At Liv Hospital, we understand the importance of innovative treatments for severe aortic stenosis. Balloon aortic valvuloplasty is a minimally invasive intervention that improves blood flow across the narrowed aortic valve, offering a vital solution for patients who cannot undergo direct surgical valve replacement.
We will guide you through the step-by-step process of the BAV procedure, highlighting its benefits and significance in managing aortic stenosis. This advanced treatment restores heart function and improves quality of life, providing a safe and effective solution for patients with severe aortic stenosis.
Key Takeaways
- Balloon aortic valvuloplasty is a minimally invasive treatment for severe aortic stenosis.
- The procedure improves blood flow across the narrowed aortic valve.
- It is particularly beneficial for patients who cannot undergo surgical valve replacement.
- The BAV procedure involves using a catheter with a balloon to widen the valve.
- This treatment restores heart function and improves quality of life.
Understanding Aortic Stenosis and the Role of Intervention
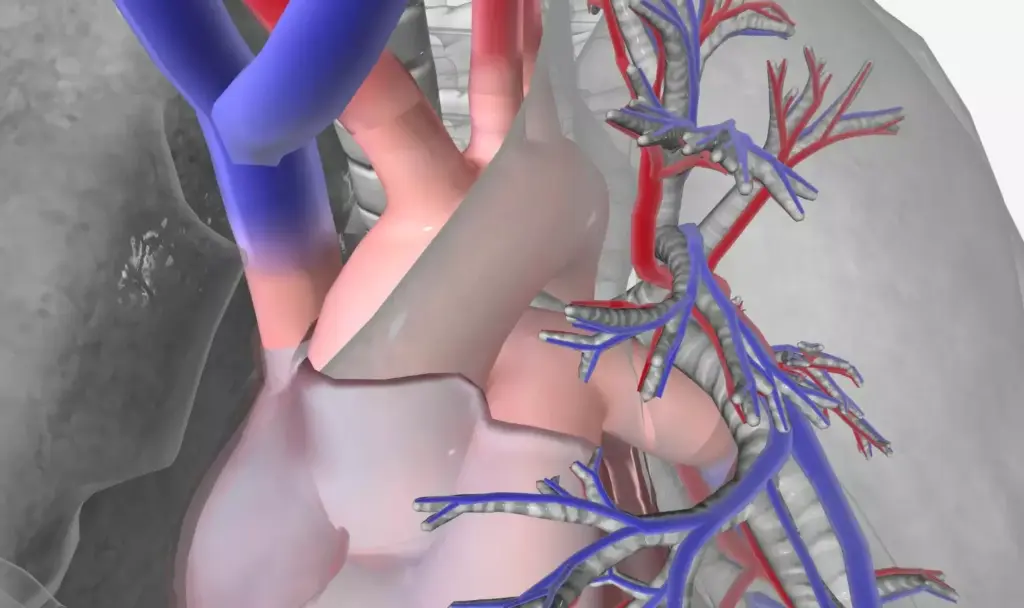
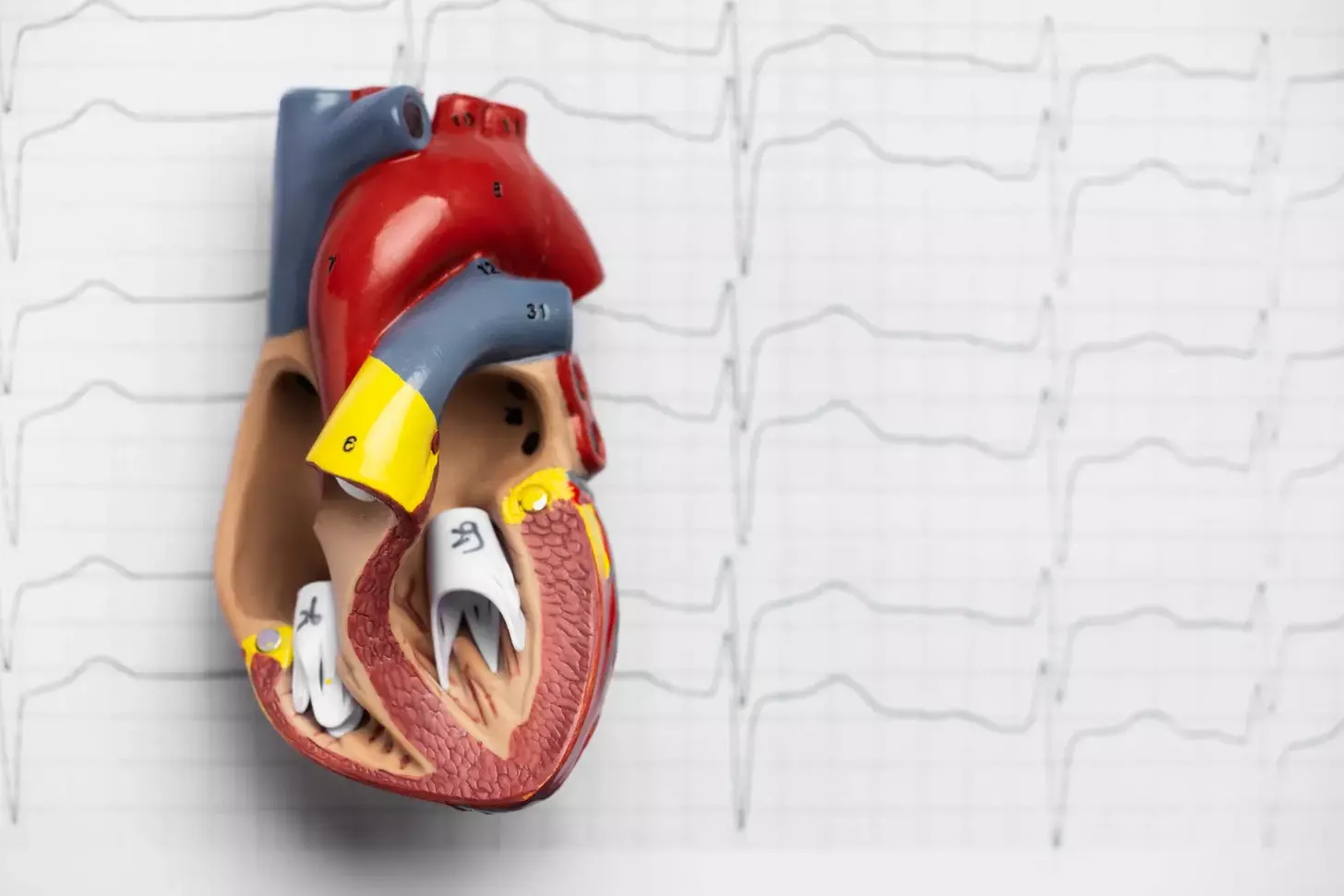
Understanding the complexities of aortic stenosis is crucial for determining the most appropriate intervention strategies. Aortic stenosis is a valvular heart disease characterized by the narrowing of the aortic valve opening, which obstructs blood flow from the left ventricle to the aorta.
Pathophysiology of Aortic Valve Stenosis
Aortic valve stenosis is primarily caused by calcification and degeneration of the valve leaflets, leading to a progressive narrowing of the valve orifice. This narrowing results in increased resistance to blood flow, causing the left ventricle to work harder, potentially leading to left ventricular hypertrophy and, eventually, heart failure if left untreated.
Key factors contributing to the pathophysiology of aortic stenosis include:
- Calcification of valve leaflets
- Degenerative changes
- Congenital abnormalities
- Rheumatic fever
| Pathophysiological Changes | Clinical Implications |
|---|---|
| Left ventricular hypertrophy | Increased risk of heart failure |
| Reduced valve orifice area | Increased resistance to blood flow |
| Potential for arrhythmias | Increased risk of sudden cardiac death |
Clinical Presentation and Diagnosis
The clinical presentation of aortic stenosis can vary significantly among patients. Common symptoms include dyspnea on exertion, angina, and syncope. Diagnosis is typically made through a combination of clinical evaluation, echocardiography, and other imaging modalities to assess the severity of valve narrowing and its impact on cardiac function.
Recent research highlights the utility of Balloon Aortic Valvuloplasty (BAV) as a bridge to transcatheter or surgical aortic valve replacement, or as palliative therapy in high-risk populations. Understanding the role of BAV in the management of aortic stenosis is essential for clinicians to make informed decisions regarding patient care.
The BAV Procedure: Overview and Indications

Understanding the BAV procedure is essential for both cardiologists and patients dealing with aortic stenosis. The balloon aortic valvuloplasty procedure involves passing a catheter with a balloon across the narrowed aortic valve and inflating it, which improves blood flow and reduces the pressure gradient.
What is Balloon Aortic Valvuloplasty
Balloon aortic valvuloplasty (BAV) is a minimally invasive procedure used to widen the aortic valve opening. This technique is particularly beneficial for patients with severe aortic stenosis, a condition characterized by the narrowing of the aortic valve. By inflating a balloon within the valve, we can temporarily improve valve function and alleviate symptoms.
The procedure involves several key steps, including:
- Accessing the aortic valve through a catheter inserted via an artery.
- Guiding the catheter to the valve using imaging techniques.
- Inflating the balloon to widen the valve opening.
Primary and Secondary Indications
The primary indication for BAV is severe aortic stenosis in patients who are at high risk for surgical complications or are considered inoperable. Secondary indications include:
- Bridge therapy to stabilize patients before undergoing more definitive treatments like surgical valve replacement or transcatheter aortic valve replacement (TAVR).
- Palliative care for patients with advanced age or significant comorbidities.
As noted by a leading cardiology expert, “BAV serves as a crucial intervention for patients with severe aortic stenosis, offering symptom relief and potentially improving outcomes.”
“BAV is a valuable tool in our armamentarium against aortic stenosis, providing a bridge to more definitive therapies or serving as a palliative measure in appropriate cases.”
By understanding the indications and benefits of BAV, healthcare providers can better identify suitable candidates for this procedure, ultimately improving patient outcomes.
Patient Selection and Pre-Procedural Evaluation
The success of BAV heavily relies on meticulous patient selection and thorough pre-procedural evaluation. We need to identify patients who will benefit most from this procedure while minimizing potential risks.
Ideal Candidates for BAV
Ideal candidates for BAV are typically those with severe aortic stenosis who are at high risk for surgical aortic valve replacement or are inoperable. Clinical and anatomical factors play a crucial role in determining suitability. Patients with critical aortic stenosis presenting with symptoms such as heart failure, angina, or syncope are considered for BAV, especially if they are hemodynamically unstable.
Data shows that procedural success rates exceed 80 percent, with major complication rates ranging between 2-6 percent. This data underscores the importance of careful patient selection to maintain high success rates and minimize complications.
Required Diagnostic Testing
Before proceeding with BAV, comprehensive diagnostic testing is required to assess the severity of aortic stenosis and the patient’s overall suitability for the procedure. This includes:
- Echocardiography to evaluate valve morphology and function
- Cardiac catheterization to assess coronary artery disease and measure gradients across the aortic valve
- CT angiography or MRI to evaluate the aortic valve and root anatomy
- Exercise stress testing or other functional assessments to gauge the patient’s physical reserve
These diagnostic tests help us to assess the risks and benefits of BAV for each patient, tailoring our approach to individual needs and maximizing the chances of a successful outcome.
By carefully selecting patients and conducting thorough pre-procedural evaluations, we can optimize the outcomes of BAV and provide significant benefits to those suffering from severe aortic stenosis.
Equipment and Materials Required for BAV
BAV requires a specific set of equipment and materials to ensure a safe and successful procedure. The setup in the catheterization laboratory is crucial for the effective execution of BAV.
Catheterization Laboratory Setup
The catheterization laboratory must be equipped with state-of-the-art technology to support the complexities of the BAV procedure. This includes a high-quality fluoroscopy system, hemodynamic monitoring equipment, and a rapid ventricular pacing system to stabilize the balloon during inflation.
We utilize a biplane fluoroscopy system to provide detailed imaging of the aortic valve from multiple angles, enhancing our ability to navigate the valve and position the balloon accurately.
Balloon Catheter Types and Selection
The selection of the appropriate balloon catheter is critical for the success of the BAV procedure. Various types of balloon catheters are available, each with its own characteristics and advantages.
- Truflex Balloon Catheter: Known for its flexibility and trackability.
- Z-Med Balloon Catheter: Offers a range of sizes and is designed for aortic valvuloplasty.
When choosing a balloon catheter, we consider factors such as the patient’s anatomy, the severity of the aortic stenosis, and the desired outcome of the procedure.
Guidewires and Accessory Equipment
Guidewires play a vital role in navigating the vascular system and crossing the aortic valve. We use a variety of guidewires, including stiff and extra-stiff wires, to facilitate the passage of the balloon catheter.
| Guidewire Type | Characteristics | Use in BAV |
|---|---|---|
| Stiff Guidewire | Provides strong support for catheter advancement. | Ideal for navigating tortuous vessels. |
| Extra-Stiff Guidewire | Offers maximum support and stability. | Used for complex cases or when additional support is needed. |
In addition to guidewires, other accessory equipment such as sheaths, dilators, and inflation devices are essential for the successful completion of the BAV procedure.
Pre-Procedure Patient Preparation
As we guide patients through the BAV process, pre-procedure preparation plays a vital role in their overall experience. Proper preparation not only helps in minimizing anxiety but also ensures that the patient is comfortable and well-informed throughout the procedure.
Patient Education and Informed Consent
Patient education is a critical component of pre-procedure preparation. We ensure that patients are thoroughly informed about the BAV procedure, including its benefits, potential risks, and what to expect during and after the intervention. Informed consent is obtained after a detailed discussion, allowing patients to make an educated decision about their care.
Our team takes the time to explain the procedure in a clear and understandable manner, addressing any questions or concerns the patient may have. This process not only empowers patients but also helps in building trust between the patient and the healthcare provider.
Anesthesia and Sedation Options
Choosing the right anesthesia and sedation is crucial for the comfort and safety of the patient during BAV. We evaluate each patient’s individual needs and medical history to determine the most appropriate anesthesia plan. Options may include conscious sedation or general anesthesia, depending on the specific case and patient preference.
Our anesthesiologists work closely with the interventional team to ensure that the anesthesia plan is tailored to the patient’s needs, providing optimal comfort and minimizing risks. The choice of anesthesia is discussed with the patient as part of the informed consent process, ensuring that they are fully aware of the options and their implications.
By focusing on comprehensive patient preparation, we aim to enhance the overall experience and outcomes for patients undergoing BAV. Through education, informed consent, and careful consideration of anesthesia options, we strive to provide the highest level of care.
Performing the BAV Procedure Step by Step
To successfully perform BAV, it’s crucial to follow a step-by-step approach. The BAV procedure is a complex intervention that requires meticulous planning and execution. We will guide you through the key steps involved in performing BAV, from vascular access techniques to rapid ventricular pacing protocols.
Vascular Access Techniques
Obtaining vascular access is the first critical step in the BAV procedure. We typically use the femoral artery for access due to its relatively larger size and easier accessibility. The use of ultrasound guidance has become standard practice to minimize complications and ensure precise access.
The access site is carefully selected and prepared, followed by the insertion of a guidewire and then a sheath. The choice of sheath size depends on the balloon catheter that will be used for the valvuloplasty.
Crossing the Aortic Valve
Crossing the aortic valve is a delicate step that requires precision. We use a combination of fluoroscopic guidance and careful manipulation of the catheter and guidewire to navigate through the valve. The use of a straight or angled catheter, along with a stiff guidewire, facilitates crossing the stenotic valve.
Once the valve is crossed, a superstiff guidewire is often used to provide additional support for the subsequent steps.
Rapid Ventricular Pacing Protocol
Rapid ventricular pacing is a crucial step during BAV to stabilize the balloon during inflation. We achieve this by temporarily pacing the heart at a high rate, usually around 180-220 beats per minute, to reduce cardiac output and minimize balloon movement.
The pacing protocol involves careful monitoring to avoid complications such as ischemia or arrhythmias.
| Step | Description | Key Considerations |
|---|---|---|
| Vascular Access | Obtaining access through the femoral artery | Use of ultrasound guidance, sheath size selection |
| Crossing the Valve | Navigating the catheter and guidewire through the aortic valve | Fluoroscopic guidance, catheter and guidewire selection |
| Rapid Ventricular Pacing | Temporarily pacing the heart at a high rate | Pacing rate, monitoring for complications |
By following these steps and protocols, we can ensure a successful BAV procedure. The recovery time following balloon valvuloplasty is often brief, with most patients being discharged shortly after the procedure.
Balloon Inflation and Valvuloplasty Technique
Balloon inflation and valvuloplasty technique are critical components of the BAV procedure that require meticulous attention to detail. The success of the procedure heavily relies on the precise technique used during balloon inflation and valvuloplasty.
Balloon Positioning Across the Valve
Accurate balloon positioning across the aortic valve is crucial for the success of the BAV procedure. We use fluoroscopic guidance to ensure the balloon is correctly positioned across the stenotic valve. The balloon should be centered and stable during inflation to avoid complications such as valve damage or embolization.
The key steps for balloon positioning include:
- Using fluoroscopy to guide the balloon catheter across the valve
- Ensuring the balloon is centered and stable
- Verifying the position with contrast injections
Inflation and Deflation Sequence
The inflation and deflation sequence is a critical aspect of the valvuloplasty technique. Rapid ventricular pacing is often used during balloon inflation to reduce cardiac output and minimize the risk of balloon migration.
The steps involved in the inflation and deflation sequence are:
- Initiating rapid ventricular pacing
- Inflating the balloon to the recommended pressure
- Maintaining inflation for a few seconds
- Deflating the balloon and stopping rapid ventricular pacing
Assessment of Immediate Results
After completing the valvuloplasty, we assess the immediate results to determine the procedure’s success. This includes evaluating the aortic valve area, gradient, and any potential complications.
The key parameters for assessing immediate results include:
- Aortic valve area calculation
- Transvalvular gradient measurement
- Echocardiographic assessment of valve function
While balloon valvuloplasty can temporarily improve symptoms in patients with aortic valve stenosis, it’s essential to note that restenosis is a common long-term complication. Therefore, close follow-up and further management strategies are crucial.
Managing Complications During and After BAV
Managing complications is a critical aspect of the BAV procedure, requiring a comprehensive understanding of potential risks and effective strategies for mitigation. As we navigate the complexities of BAV, being prepared for complications is essential for ensuring patient safety and optimizing outcomes.
Common Procedural Complications
During the BAV procedure, several complications can arise, including vascular access site complications, cardiac tamponade, and aortic regurgitation. We must be vigilant in monitoring for these potential issues, as timely intervention is crucial in preventing adverse outcomes. Vascular access site complications can often be managed with careful technique and post-procedure care.
Cardiac tamponade, although rare, is a serious complication that requires immediate attention. We are prepared to perform emergency pericardiocentesis to address this potentially life-threatening condition. Aortic regurgitation, another possible complication, necessitates careful balloon sizing and positioning to minimize the risk.
Emergency Interventions and Management
In the event of a complication, having a well-coordinated response plan is vital. For instance, in cases of severe aortic regurgitation or cardiac tamponade, emergency interventions such as pericardiocentesis or the deployment of a covered stent may be necessary. We emphasize the importance of having a multidisciplinary team available to manage such emergencies effectively.
Effective management of BAV complications also involves close monitoring post-procedure. We keep a close watch on patients for signs of vascular complications, heart failure, or other adverse effects, ensuring that any issues are addressed promptly. By being proactive and prepared, we can mitigate the risks associated with BAV and improve patient outcomes.
Post-Procedure Care and Recovery Time
Post-procedure care plays a vital role in the overall success of the BAV procedure, influencing both short-term and long-term outcomes. Effective care after BAV is crucial for managing potential complications, assessing the procedure’s effectiveness, and ensuring a smooth recovery.
Immediate Post-Procedure Monitoring
After the BAV procedure, patients are closely monitored in a hospital setting. We focus on managing any potential complications, such as bleeding, vascular injury, or arrhythmias. Immediate post-procedure monitoring includes:
- Continuous electrocardiographic monitoring to detect any arrhythmias or ischemic changes.
- Frequent blood pressure checks to ensure stability.
- Monitoring for signs of bleeding or vascular complications at the access site.
Hospital Stay Duration
The duration of hospital stay after BAV can vary depending on the patient’s condition and the presence of any complications. Generally, patients are observed for 24 to 48 hours after the procedure. During this time, we assess the effectiveness of the valvuloplasty and manage any post-procedural complications.
The following table outlines the typical hospital stay duration and the factors that influence it:
| Hospital Stay Duration | Influencing Factors |
|---|---|
| 24-48 hours | Uncomplicated procedure, stable patient condition |
| 48-72 hours | Presence of minor complications, need for further monitoring |
| More than 72 hours | Significant complications, need for additional treatment or intervention |
Discharge Planning and Follow-up
Discharge planning is an essential part of post-procedure care. We ensure that patients are stable and have a clear understanding of their post-discharge care instructions. Follow-up appointments are scheduled to monitor the patient’s recovery and the effectiveness of the BAV procedure.
Key aspects of discharge planning include:
- Providing clear instructions on medication management and follow-up care.
- Arranging for follow-up appointments with the patient’s healthcare team.
- Educating patients on signs and symptoms that require immediate medical attention.
By following a structured post-procedure care plan, we can minimize risks and optimize patient outcomes after BAV. Our team is committed to providing comprehensive care and support throughout the recovery process.
Clinical Outcomes and BAV as Bridge Therapy
BAV has emerged as a critical intervention for patients with severe aortic stenosis, offering significant clinical benefits. We will examine the clinical outcomes associated with BAV, including short-term hemodynamic improvements and long-term results, and discuss the role of BAV as a bridge therapy to more definitive treatments like TAVR or surgical valve replacement.
Short-Term Hemodynamic Improvements
One of the immediate benefits of BAV is the improvement in hemodynamic parameters. Studies have shown that BAV can significantly reduce the mean aortic valve gradient and improve the aortic valve area. For instance, a study published in the Journal of the American College of Cardiology found that BAV resulted in a substantial reduction in the mean gradient from 54 mmHg to 29 mmHg.
We observe that the short-term benefits of BAV are crucial for patients with severe aortic stenosis who are hemodynamically unstable. These improvements can be life-saving and provide a window of opportunity for further management.
Long-Term Results and Restenosis
While BAV offers short-term benefits, its long-term efficacy is limited by the occurrence of restenosis. Research indicates that within 6 to 12 months after the procedure, a significant proportion of patients experience restenosis. We must consider this when evaluating the long-term outcomes of BAV.
| Time Frame | Restenosis Rate |
|---|---|
| 6 months | 30% |
| 12 months | 50% |
BAV as Bridge to TAVR or Surgical Valve Replacement
Recent research highlights BAV’s utility as a bridge to transcatheter or surgical aortic valve replacement. For patients who are not immediate candidates for TAVR or surgery due to comorbidities or instability, BAV can serve as a stabilizing measure. We have seen that BAV can improve the clinical condition of patients, making them more suitable candidates for definitive therapies.
In conclusion, BAV is a valuable procedure that offers significant short-term hemodynamic improvements. While long-term results are affected by restenosis, BAV remains a crucial bridge therapy to more definitive treatments. We continue to see advancements in the management of aortic stenosis, with BAV playing a pivotal role.
Conclusion
Balloon aortic valvuloplasty (BAV) is a critical intervention for patients with severe aortic stenosis, particularly those at high risk for surgical complications or seeking a bridge to more definitive therapy. Our discussion has highlighted the importance of understanding the procedure’s benefits and risks.
A comprehensive summary of the BAV procedure reveals its role in providing immediate hemodynamic relief and improving patient outcomes. We have explored the indications, patient selection criteria, and the step-by-step technique involved in performing BAV.
While BAV offers significant benefits, it is not without risks. Common complications and emergency interventions have been discussed, emphasizing the need for careful patient monitoring and post-procedure care. As a bridge therapy, BAV plays a vital role in stabilizing patients before they undergo more definitive treatments like transcatheter aortic valve replacement (TAVR) or surgical valve replacement.
In conclusion on BAV procedure, we emphasize that a thorough understanding of its benefits and risks is crucial for optimal patient management. By summarizing the key aspects of BAV, we provide a summary of BAV benefits and risks, underscoring its value as a treatment option for severe aortic stenosis.
What is Balloon Aortic Valvuloplasty (BAV) and how does it work?
Balloon Aortic Valvuloplasty (BAV) is a minimally invasive procedure used to treat severe aortic stenosis by improving blood flow across the narrowed aortic valve using a catheter with a balloon.
What is aortic stenosis and how does it affect the heart?
Aortic stenosis is a condition characterized by the narrowing of the aortic valve, obstructing blood flow from the heart to the rest of the body, which can lead to symptoms such as chest pain, shortness of breath, and fatigue.
Who are the ideal candidates for the BAV procedure?
Ideal candidates for BAV are patients with severe aortic stenosis who are at high risk for surgical complications or are seeking a bridge to more definitive treatments like TAVR or surgical valve replacement.
What diagnostic tests are required before undergoing BAV?
Required diagnostic tests include echocardiography, cardiac catheterization, and sometimes CT or MRI scans to assess the severity of aortic stenosis and the patient’s overall suitability for BAV.
What are the benefits of BAV as a treatment option for aortic stenosis?
BAV improves blood flow, reduces symptoms, and can serve as a bridge to more definitive treatments, providing relief for patients who are not immediate candidates for surgical valve replacement.
What are the potential complications associated with the BAV procedure?
Potential complications include vascular injury, bleeding, aortic regurgitation, and cardiac complications, which can be managed with appropriate emergency interventions.
How long is the recovery time after BAV, and what is the typical hospital stay?
The hospital stay typically ranges from a few days, and recovery time varies, but most patients require close monitoring and follow-up care to ensure the effectiveness of the procedure.
What are the short-term and long-term outcomes of BAV?
BAV provides short-term hemodynamic improvements, but restenosis can occur; it is often used as a bridge to TAVR or surgical valve replacement for long-term relief.
Is BAV a definitive treatment for aortic stenosis?
BAV is not typically considered a definitive treatment but rather a bridge to more definitive treatments like TAVR or surgical valve replacement, although it can provide significant symptom relief.
How does BAV compare to other treatments for aortic stenosis, such as TAVR?
BAV is a less invasive procedure compared to TAVR or surgical valve replacement and is often used for patients who are at high risk or as a bridge to these more definitive treatments.
References:
- • StatPearls. (n.d.). Balloon valvuloplasty. NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519532/
- • Tumscitz, C. (2021). Balloon aortic valvuloplasty through radial access. Cardiac Interventions Today. https://citoday.com/articles/2021-sept-oct/balloon-aortic-valvuloplasty-through-radial-access
- • EuroIntervention. (n.d.). Single-access balloon aortic valvuloplasty – an overview of contemporary technical improvements. https://eurointervention.pcronline.com/article/tools-and-techniques-single-access-balloon-aortic-valvuloplasty-an-overview-of-contemporary-technical-improvements








