Last Updated on October 31, 2025 by

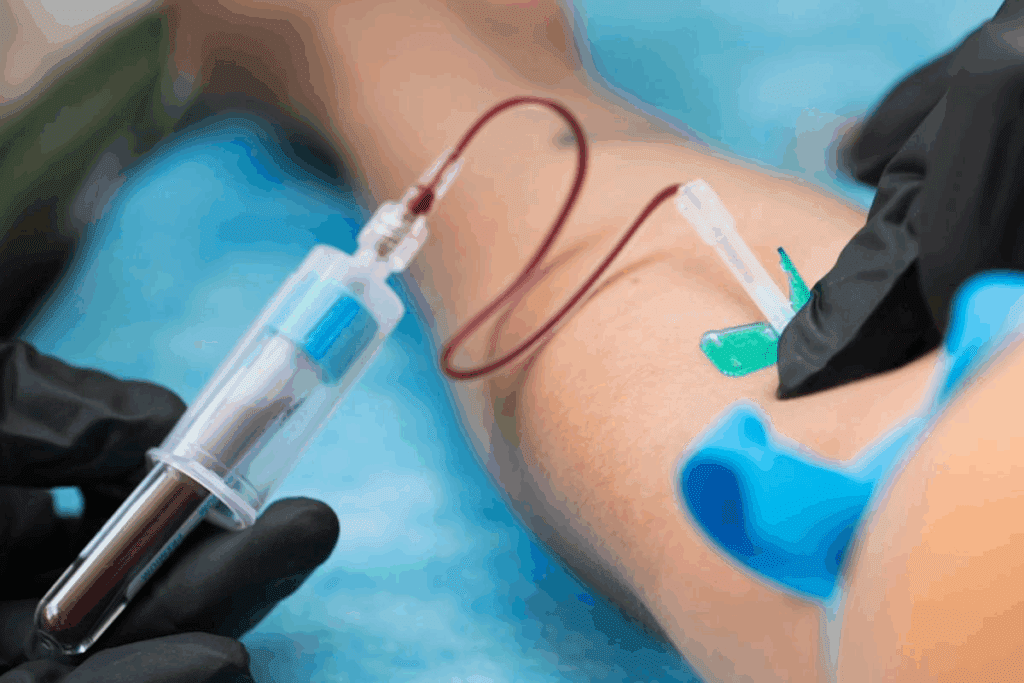
Diagnosing congestive heart failure needs a detailed approach. Blood tests are key in this process. At Liv Hospital, we use top-notch lab tech to spot the condition early.
Learn the top lab values for congestive heart failure and their importance in diagnosis.
Blood tests show important signs about the heart’s function. They help find underlying issues that might cause heart failure. A special protein made by the heart and blood vessels is very telling, as its levels go up in heart failure.
By getting the blood test results, we can give precise diagnoses and create good treatment plans. Our team is committed to top-notch healthcare. We offer full support for patients from abroad.
Congestive heart failure is a serious condition that affects millions worldwide. It’s important to understand how it’s diagnosed to manage it effectively. Heart failure happens when the heart can’t pump enough blood for the body’s needs. Conditions like coronary artery disease and high blood pressure can cause this.
Congestive heart failure, or heart failure, is a chronic condition. It happens when the heart can’t pump blood well. This leads to fatigue, swelling in the legs, and shortness of breath. The heart muscle becomes weakened or damaged, making it hard for the heart to pump blood.
Laboratory testing is key in diagnosing congestive heart failure. We use blood tests to check the heart’s function and find heart failure causes. Laboratory tests give us the data we need to confirm or rule out heart failure. They measure heart stress and damage markers like BNP or NT-proBNP.
Diagnosing congestive heart failure based on symptoms alone is tricky. Symptoms like shortness of breath and fatigue can mean other things too. Laboratory testing helps clarify the diagnosis by giving us specific heart condition information. By combining clinical evaluation with lab results, we get a more accurate diagnosis.

Blood tests are key in diagnosing and managing heart failure. They give vital info on the heart’s health. They also spot complications early.
Diagnosing congestive heart failure needs clinical checks, imaging, and lab tests. Blood tests are vital. They find biomarkers linked to heart failure. For example, B-type natriuretic peptide (BNP) and N-terminal pro b-type natriuretic peptide (NT-proBNP) are often high in heart failure patients.
These markers help diagnose and gauge heart failure’s severity. Doctors use them to decide on the right care and treatments.
After diagnosing heart failure, blood tests keep track of the disease’s progress. Regular tests show how the condition changes. This lets doctors adjust treatments as needed.
For example, checking basic metabolic panel electrolyte levels helps manage symptoms and prevent problems. Also, watching BNP or NT-proBNP levels over time shows if treatments are working. This info is key for patient care decisions.
Blood tests are vital for both diagnosis and treatment planning. They help find the best treatment strategies. For instance, a complete blood count (CBC) can spot anemia or other heart failure causes.
Also, blood tests check medication side effects. Some meds can harm the kidneys, which can be seen through BUN and creatinine tests. This lets doctors tweak treatments to avoid bad side effects.
BNP and NT-proBNP are key in diagnosing congestive heart failure. They are made by the heart when it’s under stress. This stress often comes from heart failure.
BNP is a hormone made by the heart’s ventricles when it’s strained. NT-proBNP is what BNP breaks down from. Both are signs of heart failure.
Knowing what BNP and NT-proBNP levels mean is key. Low levels mean heart failure is unlikely. High levels suggest it’s likely.
| Test | Normal/Indication | Abnormal/Indication |
| BNP | <100 pg/mL: Heart failure unlikely | >400 pg/mL: Heart failure likely |
| NT-proBNP | <300 pg/mL: Heart failure unlikely | >900 pg/mL (age < 50), >1800 pg/mL (age 50-75), >1800 pg/mL (age > 75): Heart failure likely |
BNP and NT-proBNP are very good at spotting heart failure. High levels mean heart failure is likely.
Even though BNP and NT-proBNP are helpful, they have limits. Age, kidney function, and weight can affect their levels. So, we must look at the whole picture of the patient.
By understanding these factors, we can make sure we’re diagnosing and treating heart failure correctly.
Healthcare providers use the Basic Metabolic Panel (BMP) to check on heart failure patients. It shows important health details like electrolyte levels and kidney function. This helps in managing heart failure better.
The BMP tests for glucose, sodium, potassium, calcium, chloride, carbon dioxide, BUN, and creatinine. Each test gives valuable info about the patient’s health. It helps spot issues that could affect heart failure care.
Electrolytes like sodium and potassium are key for heart health. Too little or too much can cause serious problems. For example, hypokalemia (low potassium) can lead to dangerous heart rhythms. On the other hand, hyperkalemia (high potassium) can cause fatal arrhythmias.
Sodium imbalances can also affect blood pressure and fluid balance. This makes heart failure harder to manage.
BUN and creatinine show how well the kidneys are working. High levels mean the kidneys might not be working right. This is common in heart failure patients.
Checking BUN and creatinine helps doctors adjust treatments. It helps manage fluid balance better.
The BMP’s findings are key for treating heart failure patients. It helps doctors tailor treatments to fix specific problems. This approach improves patient care and lowers the risk of complications.
Cardiac troponin tests are key in diagnosing heart problems. These proteins are vital for heart muscle function. When the heart is damaged, like in a heart attack, they leak into the blood. This makes them great markers for heart muscle injury.
Troponin tests check the blood for troponin levels. High levels mean heart muscle damage. The more troponin, the worse the damage, helping doctors decide on treatment.
Heart failure and heart attack are different. Heart failure is a long-term issue where the heart pumps poorly. A heart attack is when a blockage damages heart muscle. Troponin tests show if the heart is injured recently.
The main differences are:
High-sensitivity troponin tests can spot small amounts of troponin. This means they can catch heart problems earlier. This can lead to better care and outcomes for patients.
High troponin levels in heart failure patients mean a worse outlook. Watching troponin levels helps doctors know the risk. This helps them make better treatment plans.
The value of troponin levels includes:
Liver function tests are key in checking how heart failure affects the body. Heart failure can harm the liver by reducing blood flow and raising pressure. These tests are vital for caring for patients fully.
Heart failure can hurt the liver by affecting blood flow. When the heart doesn’t pump well, it can cause liver congestion. This can damage the liver and reduce its function. Monitoring liver health is important to see how heart failure affects the body.
There are important liver enzymes and markers to check in heart failure patients. These include:
These markers help understand the liver’s condition and how heart failure might be affecting it.
Abnormal liver function test results in heart failure need careful thought. High liver enzymes might show liver congestion or damage from heart failure. It’s important to look at the patient’s symptoms and other test results too.
Findings from liver function tests can change how we treat heart failure. For example, patients with serious liver problems might need different medications or treatments. Comprehensive care that looks at both heart and liver health is key for the best patient results.
A Complete Blood Count is a key tool for doctors to find hidden health issues that affect heart failure. It helps understand a patient’s health fully. This way, doctors can make better choices for their care.
A CBC checks many parts of the blood, like red and white blood cells, and platelets. The main parts of a CBC are:
These parts give a quick look at a patient’s blood health. They help find issues that might affect heart failure care.
Anemia is common in heart failure patients, affecting up to 50%. It means fewer red blood cells or hemoglobin. This makes it hard for tissues and organs to get enough oxygen.
Anemia makes heart failure symptoms worse, like feeling tired, short of breath, and less able to exercise. Studies show anemia can lead to more serious problems and death in heart failure patients. So, treating anemia is very important.
| Parameter | Normal Range | Anemic Range |
| Hemoglobin (g/dL) | 13.5-17.5 (male) | <13.5 (male) |
| 12-16 (female) | <12 (female) | |
| Hematocrit (%) | 40-54 (male) | <40 (male) |
| 37-48 (female) | <37 (female) |
Abnormalities in white blood cells can show infections or inflammation that affect heart failure. A high WBC count means the body might be fighting an infection, inflammation, or stress.
In heart failure, a high WBC count is linked to more hospital stays and deaths. So, it’s key to watch WBC counts to catch problems early.
CBC results can change how heart failure patients are treated. For example, finding anemia might mean starting iron supplements or special medicines to help oxygen reach tissues.
Also, odd WBC counts might lead to looking into infections or inflammation. This could mean using antibiotics or other treatments. By using CBC results, doctors can make treatment plans that are just right for each patient.
“The use of CBC in heart failure management allows for early detection of complications and comorbidities, enabling timely interventions that can improve patient outcomes.”
Understanding lab values is key to diagnosing and managing heart failure. Tests give vital info about a patient’s health. This helps doctors make the right decisions about treatment and care.
Doctors don’t just look at one test when diagnosing heart failure. They use many lab values to understand a patient’s health fully. For example, B-type natriuretic peptide (BNP) and NT-proBNP levels are checked with cardiac troponins to see how well the heart is working.
This way, doctors can see how severe heart failure is, find the cause, and plan the best treatment.
Watching lab values over time is key to managing heart failure. By tracking changes, doctors can see if treatment is working. They can then adjust the treatment if needed.
For example, if BNP levels go down, it means heart failure is being managed well. But if they go up, it might mean heart failure is getting worse.
Getting baseline lab values is very important. These values are used as a starting point for future comparisons. This helps doctors see if a patient’s condition is changing.
For patients with chronic conditions like heart failure, baseline values are even more important. They help doctors track how the disease is progressing and if treatments are working.
Abnormal lab results can be a worry, but they need to be looked at in context. Doctors consider the patient’s history, symptoms, and other test results when they see abnormal values.
For example, high cardiac troponin levels might mean heart damage. And abnormal electrolyte levels could point to complications. Addressing these issues quickly can help prevent more problems and improve patient care.
Heart failure patients often ask how often they should get blood tests. Blood tests are key in managing heart failure. They help doctors diagnose and monitor the condition, and adjust treatments.
When first diagnosed with heart failure, patients start with a blood test series. This includes a complete blood count (CBC), basic metabolic panel (BMP), and tests like BNP or NT-proBNP. These tests give a first look at the patient’s health and find any underlying issues.
After the first tests, regular blood tests are needed. How often depends on the heart failure’s severity, the patient’s health, and treatment response. Stable heart failure patients might need tests every 6 to 12 months. Those with severe or unstable heart failure might need more frequent tests.
When heart failure symptoms get worse, blood tests are needed more often. These tests help doctors quickly see changes and adjust treatments. Tests during these times include BNP or NT-proBNP to check heart failure severity and other tests for complications.
Some heart failure medications, like anticoagulants and diuretics, need regular blood tests. For example, warfarin patients need INR tests to keep their blood in the right range. Diuretics patients might need electrolyte level checks to avoid imbalances.
| Medication | Monitoring Test | Frequency |
| Warfarin | INR | Every 1-4 weeks |
| Diuretics | Electrolyte levels (e.g., potassium) | Every 3-6 months |
| Digoxin | Digoxin level | Every 6-12 months |
In conclusion, blood test frequency for heart failure patients depends on their condition, treatment, and health. Knowing when and how often to get blood tests helps patients manage their heart failure better and improve their life quality.
New biomarkers are being discovered to help diagnose and manage heart failure better. These biomarkers give us new insights into heart failure’s complex nature. They could lead to more tailored and effective treatments.
Galectin-3 and ST2 are biomarkers that have caught a lot of attention. Galectin-3 is linked to fibrosis and inflammation, key parts of heart failure. High levels of galectin-3 are tied to worse outcomes for heart failure patients. ST2 is part of the interleukin-1 receptor family and plays a role in heart remodeling. Both biomarkers help us understand how much the heart has changed, aiding in treatment planning.
MicroRNAs are small RNAs that control gene expression. Research has found specific microRNAs linked to heart failure. They could be used to diagnose and predict outcomes. Genetic markers are also being studied to identify risk and tailor treatments.
Inflammation is a big part of heart failure. C-reactive protein (CRP) is a known inflammation marker linked to poor outcomes in heart failure. Other markers are being looked into for diagnosing and managing heart failure.
The future of heart failure diagnosis and treatment involves these new biomarkers. As research finds more biomarkers, we’ll see more precise and personalized care. The idea of using multiple biomarkers together is very promising.
Comprehensive blood testing is key in managing heart failure. It gives important info for diagnosing and treating the condition. We talked about lab tests like BNP and NT-proBNP, cardiac troponins, and liver function tests.
These tests help doctors understand how severe heart failure is and track its progress. They can also guide treatment choices and adjust medications. Blood tests can spot other health issues, like anemia or kidney problems, that affect heart failure care.
Blood tests for CHF are very important. They let doctors check if treatments are working and make changes if needed. We suggest heart failure patients work with their doctors to create a testing plan. This ensures they get the best care for their condition.
In summary, blood testing is vital for managing heart failure. By using these tests, doctors can improve patient outcomes and quality of life.
We use several blood tests to diagnose congestive heart failure. These include B-type natriuretic peptide (BNP) and NT-proBNP. We also check basic metabolic panels, cardiac troponins, liver function tests, and complete blood counts.
BNP and NT-proBNP are biomarkers that help diagnose heart failure. They measure the levels of these peptides in the blood. These peptides are released by the heart when it’s under strain.
The frequency of blood tests for heart failure patients varies. Generally, we recommend regular monitoring. This is important during the initial diagnosis and when adjusting treatment plans.
Electrolyte imbalances, like sodium and potassium imbalances, can affect heart function. They may require changes to treatment plans.
Yes, blood tests like complete blood count can identify underlying conditions. For example, anemia can contribute to or worsen heart failure.
Cardiac troponins are biomarkers that detect myocardial injury. They help differentiate heart failure from heart attack and assess prognosis.
Liver function tests evaluate the systemic effects of heart failure on the liver. They provide insights into the severity of the condition and guide treatment decisions.
Yes, emerging biomarkers like galectin-3, ST2, microRNAs, and inflammatory markers are being researched. They may play a role in diagnosing and managing heart failure.
Interpreting lab values involves considering multiple test results together. We also trend values over time. Understanding the clinical significance of abnormal results is key.
Lab tests are vital in monitoring disease progression and guiding treatment decisions. They provide insights into the effectiveness of treatment and help identify complications.
National Center for Biotechnology Information. (2025). 5 Essential Blood Tests for Diagnosing Congestive Heart.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!