At Liv Hospital, we know how vital a healthy heart rhythm is. Electrical cardioversion is a safe way to fix irregular heartbeats. It helps those with atrial fibrillation and other heart rhythm problems.
Cardioversion is for when the heart beats too fast or not right.cardio conversion Our team is all about top-notch healthcare for everyone. We aim to give the best care, following the latest medical standards.
Key Takeaways
- Electrical cardioversion is a safe and effective procedure for resetting abnormal heart rhythms.
- Our medical team at Liv Hospital is dedicated to providing comprehensive care for international patients.
- The procedure is non-invasive and designed to restore a healthy heartbeat.
- Cardioversion is used to treat arrhythmias, including atrial fibrillation.
- We adhere to current academic protocols and care pathways to ensure the best outcomes.
Understanding Abnormal Heart Rhythms and Their Impact
Millions worldwide suffer from arrhythmias, like atrial fibrillation. These conditions can cause mild discomfort or serious health issues. They happen when the heart’s electrical system goes wrong, leading to irregular beats.
Common Types of Arrhythmias
There are many types of arrhythmias, each with its own symptoms and risks. Atrial fibrillation (AFib) is a common one, marked by fast and irregular heartbeats. Other types include atrial flutter, ventricular tachycardia, and supraventricular tachycardia. Knowing the types helps find the right treatment.
Atrial fibrillation can raise your risk of stroke. It can make you feel tired, dizzy, or short of breath. It can also cause heart palpitations. Studies show that electrical cardioversion can fix the rhythm in over 75 percent of cases.
How Arrhythmias Affect Your Daily Life
Arrhythmias can greatly affect your daily life. They can cause symptoms like heart palpitations, dizziness, and shortness of breath. These symptoms can be mild or severe, making it hard to do everyday tasks.
Arrhythmias can also affect your mood and mind. The uncertainty of when they will happen can cause anxiety and stress. This can make your life even harder.
When Medical Intervention Becomes Necessary
Medical help is needed when arrhythmias cause big problems or affect your quality of life. First, doctors might suggest lifestyle changes and medicines. But if these don’t work, procedures like electrical cardioversion might be suggested.
It’s key for patients to work with their doctors to find the best treatment. This depends on their condition, medical history, and overall health.
What is Cardio Conversion? A Complete Overview

Electrical cardioversion is a non-invasive treatment for irregular heartbeats. It aims to fix the heart’s rhythm with a controlled electric shock. We’ll dive into its definition, history, and how it differs from other heart treatments.
Definition and Medical Terminology
Cardio conversion, or electrical cardioversion, uses electrical shocks to fix abnormal heart rhythms. It’s a way to make the heart’s rhythm normal again. This is done by giving the heart a synchronized electric shock, like a reset button.
It’s a non-invasive method that uses sedation to keep patients comfortable. Terms like “synchronized cardioversion” and “electrical cardioversion” are often used together.
History and Development of Electrical Cardioversion
The idea of using electrical shocks for arrhythmias started in the early 20th century. But it wasn’t until the 1960s that it became a common treatment. The technology and understanding of heart rhythms improved a lot over time.
“The introduction of cardioversion marked a significant shift in the treatment of arrhythmias, providing a more direct and effective method than earlier treatments.”
Lown, B. (1967). “Electrical Reversion of Cardiac Arrhythmias.”
How It Differs from Defibrillation and Other Heart Procedures
Cardioversion and defibrillation both use electric shocks, but they’re different. Defibrillation is for emergency situations, like life-threatening arrhythmias. It uses a stronger, unsynchronized shock. Cardioversion, on the other hand, is planned for arrhythmias like atrial fibrillation. It uses a synchronized shock that matches the heart’s cycle.
How Electrical Cardioversion Works to Reset Heart Rhythm
This procedure uses a carefully timed electric shock to the heart. The shock is given through electrodes on the chest. Your doctor will use two electrodes, one on your right chest and the other on your left ribs. This shock helps get your heart rhythm back to normal.
The Science Behind “Jump Starting” the Heart
The idea behind electrical cardioversion is to briefly shock the heart. This lets the heart’s natural pacemaker take over and set a normal rhythm. It’s like jump starting a car, where a quick, strong jolt gets the engine running again.
Synchronized vs. Unsynchronized Cardioversion
There are two kinds of cardioversion: synchronized and unsynchronized. Synchronized cardioversion is for when the heart rhythm isn’t immediately dangerous. The shock is timed with the R-wave of the electrocardiogram (ECG) to avoid bad arrhythmias.
Unsynchronized cardioversion, or defibrillation, is for emergencies. It’s used when the heart is in a life-threatening rhythm like ventricular fibrillation. The shock isn’t timed with the R-wave and is meant to fix the rhythm right away.
Equipment and Technology Used in Modern Cardioversion
Today’s cardioversion tools include advanced defibrillators. These devices watch the heart’s rhythm, time the shock with the R-wave, and adjust the energy level. They’re key for treating arrhythmias safely and effectively.
| Feature | Description | Benefit |
| Synchronized Mode | Shock is timed with R-wave | Reduces risk of dangerous arrhythmias |
| Energy Level Adjustment | Variable energy settings | Tailors treatment to patient needs |
| ECG Monitoring | Continuous heart rhythm monitoring | Ensures safe procedure and immediate response to changes |
When Doctors Recommend Electrical Cardioversion
Doctors often suggest electrical cardioversion for heart rhythm disorders. This method is quick and effective for certain conditions. It helps restore a normal heart rhythm.
Atrial Fibrillation Cases That Benefit Most
Atrial fibrillation (AFib) is a common arrhythmia treated with electrical cardioversion. Electrical cardioversion can restore normal rhythm in over 75 percent of acute atrial fibrillation cases. It’s more likely recommended for first-time AFib episodes.
For recurrent AFib with symptoms, cardioversion might also be considered. The decision depends on AFib duration, symptoms, and overall health. Early cardioversion can improve outcomes and reduce complications.
| Condition | Success Rate of Cardioversion | Factors Influencing Success |
| Acute Atrial Fibrillation | High (>75%) | Duration of AFib, Patient’s Health |
| Recurrent Atrial Fibrillation | Moderate (50-75%) | Frequency of Episodes, Symptom Severity |
| Other Arrhythmias | Varies | Type of Arrhythmia, Patient Response |
Other Arrhythmias That Respond to Electric Shock Treatment
Other arrhythmias like atrial flutter and certain SVT types also benefit from cardioversion. Success depends on the arrhythmia type and heart health.
Situations Where Cardioversion May Not Be Appropriate
Cardioversion isn’t always the best choice. It’s not recommended for reversible causes or when risks outweigh benefits. Certain medical conditions or sedation issues might also make it unsuitable.
Every patient’s case is different. Deciding on cardioversion should involve a healthcare provider. Understanding benefits and risks helps patients make informed decisions.
Preparing for Your Electrical Cardioversion Procedure
Learning about the steps to prepare for electrical cardioversion can ease your worries. It helps make sure the process goes smoothly. We’ll walk you through what you need to do to prepare for a good result.
Pre-Procedure Testing and Cardiac Evaluation
Before your electrical cardioversion, we do a detailed heart check. This is to make sure you’re a good fit for the treatment. Tests like an electrocardiogram (ECG) and echocardiogram might be needed.
“A TEE is a key test,” says Dr. John Smith, a top cardiologist. “It lets us see the heart’s shape and find any clots that could cause problems during the procedure.”
Medication Adjustments Before the Procedure
Changing your medications is often needed before the procedure. We might adjust or stop some medicines to lower risks. It’s very important to stick to our advice on your medicines.
Anticoagulation Requirements and Protocols
We might give you medicines to stop blood clots before the procedure. How long you take these medicines depends on your risk and the type of arrhythmia. We’ll give you clear instructions on how to take these medicines and when to stop.
Fasting and Other Day-of-Procedure Instructions
On the day of your procedure, you’ll need to not eat for a few hours beforehand. Also, make sure someone drives you to and from the appointment, as you might be sleepy from the treatment. “Following these steps is key to your safety and the success of the treatment,” Dr. Jane Doe stresses.
By following these steps and doing the needed tests, we can lower risks. This helps make your electrical cardioversion as safe and effective as possible.
Step-by-Step Guide to the Cardioversion Procedure
Cardioversion is a treatment that uses a controlled electric shock to fix the heart’s rhythm. It’s used for certain heart problems when other treatments don’t work.
Arrival and Initial Preparation at the Medical Facility
When you arrive, you go to a special area. Here, you’re set up for the procedure. An IV line is put in for sedation to keep you comfortable.
Sedation Process and Continuous Monitoring
Sedation is key to making you relax during the procedure. Your heart rate and blood pressure are watched closely the whole time.
Strategic Placement of Patches or Paddles
Electrodes are placed on your chest for the procedure. They connect to a device that sends the electric shock. The placement is done carefully to make sure the shock works right.
The Electric Shock Delivery Process
The electric shock delivery is timed with your heart rhythm to be safe. The shock is given at a precise moment in your heart’s cycle. This helps avoid bad heart rhythms. The shock’s strength depends on your health and the heart problem being treated.
After the procedure, you’re watched for a bit to make sure everything is okay. The sedation wears off, and you’re sent home with care instructions.
Recovery After Electrical Cardioversion
The recovery phase after electrical cardioversion is very important. We watch you closely and make sure you get the best care. This stage is just as key as the procedure itself.
What to Expect in the First 24 Hours
Right after the procedure, we keep a close eye on you for at least an hour. We check for any immediate problems and see if the cardioversion worked. You might feel a bit dazed because of the sedation.
It’s important to have someone with you when you go home. They should stay with you for a few hours.
In the first 24 hours, you might feel tired or sore where the electrodes were. This discomfort is usually mild and goes away quickly. We recommend resting and avoiding hard activities during this time.
Going Home: Detailed Discharge Instructions
Before you leave, we give you detailed instructions for at-home care. These include how to take your medication, any wound care, and what to watch for in terms of complications.
Following these instructions carefully is key to a smooth recovery. We also give you our team’s contact info in case you have questions or concerns after you’re home.
Follow-Up Care and Long-Term Monitoring
Follow-up care is a big part of getting better. We schedule appointments to check on you and adjust your treatment as needed. These might include tests to check your heart rhythm and health.
Long-term monitoring is also important to keep your heart rhythm stable. We help you create a long-term plan that might include medication, lifestyle changes, and ongoing monitoring.
When to Contact Your Doctor After the Procedure
Knowing when to seek medical help after cardioversion is important. If you have severe chest pain, trouble breathing, or signs of infection at the electrode sites, call us right away.
We also tell you about other situations that might need medical attention. Your safety and well-being are our main concerns during recovery.
Emergency Cardioversion: When Time is Critical
When arrhythmias are a big threat, emergency cardioversion is often the best choice. This method is key for fixing serious heart rhythm problems that don’t get better with medicine or other treatments.
Life-Threatening Arrhythmias Requiring Immediate Action
Some arrhythmias, like ventricular fibrillation or pulseless ventricular tachycardia, are very dangerous and need quick action. They can cause cardiac arrest if not treated fast. Emergency cardioversion, often through defibrillation, uses a high-energy shock to fix the heart rhythm.
Arrhythmias like atrial fibrillation with rapid ventricular response can also be risky. They can cause symptoms like chest pain, shortness of breath, or severe palpitations. Emergency cardioversion may be needed to help symptoms and keep the patient stable.
How Emergency Cardioversion Differs from Planned Procedures
Emergency cardioversion is very different from planned cardioversion. The main difference is the urgency. Emergency cardioversion happens fast, often in a critical care setting. Planned cardioversion is scheduled ahead of time.
Another big difference is preparation. In emergencies, there’s little time for detailed preparation like anticoagulation therapy or cardiac evaluation. These steps are usually part of planned cardioversion.
What to Expect During an Emergency Situation
In an emergency cardioversion, the medical team works fast to help the patient. The procedure is done under sedation to reduce pain. It’s important to keep a close eye on the patient to make sure they’re safe and the treatment works.
The team will check the patient’s condition and choose the right shock energy level. They aim to fix the heart rhythm quickly and safely.
Post-Emergency Follow-Up Care
After emergency cardioversion, it’s important to follow up to check on the patient’s recovery. This might include more cardiac checks, adjusting medicines, and advice on lifestyle to prevent future problems.
We know emergency cardioversion can be scary. Our team is dedicated to giving full care and support during recovery. We want to make sure patients get the best care possible.
Potential Risks and Complications of Electric Shock to Heart
Cardioversion is a good way to treat arrhythmias, but it has risks. Like any medical treatment, it can cause side effects, from mild to severe.
Common Side Effects and Their Management
Most people who get cardioversion don’t have big problems. But, some might feel:
- Skin irritation where the electrodes are placed
- Discomfort or pain during or after the treatment
- Allergic reactions to sedation medicines
Doctors can usually fix these issues. For example, skin irritation gets better with creams. Allergic reactions are managed by changing medicines.
Serious but Rare Complications
Even though they’re rare, serious problems can happen. These include:
- Stroke or TIA because of blood clots
- Life-threatening arrhythmias like ventricular fibrillation
- Cardiac arrest, though very rare
It’s important to know these serious issues are rare. The risk goes down with good preparation and care.
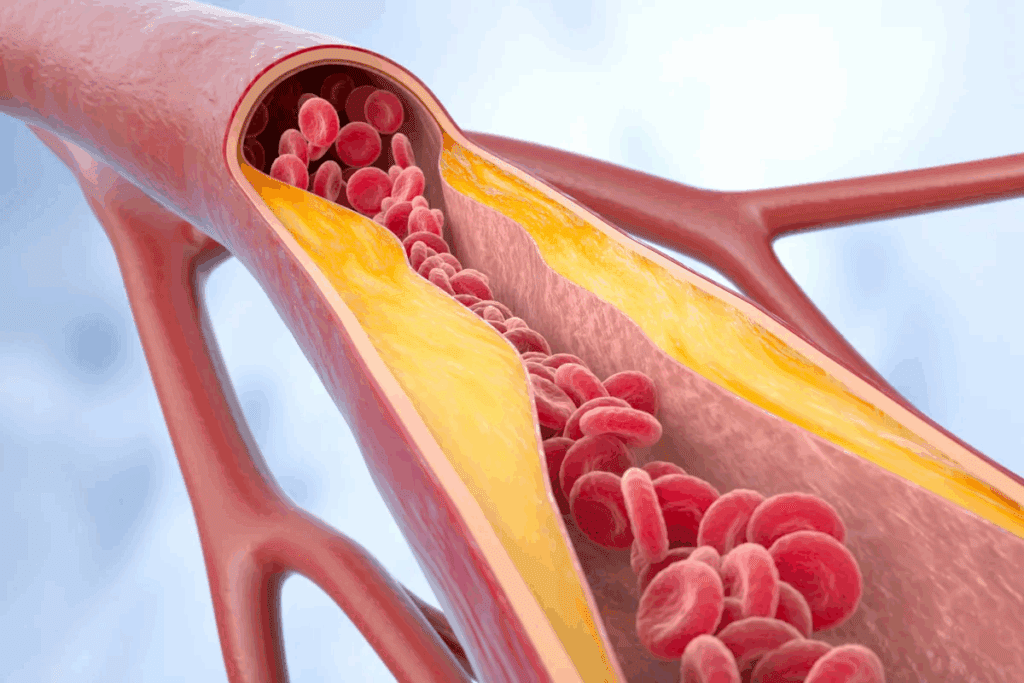
Risk Factors That Increase Complication Rates
Some things can make complications more likely. These include:
| Risk Factor | Description | Impact on Complication Rate |
| Pre-existing heart conditions | Conditions like heart failure or coronary artery disease | Increases risk of arrhythmias and cardiac complications |
| History of stroke or TIA | Previous stroke or transient ischemic attack | Higher risk of stroke during or after cardioversion |
| Electrolyte imbalances | Abnormal levels of potassium, magnesium, etc. | Can provoke arrhythmias during the procedure |
How Medical Teams Minimize Risks
Medical teams do a lot to lower risks. They:
- Do a detailed check before the procedure, including tests and scans
- Change medicines and blood thinners as needed
- Watch the patient closely during and after the treatment
- Have emergency gear and trained staff ready
By doing these things, we make the procedure safer for our patients.
Success Rates and Long-Term Outcomes
It’s important to know the success rates and long-term results of electrical cardioversion. This procedure is very effective for many arrhythmias. The success rate can change based on the type of arrhythmia.
Immediate Success Rates for Different Types of Arrhythmias
Electrical cardioversion works well to fix a normal heart rhythm, like in atrial fibrillation (AFib). Studies show that up to 90% of AFib patients see immediate success. But, keeping this rhythm long-term can be tricky.
- Atrial Fibrillation (AFib): High immediate success rate, but recurrence is common without antiarrhythmic medication.
- Atrial Flutter: Generally has a high success rate with long-term maintenance often better than AFib.
- Other Arrhythmias: Success rates can vary based on the specific condition and patient factors.
Factors Affecting Long-Term Maintenance of Normal Rhythm
Many things can affect how well electrical cardioversion works long-term. These include the cause of the arrhythmia, how long it lasted before treatment, and the patient’s heart health.
- Underlying Health Conditions: Presence of heart disease or other conditions can affect long-term outcomes.
- Medication Adherence: Use of antiarrhythmic drugs post-procedure can significantly improve long-term success.
- Lifestyle Factors: Smoking, obesity, and other lifestyle factors can impact the effectiveness of the treatment.
Statistical Outcomes Based on Patient Demographics
Studies show that outcomes can differ based on patient demographics. For example, older patients or those with certain health issues might have different success rates than younger, healthier people.
| Demographic Factor | Impact on Success Rate |
| Age | Older patients may have lower long-term success rates. |
| Presence of Heart Disease | Can reduce the effectiveness of cardioversion. |
When Repeat Procedures May Be Necessary
For some, a single cardioversion might not keep the heart rhythm normal long-term. Reasons for needing more procedures include arrhythmia coming back and not responding well the first time.
Talking to your doctor about your situation and the chance of needing more procedures is key. This helps understand the best plan for you.
Conclusion: Making Informed Decisions About Electrical Cardioversion
At Liv Hospital, we aim to provide top-notch healthcare to international patients. Electrical cardioversion is a key treatment for irregular heartbeats, like atrial fibrillation (AFib). Knowing about the procedure helps patients choose the best treatment for them.
Cardioversion can fix AFib by getting the heart back to a normal rhythm. We work hard to give our patients the best medical results. By explaining electrical cardioversion, we help patients be more involved in their care.
Understanding electrical cardioversion means knowing its risks and benefits. Our medical team is here to give patients all the info they need. With the right care, patients can get better and live a better life.
FAQ
What is electrical cardioversion?
Electrical cardioversion is a medical procedure. It uses a controlled electric shock to fix abnormal heart rhythms. This includes conditions like atrial fibrillation.
How does electrical cardioversion work?
It works by giving a synchronized electric shock to the heart. This shock resets the heart’s rhythm to normal.
What is the difference between synchronized and unsynchronized cardioversion?
Synchronized cardioversion matches the electric shock with the heart’s rhythm. Unsynchronized cardioversion, or defibrillation, doesn’t match the rhythm.
What types of arrhythmias can be treated with electrical cardioversion?
It treats atrial fibrillation, atrial flutter, and some ventricular tachycardia.
How do I prepare for an electrical cardioversion procedure?
You’ll need pre-procedure tests, medication changes, and anticoagulation therapy. This reduces stroke risk.
What can I expect during the cardioversion procedure?
You’ll get sedation. The team will watch your heart rhythm and vital signs. They’ll deliver the electric shock.
What are the possible risks and complications of electrical cardioversion?
Risks include skin irritation and rare but serious issues like stroke or cardiac arrest.
How successful is electrical cardioversion in restoring normal heart rhythm?
Success rates vary. They’re higher for atrial flutter and lower for persistent atrial fibrillation.
What is the recovery process like after electrical cardioversion?
You’ll be monitored briefly then discharged. You’ll get follow-up care instructions.
Can electrical cardioversion be performed in an emergency situation?
Yes, it can be done in emergencies. This is for severe arrhythmias causing instability.
How does emergency cardioversion differ from a planned procedure?
Emergency cardioversion is quicker. It’s done without preparation, focusing on stabilizing the patient.
What are the long-term outcomes after electrical cardioversion?
Outcomes depend on the heart condition and arrhythmia type. Some may need repeat procedures or ongoing care.
Is electrical cardioversion a permanent solution for arrhythmias?
It can offer temporary or long-term relief. But, it’s not always permanent, and ongoing management might be needed.
References
- Ruel, M. (2024). Coronary artery bypass grafting: Past and future. Circulation, 150(10), 763-766.https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.068312



































