Atrial fibrillation and other heart rhythm disorders can really affect a person’s life. Cardioversion is a medical procedure that offers new hope for those with irregular heartbeats. It’s used to treat arrhythmias, where the heart beats too fast or irregularly.
Knowing the risks and benefits of cardioversion helps patients make better choices. At places like Liv Hospital, we use the latest methods and focus on the patient. This way, we help patients get the best care, from start to finish.
Key Takeaways
- Cardioversion is a procedure used to restore a normal heart rhythm.
- Understanding the risks and benefits is key for making good choices.
- Using the latest methods and caring for the patient improves results.
- Recovery time varies, but most people can get back to normal activities quickly.
- Trusted medical centers offer full support during the cardioversion process.
Understanding Cardioversion: Definition and Purpose
Cardioversion is a complex and fascinating medical procedure. It aims to fix irregular heartbeats in patients with certain arrhythmias.
Definition of Cardioversion
Cardioversion uses electrical shocks or medicine to fix an abnormal heart rhythm. It turns an irregular heartbeat back to normal. This is done with a controlled electrical shock or special medicines.
Common Heart Rhythm Disorders Treated with Cardioversion
Cardioversion helps with many arrhythmias, including:
- Atrial fibrillation: A fast and irregular heartbeat in the atria.
- Atrial flutter: A fast, regular heartbeat in the atria.
- Atrial tachycardia: A fast heart rate starting in the atria.
- Ventricular tachycardia: A dangerous arrhythmia starting in the ventricles.
These conditions can cause symptoms like palpitations, shortness of breath, and fatigue. They can really affect a person’s life quality.
Goals of the Procedure
The main goals of cardioversion are to fix the heart rhythm and ease symptoms. It aims to improve a patient’s life quality. By fixing the rhythm, it also lowers the risk of serious problems like stroke and heart failure.
| Arrhythmia Type | Success Rate of Cardioversion | Common Symptoms |
| Atrial Fibrillation | 70-90% | Palpitations, shortness of breath |
| Atrial Flutter | 80-95% | Rapid heartbeat, fatigue |
| Atrial Tachycardia | 60-85% | Rapid heartbeat, dizziness |
| Ventricular Tachycardia | 50-80% | Palpitations, loss of consciousness |
Understanding cardioversion helps patients and doctors make better choices. It’s key in managing heart rhythm disorders.
Types of Cardioversion Procedures
Cardioversion treats irregular heart rhythms in two main ways. It aims to bring the heart back to a normal rhythm. These methods are electrical cardioversion and pharmacologic cardioversion. Knowing about these is key for both patients and doctors to choose the best treatment.
Electrical Cardioversion: The “Shock Treatment for the Heart”
Electrical cardioversion is like a “shock treatment for the heart.” It uses a controlled electric shock to the chest to fix the rhythm. This is done while the patient is sedated or under anesthesia to reduce pain.
The electric shock is timed with the heart’s cycle for safety and success.
The benefits of electrical cardioversion are:
- Quickly fixes the heart rhythm
- Works well for some arrhythmias
- Shows results right away
Pharmacologic Cardioversion
Pharmacologic cardioversion uses medicines to fix the heart rhythm. It’s often chosen for patients not good for electrical cardioversion or with specific arrhythmias that medicines can help.
Key points about pharmacologic cardioversion are:
- Uses anti-arrhythmic drugs
- May have fewer risks than electrical cardioversion
- Is better for some patients
Differences Between the Two Approaches
Choosing between electrical and pharmacologic cardioversion depends on many factors. These include the arrhythmia type, patient health, and the situation. The main differences are how the rhythm is fixed, how fast it happens, and possible side effects.
| Characteristics | Electrical Cardioversion | Pharmacologic Cardioversion |
| Method | Electric shock | Anti-arrhythmic medications |
| Speed of Effect | Immediate | Variable, depending on medication |
| Potential Risks | Related to anesthesia and electric shock | Medication side effects |
It’s important to know the differences between electrical and pharmacologic cardioversion. This helps decide the best treatment plan. We’ll look at more details and implications in the next sections.
When Is Cardioversion Necessary?
Cardioversion is needed when certain heart rhythms are off. It’s used to fix these issues. This is key for people with specific heart problems.
Medical Indications for Cardioversion
It’s mainly for treating irregular heartbeats like atrial fibrillation. Symptoms like palpitations or shortness of breath are common reasons. It’s chosen when these symptoms really affect a person’s life or when other treatments don’t work.
Common medical indications for cardioversion include:
- Symptomatic atrial fibrillation or flutter
- Arrhythmias that have not responded to medication
- Significant symptoms affecting daily life
Symptoms That May Require Cardioversion
Severe palpitations, dizziness, or chest pain might need cardioversion. These symptoms can make it hard to do everyday things. They might show that a person needs this treatment.
Emergency vs. Planned Cardioversion
Cardioversion can be urgent or planned. Emergency cardioversion is for severe symptoms like unstable heart function. Planned cardioversion is for those with ongoing arrhythmias that haven’t gotten better with other treatments.
| Characteristics | Emergency Cardioversion | Planned Cardioversion |
| Urgency | Immediate, due to severe symptoms | Scheduled in advance |
| Patient Condition | Hemodynamically unstable | Stable, but symptomatic |
| Preparation | Minimal preparation | Anticoagulation therapy and other preparations |
When Other Treatments Have Failed
Cardioversion is considered when other treatments don’t work. This includes medicines for heart rhythm. It’s a good option for managing arrhythmias.
Knowing when cardioversion is needed helps both patients and doctors. It’s about making the right choice for heart health.
Preparing for a Cardioversion Procedure
Getting ready for a cardioversion is key. This includes medical tests and adjusting your medications. It’s important to listen to your doctor and know what to expect.
Pre-Procedure Testing
Your doctor will run several tests before the procedure. These tests check your heart and overall health. You might have:
- Electrocardiogram (ECG): This test looks at your heart’s rhythm and finds any problems.
- Echocardiogram: An ultrasound that shows your heart’s structure, helping find any issues.
- Blood Tests: These tests check for conditions that could affect the procedure or your recovery.
Medical experts say, “Thorough pre-procedure testing is vital for identifying risks and ensuring a safe procedure.”
Medication Adjustments
Your medications might need to change before the procedure. This could mean:
- Stopping certain medications: Your doctor might tell you to stop taking some medications that could interfere.
- Adjusting dosages: The amount of some medications might need to change to keep you safe during the procedure.
It’s important to follow your doctor’s advice on medication changes to avoid risks.
Anticoagulation Therapy Before Cardioversion
Anticoagulation therapy is often used before cardioversion. This means taking medications that thin your blood, like warfarin or NOACs. You’ll need to take these medications for at least three to four weeks before the procedure.
Fasting and Other Preparation Guidelines
You’ll get advice on fasting and other things to do before the procedure. You might need to:
- Fast for a certain period: You’ll need to avoid eating and drinking for a while before the procedure.
- Arrange for transportation: Because you might be sedated, you’ll need someone to drive you home.
- Wear comfortable clothing: Wear loose, comfortable clothes for your ease during the procedure.
By following these guidelines, you can help make the procedure go smoothly and successfully.
What Is Cardioversion: The Procedure Step by Step
The cardioversion process has several key steps. These steps ensure a safe and effective way to restore a normal heart rhythm. We will explain what happens before, during, and after the procedure.
Before the Procedure
Before cardioversion, we conduct several tests to check if you’re a good candidate. These tests include an electrocardiogram (ECG), blood tests, and sometimes a transesophageal echocardiogram (TEE). We also review your medications to reduce risks during the procedure.
Pre-procedure preparation is key for a successful cardioversion. You’ll get instructions on fasting and arranging a ride home. It’s important to follow these steps carefully.
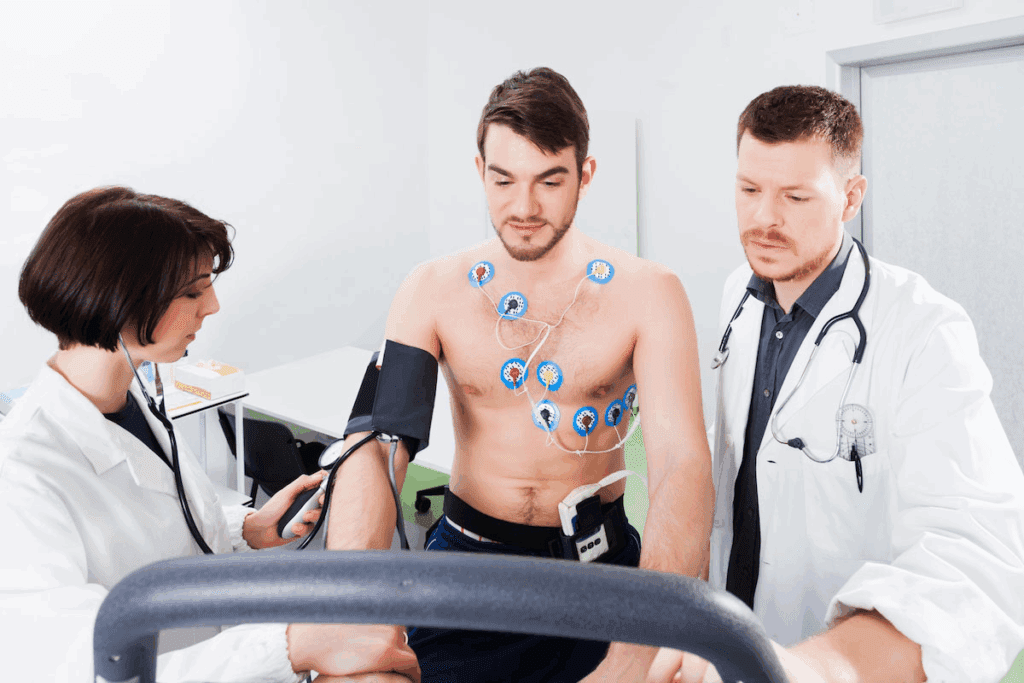
During Electrical Cardioversion
During electrical cardioversion, you’ll receive sedation to relax. We monitor your heart rhythm and vital signs closely. Electrode patches are placed on your chest and connected to a cardioversion device.
The electric shock is timed with your ECG’s R-wave to reduce risks. We watch how you respond and might adjust the shock’s energy level if needed.
During Pharmacologic Cardioversion
Pharmacologic cardioversion uses medications to restore a normal heart rhythm. We choose the right medication based on your condition and medical history. The medication is given intravenously, and we monitor your heart rhythm and response.
The goal is to convert your arrhythmia to a normal rhythm without electric shock. We watch for side effects and adjust the treatment as necessary.
Monitoring During the Procedure
During the procedure, whether electrical or pharmacologic, we monitor your heart rhythm, blood pressure, and oxygen levels. This lets us quickly respond to any changes or complications.
Our close monitoring ensures your safety and the procedure’s success. We adjust our approach as needed to achieve the best outcome.
Recovery Time for Cardioversion
Recovering from cardioversion involves several stages. These include immediate care after the procedure and getting back to normal activities. Knowing these stages helps patients recover smoothly.
Immediate Post-Procedure Recovery
Right after the procedure, patients go to a recovery area. Medical staff watch over them closely. This stage is key for catching any early signs of trouble.
Monitoring and Care: Patients are checked for heart rhythm and overall health. Staff look for any complications, like arrhythmias or reactions to anesthesia.
Going Home After Cardioversion
Most patients can go home the same day, if there are no issues. Before leaving, they get care instructions and schedule follow-up visits.
Discharge Criteria: Patients are sent home when they’re stable and fully awake. They must also show no immediate complications.
| Discharge Criteria | Description |
| Stable Condition | Patient’s vital signs are within normal limits. |
| Return to Pre-Procedure Consciousness | Patient is fully awake and alert. |
| No Immediate Complications | No signs of arrhythmias or other complications. |
Activity Restrictions
After cardioversion, patients need to follow activity limits. This means avoiding hard work and heavy lifting for a while.
“It’s vital for patients to stick to their activity limits. This helps avoid complications after cardioversion.”
Exercise After Cardioversion
Starting exercise after cardioversion should be slow and guided by a doctor. The aim is to get back to normal without pushing too hard.
Guidelines for Resuming Exercise: Begin with light activities and slowly increase intensity. It’s important to listen to how your body feels and adjust as needed.
By following these guidelines and their healthcare team’s advice, patients can recover safely and effectively after cardioversion.
Risks and Complications of Cardioversion
It’s important to know the risks and complications of cardioversion before you decide to have it. While it’s usually safe, there are some possible risks.
Common Minor Complications
Most people who have cardioversion don’t have big problems. But, some might face minor issues like:
- Skin Irritation: Redness or irritation where the electrodes are placed.
- Discomfort: Feeling a bit uncomfortable during or after the procedure.
- Temporary Changes in Blood Pressure: Blood pressure might go up or down, but it usually goes back to normal.
Serious Possible Complications
Even though they’re rare, serious problems can happen. These might include:
- Stroke or Blood Clots: There’s a small chance of stroke or blood clots, mainly for those with atrial fibrillation.
- Arrhythmias: Cardioversion might cause new heart rhythm problems or make old ones worse.
- Heart Attack: Though rare, there’s a small risk of a heart attack.
Medication-Related Complications
For those getting medication to help their heart, there are extra risks. These can be:
- Side Effects: Different side effects like dizziness, nausea, or allergic reactions, depending on the medication.
- Interactions: The medication might not work well with other drugs you’re taking.
Talking to your doctor about your health and any worries you have is key to lowering risks.
Long-Term Side Effects and Success Rates
It’s important to know the long-term effects of cardioversion before you decide on it. This treatment can fix a heart rhythm problem. But, it’s key to think about its long-term success and possible side effects.
Physical Side Effects
Cardioversion is usually safe, but it can have some long-term effects. Some people might see:
- Skin irritation or redness at the electrode site
- Mild chest discomfort
- Palpitations or irregular heartbeats
These effects are usually short-lived and go away by themselves. But, it’s important to check in with your doctor to make sure everything is okay.
Psychological Impact
The emotional side of cardioversion is also important. Patients might feel anxious or stressed about the procedure and their heart health. Talking to your doctor about these feelings is a big help.
Recurrence of Arrhythmias
Another thing to think about is if arrhythmias might come back. How likely this is depends on your heart condition and how well you take care of yourself after the procedure. Staying on top of your medications and doctor visits can help.
Factors Affecting Long-Term Success
Several things can affect how well cardioversion works in the long run. These include:
- The cause of the arrhythmia
- Other heart problems you might have
- How well you follow your doctor’s advice after the procedure
- Keeping up with regular check-ups with your doctor
By understanding and dealing with these factors, you can increase your chances of a good outcome.
In summary, cardioversion is a good option for some heart rhythm problems. But, knowing its long-term effects and success rates is key to making the right choice. Thinking about the physical and emotional impacts, and what affects long-term success, helps patients make the best decisions for their treatment.
Is Cardioversion Safe? Safety Considerations
Understanding the safety of cardioversion is key. It’s seen as safe when done right, but it has risks and complications.
Safety Profile of Cardioversion
Cardioversion is mostly safe for most people. Electrical cardioversion is safe with the right precautions. But, some factors can raise the risk of problems.
Who Should Avoid Cardioversion
Not everyone is a good candidate for cardioversion. Those with heart issues like digitalis toxicity or severe heart failure are at higher risk. Choosing the right patients and checking them before the procedure is important.
Risk Factors That Increase Complications
Some factors can make cardioversion riskier. These include a history of arrhythmias, pacemakers or ICDs, and certain meds. Knowing these helps manage what to expect.
How Doctors Ensure Patient Safety
Doctors take many steps to keep patients safe during cardioversion. They do a detailed check before, watch closely during, and care for patients after. Anticoagulation therapy helps prevent blood clots. Having skilled staff and the right tools is also key.
With the right steps, cardioversion can be a safe and helpful treatment for heart rhythm problems.
Conclusion: Making Informed Decisions About Cardioversion
Understanding cardioversion helps patients make smart choices. It’s a key treatment for heart rhythm problems, aiming to fix the heart’s rhythm.
It’s important to think about the cardioversion risks and benefits when deciding. While it’s usually safe, there can be side effects or serious issues. Your doctor will guide you, helping you choose the best path.
To make a good choice, look at your health, the heart issue, and what cardioversion can do. Talk to your doctor about your worries. This way, you’ll be ready to decide on this treatment.
For many, cardioversion can change their life for the better. By carefully looking at the treatment, you can pick what’s best for your health and well-being.
FAQ
What is cardioversion?
Cardioversion is a medical procedure. It helps people with abnormal heart rhythms, or arrhythmias, get back to a normal rhythm.
Is cardioversion a surgical procedure?
No, it’s not surgical. It’s a non-invasive treatment. It uses electrical shocks or medications to fix the heart rhythm.
What are the risks associated with cardioversion?
Minor risks include skin irritation or redness. Serious risks like stroke, heart attack, or cardiac arrest are rare but possible.
How long is the recovery time for cardioversion?
Recovery is usually quick. Most people can get back to normal in a few days. Always follow your doctor’s advice on activity and exercise.
Can cardioversion be performed as an emergency procedure?
Yes, it can be done in emergencies. This is if the arrhythmia is life-threatening or causing severe symptoms.
What are the differences between electrical and pharmacologic cardioversion?
Electrical cardioversion uses shocks to fix the rhythm. Pharmacologic cardioversion uses medications for the same purpose.
How effective is cardioversion in treating arrhythmias?
It’s usually effective in fixing the rhythm. But success depends on the arrhythmia cause and any underlying health issues.
Are there any long-term side effects of cardioversion?
Long-term side effects are rare. But some might experience psychological impacts or arrhythmia recurrence.
Can I exercise after cardioversion?
Always follow your doctor’s exercise advice after cardioversion. Avoid strenuous activities for a few days and then gradually return to normal exercise.
Who should avoid cardioversion?
Some people, like those with certain medical conditions or on specific medications, should avoid it. Always talk to your healthcare provider about your situation.
How do doctors ensure patient safety during cardioversion?
Doctors ensure safety by carefully choosing patients, monitoring during the procedure, and adjusting treatment plans as needed.
What is the success rate of cardioversion?
Success rates vary based on the individual and the arrhythmia type. It’s often effective for certain arrhythmias.
References
White, H. J. (2023). Anatomy, Thorax, Superior Vena Cava. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK545255/








