pain or organ damage can happen later.
How is arteriosclerosis diagnosed?
Doctors use physical exams, lab tests, and imaging to diagnose arteriosclerosis. It’s a detailed process.
What are the treatment options for arteriosclerosis?
Treatment starts with lifestyle changes. Then, doctors might prescribe medicine or surgery. It depends on the person’s situation.
Can arteriosclerosis be prevented?
Yes, it can be prevented or managed. Eating well, exercising, managing stress, and regular check-ups help.
What are the complications of arteriosclerosis?
Complications include heart disease, brain problems, and peripheral artery disease. These are serious issues.
How can I manage arteriosclerosis?
Managing it involves lifestyle changes, medical care, and support. It’s a team effort.
What is vascular sclerosis?
Vascular sclerosis is when blood vessels harden. It’s a form of arteriosclerosis.
What is arteriolosclerosis?
Arteriolosclerosis is when small arteries thicken. It’s a type of arteriosclerosis.
Is arthrostenosis related to arteriosclerosis?
Yes, arthrostenosis is linked to vascular sclerosis, which is a form of arteriosclerosis.
References
Libby, P., & Hansson, G. K. (2019). Inflammation in atherosclerosis: From pathophysiology to practice. Journal of the American College of Cardiology, 74(10), 1376-1398. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7089587/


































