Last Updated on November 25, 2025 by Ugurkan Demir
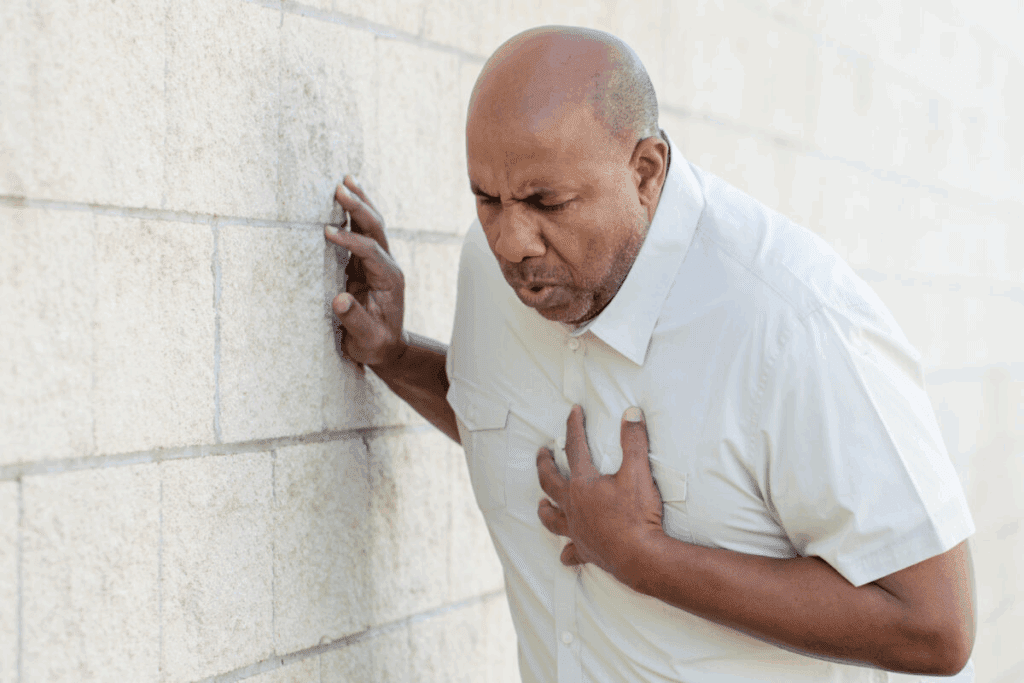
Feeling pain after a heart attack and stent placement can worry you. But, it’s something many people go through. At Liv Hospital, we focus on helping you feel better and recover fully.Understand how long chest pain after heart attack and stent placement.
A stent is a flexible tube in an artery to help blood flow to the heart. It lowers the risk of another heart attack. Even though stents work well, some people might feel discomfort while they heal.
This article will look at why you might feel pain after a stent, how long it lasts, and how to handle it. We aim to help you know what to expect and when to get medical help.

It’s important to know what happens during a heart attack. This helps us see how stent placement helps the heart. A heart attack happens when blood flow to the heart stops, damaging the heart muscle. This usually happens because of a blood clot on atherosclerosis (plaque) in a coronary artery.
During a heart attack, the heart muscle doesn’t get the oxygen and nutrients it needs. This leads to cell death. The damage’s severity depends on where and how long the blockage lasts. Symptoms include chest pain, shortness of breath, nausea, and fatigue.
The goal is to get blood flowing back to the heart. This is done with quick medical actions like clot-busting drugs or stent placement.
Stent placement is key in PCI. It involves putting a small, mesh-like device (stent) in the blocked artery. This opens the artery, letting blood flow to the heart muscle. There are two types of stents: bare-metal and drug-eluting. Drug-eluting stents release medicine to prevent the artery from narrowing again.
Stent placement offers several benefits:
Recovering from a heart attack and stent placement takes time. Right after, patients are watched for any issues in the hospital. Most leave within a few days and start to get back to normal slowly.
It’s vital to follow a detailed recovery plan. This includes:
Knowing the recovery process and following the guidelines can greatly improve outcomes. It also lowers the chance of future heart issues.

It’s important to know why chest pain happens after a heart attack and stent. This pain can be scary, but it’s usually because your body is healing.
One main reason for chest pain after a stent is the artery’s healing. When a stent is put in, it can make the artery bigger. This is part of healing, as it helps blood flow better to the heart.
As the artery heals, you might feel some pain. This pain shows your body is getting used to the stent and healing.
Muscle irritation and inflammation also cause chest pain. The way the heart is accessed can irritate nearby tissues and muscles.
This irritation can cause inflammation, leading to pain. The catheter used in the procedure can also hurt the artery, adding to the pain.
Several things during the procedure can cause pain. These include the stent’s size and type, where it’s placed, and how complex the procedure is.
Patients might feel chest tightness or discomfort from the stent. This usually goes away as your body gets used to it.
Talking to your doctor about your pain is key. They can help figure out why you’re feeling pain and guide you on what to do next.
Knowing how long chest pain lasts after a stent is key for patient care. The time it lasts can change a lot, based on the procedure and the patient’s health.
Right after a stent is placed, patients often feel chest pain. This pain comes from the artery expanding and starting to heal. Most say this pain is bearable and gets better in the first week. They might feel tightness or mild pain in their chest.
In the first 1 to 10 weeks, chest pain is common. Studies show many patients feel chest pain or tightness. It’s normal for many during recovery. The pain usually goes away as the artery heals and the body gets used to the stent.
Research shows how common chest pain is after a stent. Up to 68% of patients feel chest pain, tightness, or discomfort in the first ten weeks. This highlights the need for patient education and support during recovery. Knowing they’re not alone helps patients deal with their recovery better.
The time chest pain lasts after a stent can vary. But with the right care and understanding, patients can handle it better. Healthcare providers should give detailed guidance and support to manage symptoms and ensure the best results.
Understanding normal chest pain after a stent helps patients feel better. They often wonder about chest pain during recovery. This can make them anxious.
Normal chest pain after a stent can feel different. We’ll look at the types of sensations, where they happen, and if they spread.
After a stent, patients might feel various sensations. These can include:
These feelings come from the body’s reaction to the stent and healing. It’s important to know these feelings are usually normal during recovery.
The pain from a stent can be in the chest. Sometimes, it spreads to other areas like:
This pattern is similar to heart attack pain. But, in recovery, it’s usually about healing.
It can be hard for patients to tell normal chest pain from pre-stent angina. Angina usually happens when you’re active or stressed. It goes away with rest or medicine. But, post-stent pain can happen when you’re resting and might not follow the same patterns.
Knowing the difference is key for managing worries and knowing when to see a doctor. If you’re unsure about chest pain after a stent, talk to your doctor.
After getting a stent, people often feel more symptoms than expected. These symptoms are usually part of the healing process. Knowing about them can help you feel better and recover faster.
Shortness of breath, or dyspnea, is a common symptom after a stent. It can happen because the heart is adjusting to better blood flow or because of the procedure’s effects. A study in the Journal of the American College of Cardiology found that up to 20% of patients may experience some degree of shortness of breath after a stent.
How long you feel short of breath varies. Usually, it goes away in a few weeks as your heart gets used to the change. But if it doesn’t get better or gets worse, you should talk to your doctor.
| Cause | Typical Duration | Action |
| Adjustment to improved blood flow | A few weeks | Monitor symptoms |
| Residual effects from the procedure | Variable | Consult healthcare provider if persistent |
Fatigue is another common symptom after a stent. The body’s response to the procedure and the heart condition can make you feel weak and tired. As one patient said,
“I was surprised by how exhausted I felt after my stent placement. It was as if my body was recovering from a significant event, which, in hindsight, it was.”
Resting and slowly getting back to normal activities is important during this time. Most people start to feel more energetic in a few weeks. But, it can take longer to fully recover.
The emotional impact of a stent placement should not be ignored. Anxiety and depression are common as people adjust to their condition and its health implications.
Talking about these feelings is important. You can join support groups, see a counselor, or talk to your doctor. Recognizing the emotional side of recovery helps manage it better.
Understanding these symptoms can greatly help in the recovery process. If you have any worries or questions, always reach out to your healthcare team for help and support.
Chest pain after a stent is common, but some signs might mean trouble. It’s important to know these signs to get help fast.
In-stent restenosis happens when the artery gets narrow again after a stent. It can cause pain like angina, often when you’re active or stressed. If your chest pain keeps coming back or gets worse, see your doctor right away.
New blockages can form in other arteries, not just the stented one. These can cause pain or discomfort, which might feel different from before. Keeping an eye on risk factors helps prevent these blockages.
Stent thrombosis is a rare but serious issue where a blood clot forms in the stent. It can cause severe chest pain and is a medical emergency. Look out for sudden, intense pain in your chest, and get help fast.
To better understand the possible complications and their symptoms, let’s look at the following table:
| Complication | Symptoms | Urgency |
| In-Stent Restenosis | Chest pain on exertion, similar to angina | Monitor and consult healthcare provider |
| New Arterial Blockages | Chest pain or discomfort, potentially different from pre-stent angina | Manage risk factors, consult healthcare provider |
| Stent Thrombosis | Sudden, severe chest pain | Immediate medical attention required |
It’s key to spot these complications’ signs and get medical help to stay healthy after a stent.
Chest pain or discomfort months after a stent is placed can be worrying. Yet, it’s a common issue we need to grasp. Up to 20% of patients face recurring chest pain, often tied to heart disease.
Several reasons can cause chest pain after a stent. Underlying heart disease is a big factor, as the original condition might not be fully treated. The body’s healing process and reaction to the stent can also lead to discomfort.
Having a stent doesn’t mean all heart-related pain goes away. Patients might feel angina or chest pain again. This could be due to new blockages or the stent itself narrowing.
Chest pain three months or more after a stent needs a close look. By then, the healing should be done. Any new symptoms might point to other problems.
| Potential Causes | Characteristics |
| In-stent Restenosis | Narrowing of the stented artery, potentially causing angina-like symptoms |
| New Arterial Blockages | Development of new blockages in other coronary arteries |
| Non-Cardiac Causes | Musculoskeletal or gastrointestinal issues that may mimic cardiac pain |
It’s key to tell normal post-stent feelings from serious symptoms. Know the details of your chest pain, like where it is, how bad it is, and what makes it worse.
If your chest pain is severe, lasts a long time, or comes with other signs like trouble breathing, feeling dizzy, or nausea, get help right away.
Understanding why chest pain can last long after a stent helps patients manage their recovery. It also tells them when to see a doctor again.
Learning how to handle post-stent chest pain can really help with recovery. It’s key to find good ways to ease symptoms and get better faster.
Medicines are very important for dealing with chest pain after a stent. Antiplatelet therapy stops blood clots from forming around the stent. Other drugs like beta-blockers, nitrates, and calcium channel blockers help by making blood flow better to the heart.
A study in the Journal of the American College of Cardiology showed that the right antiplatelet therapy cuts down on stent thrombosis and heart attacks in people with heart disease.
“The use of antiplatelet therapy has changed how we care for patients with stents, greatly lowering the chance of bad heart events.”
— Medical Expert, Cardiologist
| Medication | Purpose | Common Side Effects |
| Aspirin | Antiplatelet therapy | Bleeding, stomach upset |
| Clopidogrel | Antiplatelet therapy | Bleeding, rash |
| Beta-blockers | Reduce heart workload | Fatigue, dizziness |
Making lifestyle changes is also key in managing chest pain after a stent. Dietary changes can lower heart disease risk. Eating more fruits, veggies, and whole grains, and less saturated fats and cholesterol is advised.
It’s also good to stay active, but it must fit your health and abilities. A doctor can help make an exercise plan that’s right for you.
It’s important to know when to get medical help. Severe or getting worse chest pain, trouble breathing, or other serious symptoms mean you should call your doctor right away.
By using medicines, making lifestyle changes, and knowing when to get help, you can manage post-stent chest pain well. This helps improve your recovery.
It’s key to know why chest pain happens after a heart attack and stent placement. At Liv Hospital, we focus on full care during recovery. This helps patients get better smoothly.
Patients should understand what’s normal and possible complications after a stent. Managing chest pain well needs the right medicine and changes in lifestyle.
We urge patients to keep up with their care and talk to their doctors about any issues. This way, they can recover better and feel better overall. It helps them handle chest pain well.
Chest discomfort after a stent usually lasts a few days to weeks. Most people see big improvements in 1-10 weeks.
Chest pain can come from healing, muscle irritation, or the stent type and procedure complexity.
Yes, shortness of breath is common after a stent. It’s often due to the body’s reaction or temporary heart changes. But, always talk to your doctor about it.
Normal pain is dull, tight, or sharp, and might spread to the arm, neck, or jaw. But, watch out for severe, lasting, or getting worse pain. Also, be cautious of dizziness, nausea, or trouble breathing.
Look out for signs like in-stent restenosis, new blockages, or stent thrombosis. These can show as more pain, shortness of breath, or other bad signs. If you see these, get help fast.
Yes, some people feel chest pain months later. It’s key to talk to your doctor to see if it’s healing or a problem.
To manage pain, try medicines, change your diet, and exercise. Also, know when to see a doctor. A good plan can help you feel better.
Chest pain can be from not fully opening the artery, microvascular issues, or other health problems. Talk to your doctor to figure out why and how to fix it.
Eat well, exercise, manage stress, and quit smoking. These steps can boost your heart health and lower future risks.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!