Last Updated on November 25, 2025 by Ugurkan Demir

When you get a prostate cancer diagnosis, knowing your treatment options is key. Androgen deprivation therapy (ADT), or hormone therapy, is a main treatment. It lowers androgen levels to slow cancer growth.
At Liv Hospital, we focus on both medical results and patient care. We make sure you get care that’s backed by science. By lowering testosterone, ADT stops prostate cancer cells from growing. This makes it a vital treatment for advanced prostate cancer.
Understanding androgen deprivation is key to seeing its role in fighting prostate cancer. Androgen deprivation therapy (ADT) is a mainstay in treating prostate cancer, mainly for those with advanced or non-metastatic disease. Studies show many patients with non-metastatic prostate cancer use ADT, showing its vital role in treatment.
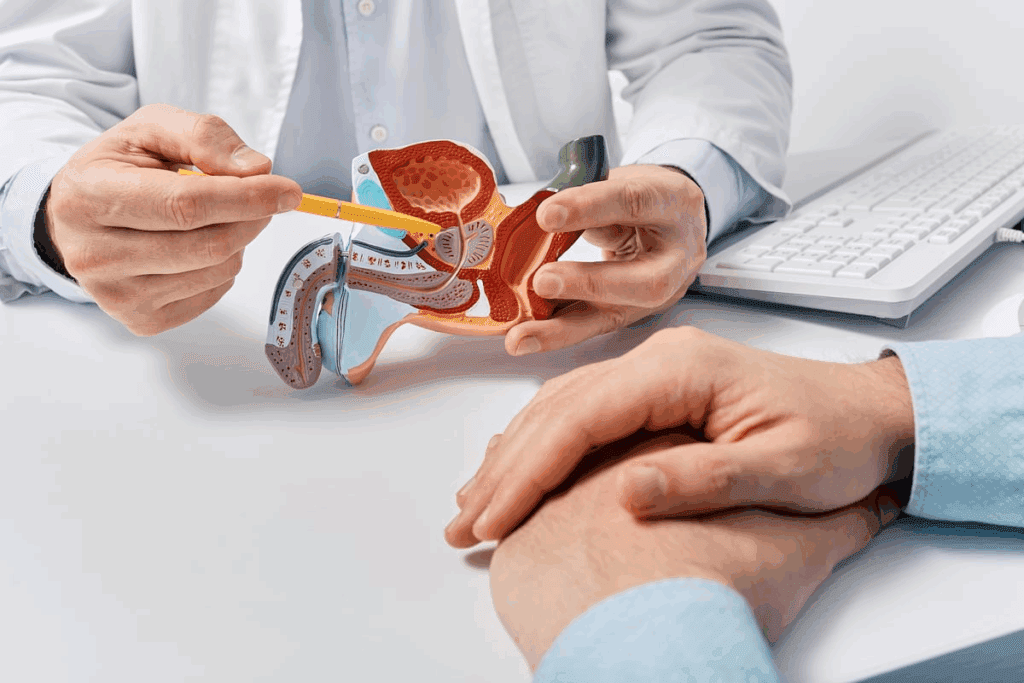
Prostate cancer cells rely on androgen hormones like testosterone to grow. This reliance is a big factor in the disease’s development and spread.
Androgens, like testosterone, are vital in prostate cancer’s growth and spread. These hormones help prostate cells, including cancerous ones, grow. Androgens are key for prostate cancer cells to survive and multiply, making them a prime target for treatment.
Research shows lowering androgen levels can slow prostate cancer cell growth and spread. This is done through androgen deprivation therapy, which reduces androgen hormones in the body.
ADT’s strategy of reducing hormone levels is key to slowing cancer growth. Lowering androgen levels makes it harder for prostate cancer cells to grow and multiply.
The benefits of ADT are many, including:
By grasping how androgen deprivation works, we can better see its role in managing prostate cancer.
Prostate cancer treatment often uses ADT. This includes several ways to lower androgen levels or block their effects. The choice depends on the cancer stage, patient health, and personal choices.
Medical castration uses drugs to lower testosterone levels. LHRH agonists and antagonists are the main drugs. LHRH agonists first raise then lower testosterone levels. LHRH antagonists immediately lower levels without a surge.
These drugs are given by injection or implant. They are used monthly, every 3 months, or every 6 months, based on the type.
Surgical orchiectomy removes the testicles to lower testosterone. It’s for those needing quick androgen reduction or prefer surgery over medication.
Though effective, it’s less chosen than medical castration. This is because it’s permanent and can affect a person’s mental health.
Combined androgen blockade (CAB) uses both medical castration and anti-androgen drugs. Anti-androgens block androgen action at the cell level. This complements lowering testosterone production.
CAB is for patients with advanced disease or needing stronger treatment. Studies show it can improve survival in metastatic hormone-sensitive prostate cancer.
LHRH agonists are key in treating prostate cancer. They lower testosterone, a hormone that helps cancer grow. This slowdown helps control the disease.
At first, LHRH agonists increase testosterone production. But, they eventually reduce it. This makes it hard for prostate cancer cells to grow.
Medical Expert, a renowned oncologist, says, “LHRH agonists are vital in prostate cancer treatment. They help control the disease by lowering hormone levels.” Studies have shown they are effective, making them a reliable choice for both patients and doctors.
There are several LHRH agonists for prostate cancer treatment. These include:
These are given as injections. The frequency depends on the type. Some are given prostate cancer injections every 6 months, making treatment easier for patients.
LHRH agonists are a cornerstone in prostate cancer treatment. They are key in hormone therapy for the disease.
LHRH antagonists are a new way to treat prostate cancer. They block the hormone testosterone, which helps cancer grow. This is different from older treatments.
LHRH antagonists stop the hormone LHRH from working. This reduces the hormone LH and then testosterone. It helps slow down cancer growth.
Key aspects of their mechanism include:
LHRH antagonists have some big advantages over LHRH agonists. These include:
These benefits make LHRH antagonists a good choice for treating prostate cancer. They are great when quick testosterone reduction is needed.
There are a few LHRH antagonists for prostate cancer treatment. These include:
These choices give doctors more options for treating prostate cancer. They can pick the best treatment based on each patient’s needs.
Anti-androgen medications are key in treating prostate cancer. They block androgens’ effects on cancer cells. This is vital in androgen deprivation therapy (ADT), which lowers male hormones like testosterone. These hormones can help prostate cancer grow.
First-generation anti-androgens were the first drugs to fight testosterone in prostate cancer. Examples include flutamide and bicalutamide. They block androgen receptors, stopping testosterone’s usual effects on cancer cells. These drugs are often used with LHRH agonists for better results.
Second-generation anti-androgens are newer and more effective. Apalutamide (Erleada), darolutamide (Nubeqa), and enzalutamide (Xtandi) are examples. They block androgen receptor signaling better, which is key in prostate cancer growth. These drugs have shown great benefits in clinical trials, mainly for advanced prostate cancer.
Anti-androgen medications are used in many prostate cancer cases. They are often started with LHRH agonists or antagonists. The choice between first and second-generation anti-androgens depends on cancer stage, patient health, and past treatments. Second-generation anti-androgens are often used for non-metastatic castration-resistant prostate cancer and metastatic hormone-sensitive prostate cancer.
Understanding anti-androgen generations and their uses helps doctors create better treatment plans. This can lead to better outcomes and quality of life for prostate cancer patients.
Prostate cancer injections given every six months have changed how we treat advanced prostate cancer. This new way of using androgen deprivation therapy (ADT) makes treatment easier for patients. It also means fewer injections, which is a big plus.
Long-acting LHRH agonists release medication slowly over months. This means patients only need injections every six months. It makes treatment more manageable and boosts patient compliance.
These long-acting formulas are given every 6 months. They offer a convenient option for those with prostate cancer.
Getting these injections is simple. They are given as a muscle injection. The schedule is every 6 months, based on the formula and patient needs.
| Formulation | Administration Schedule |
| LHRH Agonist | Every 6 months |
| LHRH Antagonist | Every 6 months |
Patients getting hormone injections for prostate cancer have varied experiences. Some might feel hot flashes or tiredness, while others might not notice much. The benefit of fewer injections can make treatment feel less burdensome.
In summary, long-acting prostate cancer injections are a great option. They help manage the disease effectively with less treatment hassle.
Adding pathway inhibitors to ADT is a big step forward in treating prostate cancer. It’s a big help for those with metastatic hormone-sensitive disease. This method has shown great promise in improving patient results by attacking the disease from different sides.
Androgen receptor pathway inhibitors (ARPIs) have changed how we treat prostate cancer. Drugs like abiraterone acetate and enzalutamide block the androgen receptor pathway. This is key for prostate cancer cells to grow and multiply.
ARPIs stop cancer cells from growing, which means better survival rates and quality of life for patients.
Using ADT with ARPIs is a strong strategy for treating metastatic hormone-sensitive prostate cancer. Studies show this combo is more effective than ADT alone.
This combo works by hitting cancer cells in different ways. It helps avoid resistance and boosts survival chances.
Studies show ARPIs with ADT greatly improve survival for patients with metastatic hormone-sensitive prostate cancer. For example, abiraterone acetate and enzalutamide with ADT can extend life and slow disease growth.
| Treatment | Survival Benefit | Disease Progression |
| ADT + Abiraterone Acetate | Improved Overall Survival | Delayed Disease Progression |
| ADT + Enzalutamide | Enhanced Survival Rates | Reduced Risk of Progression |
In summary, adding androgen receptor pathway inhibitors to ADT is a major leap in treating metastatic hormone-sensitive prostate cancer. This combo offers better survival chances and quality of life for patients.
Recent studies have shed light on the use of Androgen Deprivation Therapy (ADT) in prostate cancer treatment. Understanding ADT’s prevalence and distribution is key for healthcare providers. It helps them make informed decisions.
A significant number of patients with non-metastatic prostate cancer receive ADT. Studies show that 38% of these patients are treated with ADT. This highlights ADT’s importance in prostate cancer treatment.
The way ADT is given shows interesting trends. For non-metastatic prostate cancer, 37% of patients get LHRH agonists. Only 2% undergo surgical orchiectomy. This shows a preference for medical castration over surgery.
Looking at ADT prescription trends gives us insights into prostate cancer treatment. As new treatments come and guidelines change, ADT use will likely evolve. It’s important for healthcare providers to keep up with these changes.
| Treatment Method | Percentage of Patients |
| LHRH Agonists | 37% |
| Surgical Orchiectomy | 2% |
| Other ADT Methods | 1% |
By looking at ADT usage statistics, we can understand its role in prostate cancer management. We can also find areas for research and improvement.
Managing side effects of hormone therapy is key for men with prostate cancer. Androgen deprivation therapy (ADT) is a common treatment. It can cause various side effects.
Short-term side effects of ADT can be tough for patients. Common issues include:
These symptoms can be hard to deal with. But, there are ways to manage them. For example, hot flashes can be treated with gabapentin or estrogen patches.
Long-term use of ADT can cause serious health issues. These include:
It’s important to monitor bone density and manage metabolic changes for those on long-term ADT.
| Side Effect | Management Strategy |
| Hot Flashes | Gabapentin, estrogen patches |
| Osteoporosis | Bisphosphonates, calcium and vitamin D supplements |
| Diabetes | Dietary changes, metformin |
To lessen ADT side effects, healthcare providers suggest lifestyle changes and medications. Lifestyle changes include:
Medications like bisphosphonates can prevent osteoporosis. Drugs like metformin can help manage diabetes risk.
By understanding ADT side effects and using strategies to lessen them, we can greatly improve prostate cancer patients’ quality of life.
The 2025 PCS4 trial has given us new insights into testosterone recovery after long-term Androgen Deprivation Therapy (ADT). This study, a major breakthrough in prostate cancer treatment, shows how important testosterone recovery is for patient outcomes.
The PCS4 trial looked at patients who had long-term ADT and radiotherapy. Testosterone recovery to normal levels after this treatment greatly improved survival rates. This shows how vital testosterone recovery is in managing prostate cancer.
Our study of the trial data showed that patients who recovered their testosterone had better health outcomes. This highlights the need for doctors to watch and support testosterone recovery in patients on long-term ADT.
The PCS4 trial found a 46% reduction in mortality risk for patients who recovered their testosterone. This big drop in mortality risk shows the benefits of adding testosterone recovery to prostate cancer treatments.
The trial’s data is shown in the table below. It compares the mortality risk between patients who recovered their testosterone and those who didn’t.
| Patient Group | Mortality Risk |
| Patients with Testosterone Recovery | 54% (relative risk reduction) |
| Patients without Testosterone Recovery | 100% (baseline risk) |
The 2025 PCS4 trial’s findings are key for future prostate cancer treatment plans. Personalized treatment plans that include testosterone recovery could become the new standard. This could lead to better patient outcomes and quality of life.
As we look ahead, it’s important to use these findings in clinical practice. We must ensure patients get care that addresses their cancer treatment and overall well-being.
As we keep improving androgen deprivation methods, it’s clear they’re key in treating prostate cancer better. Understanding Androgen Deprivation Therapy (ADT) helps us make treatments more effective. This leads to better results for patients.
Hormone therapy has evolved, giving us new ways to fight prostate cancer. We now have LHRH agonists and antagonists, anti-androgen drugs, and combo therapies. These options make treatments more tailored and successful.
Our knowledge of ADT in treating prostate cancer is growing. Studies like the 2025 PCS4 trial show the benefits of testosterone recovery after long ADT. This could mean better survival rates for patients.
By using the latest research and expertise, we can keep improving androgen deprivation methods. This will make hormone therapy better for prostate cancer patients, improving their quality of life.
ADT is a treatment for prostate cancer. It lowers male hormones like testosterone. This slows down cancer cell growth.
ADT reduces androgens, which help prostate cancer grow. This slows down cancer and helps manage symptoms.
There are several ADT options. These include medical castration, surgical orchiectomy, and combined androgen blockade.
LHRH agonists lower testosterone production. They are given as injections every few months.
LHRH antagonists directly lower testosterone levels. They offer an alternative to LHRH agonists.
Anti-androgen medications block testosterone’s effect on cancer cells. They are key in ADT.
Long-acting formulations, like injections every 6 months, are convenient. They improve treatment adherence and reduce hospital visits.
Adding androgen receptor pathway inhibitors to ADT is a big step forward. It improves survival for patients with advanced cancer.
ADT can cause hot flashes and long-term issues like osteoporosis. Lifestyle changes and medications can help manage these side effects.
The PCS4 trial showed testosterone recovery after ADT lowers mortality risk. This could change future treatment plans and improve patient outcomes.
ADT is used for non-metastatic prostate cancer to manage high-risk disease. The choice of treatment depends on the clinical scenario.
Combined androgen blockade uses different ADT methods. It’s used in specific cases to improve treatment results.
National Center for Biotechnology Information. (2025). What Is Androgen Deprivation Therapy for Prostate Cancer.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!