Last Updated on November 25, 2025 by Ugurkan Demir
Learning about heart muscle disease cardiomyopathy is key to taking care of your heart. At Liv Hospital, we help you understand cardiomyopathy and its link to heart failure. This way, you can make better choices for your heart health.
Cardiomyopathy is a group of conditions that harm the heart muscle. It changes the heart’s structure and function. This heart muscle disease weakens the heart, making it hard to pump blood well. Our team is here to explain the causes and effects of cardiomyopathy.
define cardiomyopathy Knowing what cardiomyopathy is and how it can lead to heart failure helps you act early. At Liv Hospital, we’re here to support you in managing your heart health. We want to give you the care and support you need.

Cardiomyopathy is a heart muscle disease. It makes the heart muscle thick or stiff. This affects the heart’s ability to pump blood well.
The term cardiomyopathy comes from Greek words. “Cardia” means heart, “myo” means muscle, and “pathy” means disease. So, it’s a disease of the heart muscle.
The American Heart Association says it’s a disease that makes the heart pump blood poorly. This shows how serious it is for heart function.
In some places, like non-English speaking countries, they use miocardiopatia instead of cardiomyopathy. It’s a translation of the term into other languages. It keeps the same roots.
“The use of miocardiopatia as a term shows how global heart diseases are. It highlights the need for clear, worldwide medical terms.”
Cardiomyopathy is more than just a term. It’s a group of diseases that affect heart health a lot. It includes changes like dilation and hypertrophy in the heart muscle.
It can happen for many reasons, like genetics or toxins. Knowing what cardiomyopathy is helps doctors treat it right.
By looking into the term, its other names, and its roots, we learn a lot. We see how it impacts heart health. And why getting the right medical care is so important.

Cardiomyopathy refers to several heart muscle diseases. They are grouped based on their effects and characteristics. Knowing these types is key for diagnosis and treatment.
Dilated cardiomyopathy makes the heart’s chambers bigger. This reduces the heart’s pumping power. It can be caused by genetics, infections, or toxins.
Key features include a weak heart muscle and low ejection fraction. Symptoms include fatigue, shortness of breath, and leg swelling.
Hypertrophic cardiomyopathy makes the heart muscle thick. This can block blood flow and cause problems. It’s often genetic and can lead to chest pain, dizziness, and fainting.
The main risks are sudden cardiac death, heart failure, and atrial fibrillation.
Restrictive cardiomyopathy stiffens the heart walls. This makes it hard for the heart to fill with blood. It can be caused by amyloidosis and other diseases.
Symptoms include shortness of breath, fatigue, and swelling. These are similar to other cardiomyopathies but have a different cause.
Arrhythmogenic cardiomyopathy replaces heart muscle with fibrous tissue and fat. This disrupts the heart’s electrical system. It can cause dangerous arrhythmias.
The primary risks are ventricular tachycardia and sudden cardiac death. These are big concerns for young people and athletes.
Understanding cardiomyopathy’s spread is key to public health. This heart muscle disease can cause serious illness and death worldwide. We’ll look at how common it is, who gets it, and its economic effects.
Cardiomyopathy is a big reason for heart failure and sudden death globally. It affects about 1 in 250 people worldwide, based on different studies and criteria. This disease puts a big strain on healthcare systems.
Epidemiological studies show it can hit anyone, regardless of age, sex, or ethnicity. Some types are more common in certain groups. It’s a leading cause of heart transplants and is very costly for healthcare.
Cardiomyopathy’s spread varies by type. For example, hypertrophic cardiomyopathy often hits young people, including athletes. Dilated cardiomyopathy is more common in middle-aged men. Restrictive cardiomyopathy can happen at any age but is rarer. There are also ethnic differences in who gets certain types.
Some cardiomyopathies seem to affect men or women more. Knowing this helps us target treatments and improve care.
The cost of cardiomyopathy is huge, including medical expenses and lost work time. In the U.S., heart failure, often caused by cardiomyopathy, costs billions each year. It also affects patients’ and their families’ quality of life.
Managing cardiomyopathy well needs early diagnosis, right treatment, and lifestyle changes. Knowing who gets it and how common it is helps us plan better care and reduce its impact on health.
Cardiomyopathy can come from many sources, like genes, environment, and lifestyle. Knowing these causes helps in preventing, diagnosing, and treating this heart issue.
Genetics play a big part in cardiomyopathy. Some genetic changes can harm the heart muscle. This leads to conditions like hypertrophic or dilated cardiomyopathy. We’ll see how genetic tests can spot those at risk.
Lifestyle and environment also play a role in cardiomyopathy risk. These include:
Cardiomyopathy can also stem from other health issues. For example:
Infections, like viral myocarditis, can cause cardiomyopathy. We’ll look at how these infections impact the heart and their long-term effects.
Understanding cardiomyopathy’s causes and risk factors helps in prevention, diagnosis, and treatment. This knowledge is key to managing the condition well and improving patient care.
Knowing the symptoms and warning signs of cardiomyopathy is key to better treatment. This condition can show itself in many ways, affecting daily life. It’s important to understand these signs.
In the beginning, cardiomyopathy might show mild symptoms. These can be easy to miss or think of as something else. Look out for fatigue, shortness of breath when doing simple tasks, and swelling in the legs, ankles, and feet. Spotting these early signs is vital for quick diagnosis and treatment.
As cardiomyopathy gets worse, symptoms can get much worse too. Signs like chest pain, dizziness or fainting, and palpitations or irregular heartbeats mean it’s time to see a doctor right away. These are serious signs that need quick action.
Each type of cardiomyopathy has its own symptoms. For example, hypertrophic cardiomyopathy can block blood flow, while restrictive cardiomyopathy makes it hard for the heart to fill with blood. Knowing these differences helps doctors diagnose and treat better.
If you or a loved one is showing signs of cardiomyopathy, see a cardiologist. Quick action can make a big difference. A cardiologist can run tests like echocardiograms and electrocardiograms to check the heart and figure out the best treatment.
| Symptom | Description | Action Required |
| Shortness of Breath | Difficulty breathing during normal activities | Monitor and report to doctor |
| Chest Pain | Pain or discomfort in the chest | Seek immediate medical attention |
| Fatigue | Unusual tiredness or lack of energy | Monitor and discuss with doctor |
It’s important to understand how heart muscle damage happens to manage cardiomyopathy well. Cardiomyopathy causes changes in the heart muscle, making it hard to pump blood. We’ll look at the changes in cells and structure, how the heart works less well, and how it gets worse over time.
The heart muscle changes a lot in cardiomyopathy. These changes include thickening, scarring, and changes in the heart’s shape. Hypertrophic cardiomyopathy makes the heart muscle thick, blocking blood flow. On the other hand, dilated cardiomyopathy makes the heart chambers big, making it hard to pump blood.
The heart’s ability to work is affected by these changes. It can’t contract and relax well, leading to less blood being pumped. This can cause symptoms like tiredness, shortness of breath, and swelling in the legs. We’ll see how this affects different types of cardiomyopathy.
How fast heart muscle damage gets worse can vary. Things like the cause of cardiomyopathy, genetics, and lifestyle play a role. Knowing these helps predict the disease’s path and find the right treatment.
It’s key to measure heart muscle damage to diagnose and treat cardiomyopathy. Tests like echocardiography, cardiac MRI, and endomyocardial biopsy give insights into the heart’s state. We’ll talk about these tests and their role in checking heart muscle damage.
Cardiomyopathy and heart failure are closely linked. Cardiomyopathy often leads to heart failure through a complex process. It’s key to understand how this happens.
Cardiomyopathy changes the heart muscle, affecting its function. As it worsens, the heart struggles to pump blood well. This can lead to heart failure.
Many changes happen in the heart cells and structure. These changes harm the heart’s performance. This harm can cause heart failure.
The journey from cardiomyopathy to heart failure takes time. Knowing the stages helps in early treatment.
It’s important to find risk factors and markers. These help predict who might get heart failure. Things like family history, lifestyle, and other health issues matter.
| Risk Factor | Description | Impact on Progression |
| Genetic Predisposition | Family history of cardiomyopathy or heart failure | High |
| Lifestyle Factors | Smoking, alcohol consumption, and physical inactivity | Moderate to High |
| Comorbid Conditions | Hypertension, diabetes, and coronary artery disease | Moderate to High |
Research shows a strong link between cardiomyopathy and heart failure. People with cardiomyopathy face a higher risk of heart failure. The risk depends on the type and severity of cardiomyopathy.
Understanding the link between cardiomyopathy and heart failure is key. It helps healthcare providers manage patients better. By knowing the risks and stages, we can act early and maybe stop heart failure.
Diagnosing cardiomyopathy is a detailed process. It uses clinical checks, advanced imaging, and lab tests. This method helps doctors find and treat cardiomyopathy well.
The first step is a detailed check-up and physical exam. We look at the patient’s health history for signs of cardiomyopathy. This includes symptoms like shortness of breath and fatigue.
A physical exam might show irregular heartbeats or murmurs. These signs help us decide on more tests.
Clinical evaluation is key. It helps us know if more tests are needed and rules out other conditions.
Imaging is a big part of diagnosing cardiomyopathy. Echocardiography checks the heart’s structure and function. It shows chamber size, wall thickness, and valve function.
Cardiac MRI and CT scans also give detailed heart images. These tools help us understand the type and extent of cardiomyopathy.
Laboratory tests are vital for diagnosing cardiomyopathy. Blood tests look for heart damage or inflammation. Genetic testing is also used, mainly for those with a family history of cardiomyopathy.
Genetic testing helps family members. It aids in early detection and management of cardiomyopathy.
When diagnosing cardiomyopathy, we must rule out other conditions. This includes diseases like coronary artery disease or valve disorders. It ensures we get the right diagnosis.
By using clinical checks, imaging, and lab tests, we can accurately diagnose cardiomyopathy. Then, we can create a good treatment plan.
Managing cardiomyopathy requires a detailed treatment plan. This plan may include medication, surgery, and device therapy. The goal is to ease symptoms, slow disease progression, and improve quality of life.
Medications are key in managing cardiomyopathy. Medications like beta-blockers, ACE inhibitors, and ARBs help reduce the heart’s workload. They also improve its pumping efficiency. Sometimes, anti-arrhythmic drugs are used to control irregular heartbeats.
We choose medications based on the patient’s condition. We consider the type and severity of cardiomyopathy, as well as other health conditions.
Surgical or interventional procedures may be needed for some cases of cardiomyopathy. Surgical options include septal myectomy for hypertrophic cardiomyopathy. This involves removing a part of the thickened heart muscle to improve blood flow.
Other procedures, like alcohol septal ablation, may also be considered. This is a minimally invasive procedure that reduces the thickness of the septal wall by injecting alcohol into the artery.
Device therapies are important for managing cardiomyopathy, mainly for those at risk of dangerous arrhythmias. Implantable cardioverter-defibrillators (ICDs) can detect and correct dangerous heart rhythms.
Also, cardiac resynchronization therapy (CRT) devices help improve the heart’s pumping efficiency. They ensure the ventricles contract in sync.
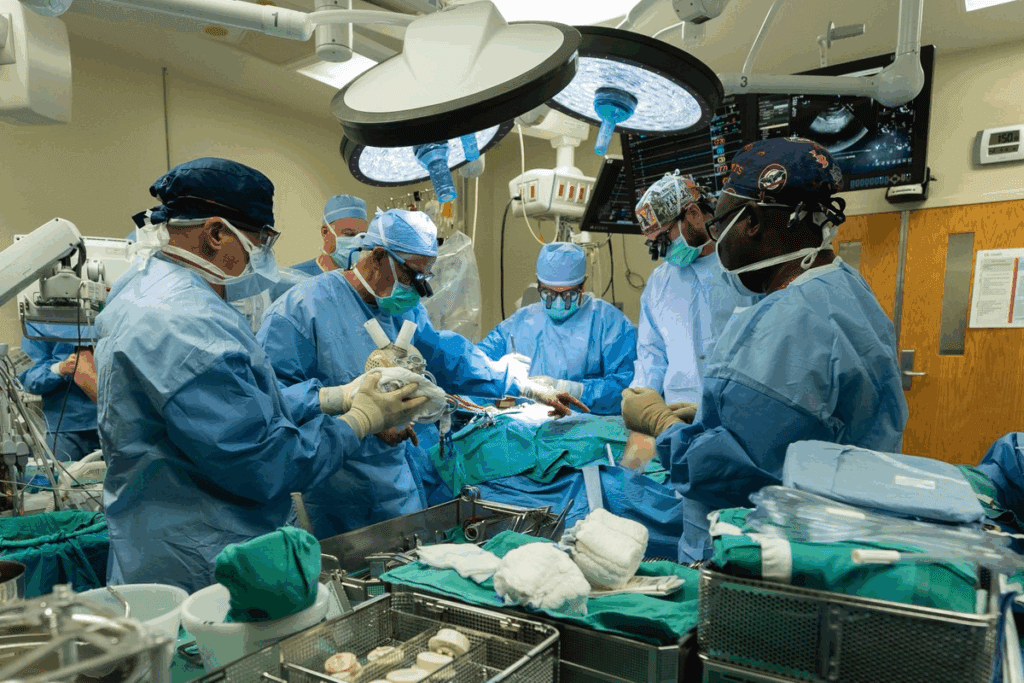
In severe cases, heart transplantation may be considered when other treatments fail. This involves replacing the diseased heart with a healthy donor heart.
For patients waiting for a transplant or as a bridge to recovery, mechanical support devices like left ventricular assist devices (LVADs) can be used. These devices help the heart pump blood more effectively.
A detailed treatment plan for cardiomyopathy requires a team effort. It involves cardiologists, surgeons, and other healthcare professionals. This approach aims to provide the best outcomes for patients.
Living with cardiomyopathy means making lifestyle changes to improve your life and slow the disease. It’s about treating the heart, changing your habits, and keeping an eye on your health.
Eating right is key for heart health. Eat lots of fruits, veggies, whole grains, lean proteins, and healthy fats. Avoid foods that can harm your heart, like foods high in sodium, saturated fats, and sugar.
Exercise is key for managing cardiomyopathy, but it must be safe. Always talk to a doctor before starting or changing your workout. Stick to low to moderate activities like walking, cycling, or swimming. Avoid high-intensity or heavy lifting.
Managing stress is vital when you have cardiomyopathy. Try meditation, deep breathing, or yoga to relax. Also, get help from mental health experts or join support groups for emotional support.
If you have cardiomyopathy, think about family planning and genetic counseling. Talk to a genetic counselor to understand the risks and make informed choices about starting a family.
By making these lifestyle changes, you can manage your cardiomyopathy better. This can improve your life quality and slow the disease’s progress.
Cardiomyopathy is a complex heart condition that can lead to heart failure if not managed well. Recent research has greatly improved our understanding of it. This has led to better ways to diagnose and treat it.
New treatments, including genetic therapies, are being developed. These aim to tackle the root causes of cardiomyopathy. They could even stop or reverse the disease’s progression.
There’s a move towards personalized medicine in treating cardiomyopathy. Treatments are now tailored to each patient’s needs. This, along with better diagnostic tools, is expected to enhance patient outcomes and quality of life.
As research delves deeper into cardiomyopathy, we’ll see new treatments and management strategies emerge. Healthcare providers can then offer top-notch care to patients. This will help reduce heart failure risks and improve health outcomes.
Cardiomyopathy is a disease of the heart muscle. It refers to different conditions that harm the heart’s function.
The term cardiomyopathy comes from Greek words. It means “heart muscle disease.” This condition affects the heart’s ability to work right.
Yes, it can. Cardiomyopathy makes it hard for the heart to pump enough blood. This can lead to heart failure.
There are several types. These include dilated, hypertrophic, restrictive, and arrhythmogenic cardiomyopathy. Each has its own risks and characteristics.
Symptoms vary by type and severity. Common signs are shortness of breath, fatigue, and swelling. Some people may not notice symptoms until it’s advanced.
Doctors use several methods to diagnose it. These include physical exams, imaging like echocardiography, and lab tests. A detailed approach is needed to understand the condition.
Treatment varies based on the condition. It can include medicines, surgery, devices like pacemakers, or heart transplantation in severe cases.
Yes, they can. Eating well, exercising safely, managing stress, and staying mentally healthy are important. Family planning and genetic counseling may also be needed.
Cardiomyopathy can cause heart failure. It’s important to understand how it progresses to manage the condition effectively.
Tests like imaging and lab tests measure damage. These help determine the extent of damage and guide treatment.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!