Third-degree heart block, also known as third-degree AV block, is a serious heart condition. It happens when electrical signals between the heart’s chambers are completely blocked. This makes the atria and ventricles beat on their own, leading to serious problems if not treated quickly.Explore 7 key complete block ECG findings and how they help identify third degree heart block quickly.
It’s important to understand the ECG findings in third-degree heart block for accurate diagnosis and treatment. The ICD-10 code for this condition is I44.2, showing it’s a complete atrioventricular block. At Liv Hospital, we use international standards to give precise care to patients with third-degree heart block.
Key Takeaways
- Third-degree heart block is a life-threatening condition requiring immediate medical attention.
- ECG findings are critical for diagnosing third-degree AV block.
- The condition is characterized by total atrioventricular dissociation.
- The ICD-10 code for third-degree heart block is I44.2.
- Prompt diagnosis and treatment are essential to prevent severe complications.
Understanding Complete Heart Block: Pathophysiology and Significance

Complete heart block, also known as third-degree atrioventricular (AV) block, is a serious heart condition. It happens when the heart’s electrical signals don’t sync up. This means the heart’s upper and lower chambers beat on their own.
Definition and Mechanism of Third-Degree AV Block
Third-degree AV block means there’s no electrical connection between the heart’s upper and lower parts. This blockage stops signals from the upper chambers from reaching the lower chambers. As a result, the heart’s upper and lower parts beat independently, causing atrioventricular dissociation.
Epidemiology and Clinical Importance
The occurrence of third-degree AV block varies. It’s often linked to heart disease, scarring in the heart’s electrical system, or complications from heart surgery. It’s serious because it can cause slow heart rates. This can lead to symptoms like dizziness, fainting, or even heart failure.
Comparison with First and Second-Degree Heart Blocks
First-degree AV block means there’s a delay in the heart’s electrical signals. Second-degree AV block means these signals fail to pass through sometimes. But third-degree AV block is different because there’s no signal passing through at all. Knowing these differences is key for correct diagnosis and treatment.
| AV Block Type | AV Conduction Characteristic | Clinical Significance |
| First-Degree | Delayed AV conduction | Often asymptomatic, may progress to higher degrees of block |
| Second-Degree | Intermittent failure of AV conduction | May be symptomatic; some types are more likely to progress to third-degree AV block |
| Third-Degree | Complete block of AV conduction | Often symptomatic with significant bradycardia; requires prompt treatment |
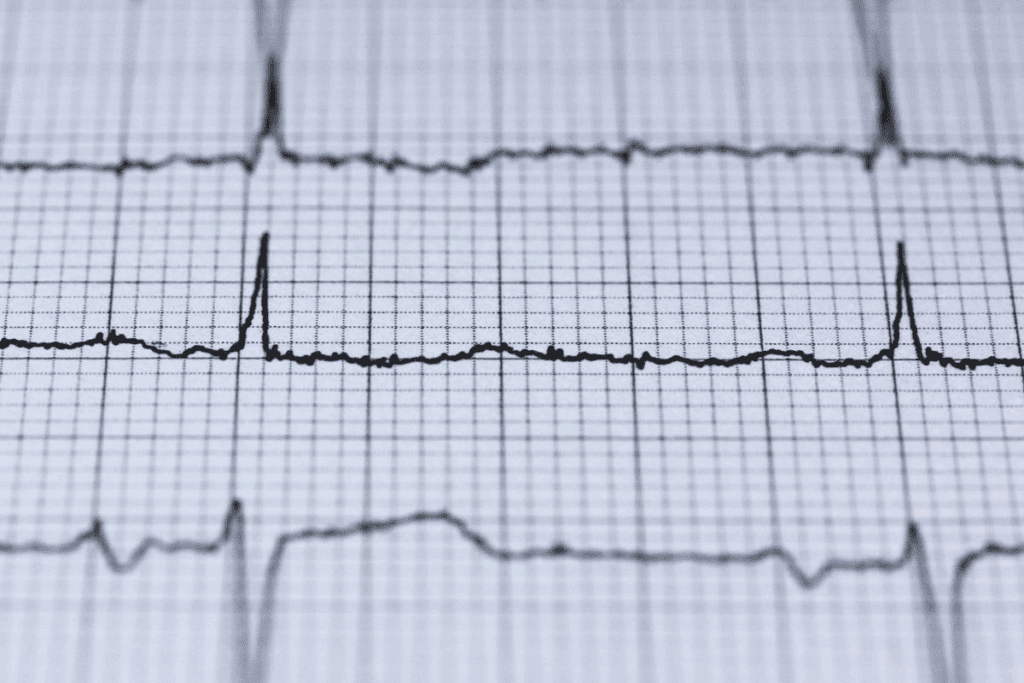
The Complete Block ECG: Fundamental Characteristics
Understanding the electrocardiogram (ECG) of complete heart block is key for correct diagnosis and treatment. The ECG of third-degree AV block shows unique features that help identify it.
Atrioventricular Dissociation on ECG
One key feature of complete heart block on ECG is atrioventricular dissociation. This means P waves and QRS complexes happen on their own. On a 3rd degree heart block ECG strip, you’ll see more P waves than QRS complexes, with no set pattern between them.
P Wave and QRS Complex Relationship
In complete AV block, the P waves and QRS complexes don’t follow each other. The atrial rate is usually faster than the ventricular rate. P waves may go through the QRS complexes without affecting them. This is a major sign of third-degree AV block.
Typical Heart Rate Patterns
The ventricular rate in third-degree AV block is usually slow, between 30-40 bpm. The rhythm can be steady or not, depending on the escape rhythm’s source. A steady ventricular rate might mean a junctional escape rhythm. An irregular rate could point to a ventricular escape rhythm.
| ECG Feature | Characteristic in 3rd Degree AV Block |
| P Wave and QRS Relationship | No consistent relationship; P waves “march through” QRS complexes |
| Atrial Rate vs. Ventricular Rate | Atrial rate > Ventricular rate |
| Ventricular Rate | Typically 30-40 bpm |
It’s vital to recognize these ECG features for diagnosing complete heart block and managing it. Look for atrioventricular dissociation, a slow ventricular rate, and no set P wave and QRS complex relationship. Healthcare professionals need to know these signs well.
Key Finding #1: P Waves and QRS Complex Dissociation
In third-degree atrioventricular (AV) block, a key ECG finding is the separation of P waves and QRS complexes. This separation shows that the atria and ventricles beat on their own.
Identifying Independent Atrial and Ventricular Activity
To spot independent atrial and ventricular activity on an ECG, we look for P waves not linked to QRS complexes. This means P waves and QRS complexes have different rates and rhythms, with no connection between them.
For example, seeing more P waves than QRS complexes on an ECG strip points to third-degree AV block. The atria beat faster than the ventricles, and there’s no sync between them.
P Wave Frequency vs. QRS Frequency
It’s important to compare P wave and QRS complex frequencies to spot third-degree AV block. Usually, P waves beat more often than QRS complexes, showing the atria beat faster than the ventricles.
| ECG Component | Frequency in Third-Degree AV Block | Typical Observation |
| P Waves | Higher Frequency | Atrial rate is typically between 60-100 BPM |
| QRS Complexes | Lower Frequency | Ventricular rate is typically between 30-40 BPM |
Diagnostic Significance of Complete Dissociation
The complete separation of P waves and QRS complexes is very important for diagnosis. It shows a total break in the electrical connection between the atria and ventricles.
This finding is key for doctors. It helps them decide on treatment, like getting a pacemaker.
Key Finding #2: Bradycardia in Third Degree Heart Block
Bradycardia is a key finding in third-degree heart block. It shows up as a heart rate between 30-40 bpm. This slow heart rate can have big effects on the patient’s health and how they are treated.
Typical Ventricular Rates
In third-degree AV block, the heart rate is usually between 30-40 bpm. This is much slower than the normal heart rate of 60-100 bpm. The ventricles have to rely on an escape pacemaker because the normal pathway is blocked.
Hemodynamic Consequences of Slow Heart Rate
The slow heart rate in third-degree AV block can cause problems. It can lead to less blood being pumped, causing symptoms like dizziness, fatigue, and shortness of breath. In serious cases, it can cause big problems with blood flow, needing quick medical help.
Differentiating from Other Causes of Bradycardia
Bradycardia is a sign of third-degree AV block, but it can also be caused by other things. It’s important to tell third-degree AV block apart from other causes to get the right treatment.
| Condition | Typical Heart Rate | ECG Characteristics |
| Third-Degree AV Block | 30-40 bpm | Complete dissociation between P waves and QRS complexes |
| Sinus Node Dysfunction | Variable, often | P wave morphology may be abnormal; may have sinus pauses or arrest |
| Medication-Induced Bradycardia | Variable, often | May have normal P wave and QRS morphology; often associated with PR prolongation |
It’s key to know the ECG signs and the patient’s situation to correctly diagnose third-degree AV block. This helps to tell it apart from other reasons for slow heart rate.
Key Finding #3: Escape Rhythms and QRS Morphology
Escape rhythms are key in third-degree AV block. They help keep the heart beating when the usual pathway is blocked. The details of these rhythms tell us a lot about the block’s location and type.
Junctional Escape Rhythms and Narrow QRS Complexes
A junctional escape rhythm starts at the AV junction. It leads to a narrow QRS complex on the ECG. This is because the electrical signal goes through the normal ventricular pathway. Third-degree AV block with junctional escape rhythm shows a narrow QRS, pointing to a closer block.
Ventricular Escape Rhythms and Wide QRS Complexes
A ventricular escape rhythm starts in the ventricular muscle, causing a wide QRS complex. This is because the signal doesn’t follow the usual fast pathway. A wide QRS in third-degree AV block means a more serious block.
Prognostic Implications of Different Escape Rhythms
The type of escape rhythm matters a lot for the patient’s future. Junctional rhythms usually mean a better outlook than ventricular ones. This is because ventricular rhythms often point to more serious heart issues.
Looking at escape rhythms and QRS shapes helps doctors understand the heart’s problem better. Knowing if it’s junctional or ventricular is key. It helps decide how to treat the patient and what to expect.
Key Finding #4: Rhythm Stability in 3rd Degree AV Block
Understanding rhythm stability in third-degree AV block is key for accurate diagnosis and treatment. The ventricular rhythm can be regular or irregular. This helps doctors diagnose better.
Regular vs. Irregular Ventricular Rhythms
In third-degree AV block, ventricular rhythms can vary. A regular rhythm means a stable escape rhythm. An irregular rhythm might show variability or other arrhythmias.
Stability as a Diagnostic Clue
The rhythm’s stability is a big clue for doctors. A stable rhythm often means a dominant pacemaker. But, an unstable rhythm might point to a more complex issue.
Variations in Escape Rhythm Stability
Escape rhythms in third-degree AV block can change a lot. The location of the pacemaker, heart disease, and treatments all play a role. These factors affect how stable the rhythm is.
| Characteristics | Regular Ventricular Rhythm | Irregular Ventricular Rhythm |
| Escape Pacemaker Location | Junctional or Ventricular | Variable or Multiple Sites |
| Underlying Heart Disease | Less likely to be severe | More likely to be severe |
| Prognostic Implication | Generally more stable | Generally less stable |
It’s important to know about rhythm stability in third-degree AV block. Patients often need urgent pacing due to instability.
Key Finding #5: ECG Changes During Acute Myocardial Infarction
Third-degree AV block is a serious issue that can happen during a heart attack. It can affect up to 10 percent of heart attack cases. This makes it very important for doctors to watch for it.
Association with Inferior Wall MI
Third-degree AV block often happens with heart attacks in the lower part of the heart. This is because the artery that supplies the AV node is usually affected. The block usually goes away once the heart attack is treated.
Association with Anterior Wall MI
When third-degree AV block happens with heart attacks in the front part of the heart, it’s a bad sign. It means the heart damage is severe. This can lead to a higher chance of death because of the bigger heart damage.
Temporary vs. Permanent Block in MI Settings
The type of third-degree AV block during a heart attack can be either short-term or permanent. It depends on how much damage there is to the heart’s electrical system. Short-term blocks are more common in lower heart attacks, while permanent blocks are more likely in front heart attacks.
It’s key for doctors to know how third-degree AV block relates to heart attack location. They need to watch ECG changes closely. This helps them spot and treat this serious problem quickly.
Key Finding #6: Clinical Manifestations and ECG Correlation
It’s important to know how third-degree AV block shows up in patients. This helps doctors match symptoms with ECG results and choose the right treatment. Symptoms can range from mild to severe and even life-threatening.
Syncope and Stokes-Adams Attacks
Syncope, or Stokes-Adams attacks, is a serious symptom of third-degree AV block. It happens when the heart beats too slow, causing a drop in blood flow to the brain. This leads to a sudden loss of consciousness. The ECG shows a very slow heart rhythm. Quick action is needed to stop more episodes and avoid harm.
“Stokes-Adams attacks are a medical emergency requiring immediate attention to prevent further episodes and possible complications.”
Heart Failure Signs
Third-degree AV block can also cause heart failure symptoms. These include feeling tired, shortness of breath, and swelling in the legs. The ECG will show a slow heart rate and might have a wide QRS complex. Spotting heart failure signs early is key to acting fast.
| Clinical Manifestation | ECG Correlation |
| Syncope/Stokes-Adams Attack | Very slow ventricular escape rhythm |
| Heart Failure Signs | Slow ventricular rate, often with wide QRS |
| Asymptomatic Presentation | Variable; may show typical 3rd degree AV block pattern |
Asymptomatic Presentation Possibilities
Some people with third-degree AV block don’t show any symptoms. They might only find out during an ECG for another reason. The ECG will show the usual signs of atrioventricular dissociation. Even without symptoms, it’s important to check and might need a pacemaker to avoid problems later.
In summary, third-degree AV block can show up in many ways, and matching symptoms with ECG results is key. Whether it’s syncope, heart failure, or no symptoms at all, knowing the ECG signs is vital for the right care.
Key Finding #7: Therapeutic Interventions and ECG Monitoring
Managing third-degree AV block requires careful treatment. The main goal is to get the heart rhythm stable and ensure it pumps well.
Temporary Pacing Indications
Temporary pacing is often needed for third-degree AV block. This is true when it happens with heart attacks or drug side effects. It helps keep the heart rate steady until a permanent fix can be found.
Permanent Pacemaker Requirements
Most patients with third-degree AV block need a permanent pacemaker. The choice depends on symptoms, heart disease, and other health issues.
Post-Intervention ECG Changes
After getting a pacemaker, ECG checks are key. They show how well the pacemaker is working and how the patient is doing. Adjustments might be made to the pacemaker settings.
| Therapeutic Intervention | Indications | ECG Changes |
| Temporary Pacing | Acute MI, drug toxicity | Temporary paced rhythm |
| Permanent Pacemaker | Chronic third-degree AV block | Paced complexes on ECG |
ECG monitoring is vital for managing third-degree AV block long-term. It helps doctors adjust treatments and quickly handle any problems.
Conclusion: Critical Importance of Recognizing Complete Heart Block
It’s key to spot complete block ECG patterns to diagnose and treat third-degree AV block. We’ve covered the main points, like atrioventricular dissociation, slow heart rate, and escape rhythms. Knowing these details is vital for the best care of patients.
Quick action and treatment for 3rd degree heart block are critical to avoid bad outcomes. Seeing third degree heart block on an ECG means a serious problem that needs fast help. Doctors can start the right treatment, like pacemakers, by knowing the ECG signs.
Managing complete heart block well needs a deep understanding of its ECG signs. We stress the need for ongoing learning and practice in reading ECGs. This ensures accurate diagnosis and treatment of this serious condition.
FAQ
What is third-degree AV block, and how is it diagnosed on an ECG?
Third-degree AV block, also known as complete heart block, is when the heart’s upper chambers can’t send signals to the lower chambers. It’s seen on an ECG by P waves and QRS complexes acting alone.
What are the typical ECG findings in third-degree heart block?
ECGs show atrioventricular dissociation, meaning P waves and QRS complexes act alone. The heart rate is usually slow, between 30-40 beats per minute.
How do you differentiate third-degree AV block from other causes of bradycardia?
Third-degree AV block is different from other slow heart rates because of atrioventricular dissociation. This is seen on an ECG, where P waves and QRS complexes are independent.
What is the significance of escape rhythms in third-degree AV block?
Escape rhythms are key in third-degree AV block. They can cause narrow or wide QRS complexes. The type of rhythm affects treatment and outlook.
How does third-degree AV block affect heart rate, and what are the hemodynamic consequences?
Third-degree AV block makes the heart rate slow, usually 30-40 beats per minute. This can lead to less blood flow and symptoms like fainting and heart failure.
What are the clinical manifestations of third-degree AV block, and how do they correlate with ECG findings?
Symptoms of third-degree AV block range from fainting to heart failure. These symptoms match what’s seen on an ECG. This shows why quick diagnosis and treatment are vital.
What are the therapeutic interventions for third-degree AV block, and how is ECG monitoring used in patient management?
Treatments include temporary pacing and permanent pacemakers. ECG monitoring is key. It helps see if treatments work and guides further care.
Can third-degree AV block occur in the context of acute myocardial infarction?
Yes, third-degree AV block can happen with heart attacks. The impact varies based on the heart area affected. It’s important to know if the block is temporary or permanent.
What is the role of ECG in diagnosing and managing third-degree AV block?
ECGs are essential for diagnosing and managing third-degree AV block. They show important details like atrioventricular dissociation and heart rate. This helps doctors make treatment plans and check how well treatments work.
References
- Lung, K., & Lui, F. (2023). Anatomy, Abdomen and Pelvis: Arteries. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK525959/









