Last Updated on November 25, 2025 by Ugurkan Demir

We focus on treating heart rhythm problems at Liv Hospital. Knowing about sodium channel blockers is key. Class 1 antiarrhythmics help by making the heart less excited and slowing down its signals.
Understand class 1 antiarrhythmics and how they affect cardiac conduction.
These drugs block sodium channels in the heart. This helps control the heart’s rhythm. Our team at Liv Hospital uses the latest research to help our patients. We’re all about giving you the best care.
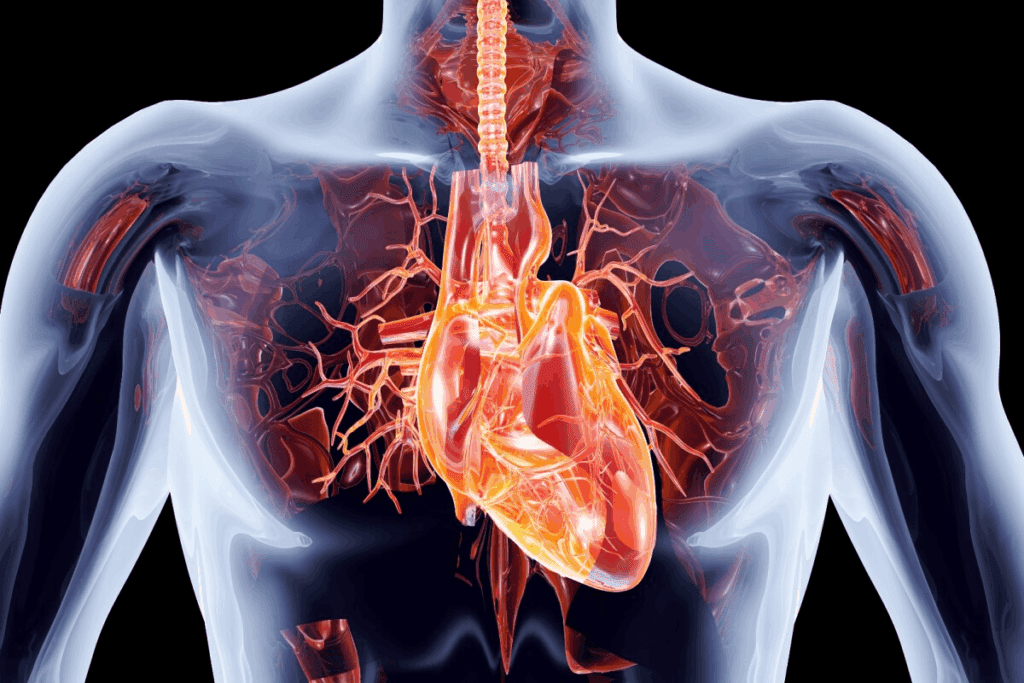
It’s key to know how the heart’s electrical system works to understand arrhythmias. This system is a complex network. It sends out electrical signals that control our heartbeat.
The heart’s natural pacemaker is the sinoatrial (SA) node. It starts the electrical impulse. This impulse then goes through the atrioventricular (AV) node and down the bundle of His.
It reaches the ventricular muscle, making it contract. This ensures the heart beats regularly and efficiently.
Arrhythmias happen when the heart’s electrical activity is disrupted. This can be due to problems in the SA node, AV node, or conduction pathways. They can be caused by genetics, electrolyte imbalances, or heart diseases.
Knowing how arrhythmias work is key to finding good treatments. This includes using class 1 antiarrhythmic drugs.
| Component | Function | Potential Arrhythmia Cause |
| Sinoatrial (SA) Node | Natural Pacemaker | Abnormal Automaticity |
| Atrioventricular (AV) Node | Regulates Impulse Conduction | Conduction Blocks |
| Bundle of His | Conducts Impulses to Ventricles | Bundle Branch Blocks |
| Ventricular Muscle | Contracts to Pump Blood | Ventricular Tachycardia/Fibrillation |
Understanding the heart’s electrical system helps us see why class 1 antiarrhythmic drugs are important. These drugs are chosen based on the type of arrhythmia and the heart condition.
Class 1 antiarrhythmics are key in treating heart rhythm problems. They work by stopping sodium from entering heart cells. This is vital for controlling different heart rhythm issues.
Class 1 antiarrhythmics block sodium channels in heart cells. This action slows how quickly the heart beats. It’s the main reason they help with heart rhythm problems.
These drugs block sodium channels, which are key for heart cell activity. By doing this, they make the heart’s electrical activity more stable. This helps prevent irregular heartbeats.
Class 1 antiarrhythmics have been used for over a century. They have evolved into subclasses like Class 1a, 1b, and 1c. Each has its own uses and effects.
| Subclass | Examples | Clinical Use |
| Class 1a | Quinidine, Procainamide | Treatment of ventricular arrhythmias, some supraventricular arrhythmias |
| Class 1b | Lidocaine, Mexiletine | Primarily used for ventricular arrhythmias, specially in acute settings |
Class 1 antiarrhythmics are important for treating many heart rhythm issues. They can greatly improve patient outcomes. But, their use must be carefully weighed against possible risks and side effects.
Class 1 antiarrhythmics work by changing how cardiac sodium channels function. These channels are key to the heart’s electrical activity. They let sodium ions rush in during the heart’s initial electrical phase.
Understanding how these channels work and how Class 1 antiarrhythmics affect them is key. This knowledge helps us see how they work.
Cardiac sodium channels are proteins in the heart cell membrane. They have an alpha subunit for sodium ion passage and beta subunits for function control. At rest, these channels are closed.
When the cell depolarizes, they open quickly. This lets sodium ions rush in, making the membrane positive. This is vital for starting the heart’s action.
These channels have closed, open, and inactivated states. Their state changes based on voltage. Class 1 antiarrhythmics bind to these channels, mainly when they’re open or inactivated. This reduces sodium influx.
During depolarization, Class 1 antiarrhythmics bind to sodium channels. This reduces how often channels open and the sodium current. This slows heart conduction, helping with arrhythmias.
As Medical Expert, “The success of antiarrhythmic drugs depends on ion channel modulation.” Class 1 antiarrhythmics show this principle well. They change sodium channel function, a key therapeutic strategy.
In summary, Class 1 antiarrhythmics work by affecting cardiac sodium channels. This changes the heart’s electrical activity. Their binding during depolarization is key to their antiarrhythmic effects, making them useful for many heart rhythm problems.
It’s important to know about the three subclasses of Class 1 antiarrhythmics – 1a, 1b, and 1c. They work differently and are used for various heart conditions. These subclasses are based on how the drugs affect the heart’s electrical activity.
The subclasses are based on how fast the drugs work and their effects on the heart. This helps doctors choose the right drug for each patient. It also helps predict side effects.
The way these drugs block sodium channels is key. This affects how well they work and how safe they are. The speed at which they bind and unbind to channels is different for each subclass.
The main differences are in how they block sodium channels and affect the heart’s electrical activity. Class 1a antiarrhythmics block sodium channels a bit and make the action duration longer. Class 1b antiarrhythmics block more but make the action duration shorter. Class 1c antiarrhythmics block a lot but don’t change the action duration much.
| Subclass | Sodium Channel Blockade | Effect on Action Duration | Examples |
| Class 1a | Moderate | Prolonged | Quinidine, Procainamide |
| Class 1b | High affinity for inactivated channels | Shortened | Lidocaine, Mexiletine |
| Class 1c | Potent | Minimal effect | Flecainide, Propafenone |
As shown in the table, each subclass has its own unique traits. Knowing these differences is key to picking the right drug for heart conditions.
Class 1a antiarrhythmics are key in treating heart rhythm problems. They work differently than other Class 1 drugs. This makes them special.
We’ll look at how they work and why they’re important. They change how sodium channels in heart cells work. This affects the heart’s electrical signals.
Class 1a antiarrhythmics are known for making the heart’s electrical signals last longer. They do this by slowing down how sodium channels close. This makes the heart less likely to have irregular beats.
This effect is important because it changes how the heart’s electrical signals work. It helps keep the heart rhythm steady.
Quinidine, procainamide, and disopyramide are the main drugs in Class 1a. Each has its own way of working and is used for different heart problems.
These drugs are effective but need careful use. They can have side effects and might not work for everyone.
Class 1b antiarrhythmics are special because they shorten the action duration of the heart’s electrical signal. This makes them useful in treating certain heart rhythm problems. We’ll see how this helps patients with specific heart issues.
These drugs work by binding to sodium channels, mainly when they’re in an inactive state. This action reduces the flow of sodium ions during the heart’s electrical signal. This effect is most pronounced in ischemic or damaged cardiac tissue, where abnormal electrical activity is more common.
The shortening of the action duration has important benefits. It reduces the unevenness of the heart’s electrical recovery, which can lead to dangerous heart rhythms. By reducing this unevenness, Class 1b drugs can help control ventricular arrhythmias without harming the heart’s upper chambers.
There are several Class 1b antiarrhythmics, each with its own characteristics. The main ones are lidocaine, mexiletine, and phenytoin.
These drugs give doctors options for treating ventricular arrhythmias. They’re useful when other treatments can’t be used or won’t work.
Class 1c antiarrhythmics, like flecainide and propafenone, slow down heart conduction a lot. They are key in treating heart rhythm problems by affecting how the heart conducts electrical signals.
We will look into how they slow down heart conduction and their uses in medicine.
Class 1c antiarrhythmics slow down heart conduction. They do this by affecting sodium channels in the heart. Sodium channels are important for starting and spreading electrical signals in the heart.
Sodium channel blockade is how these drugs work. They block sodium from entering the heart cells during depolarization. This slows down how fast the action potentials rise, which in turn slows down conduction.
Flecainide and propafenone are the main Class 1c antiarrhythmics used today. They are good at treating heart rhythm problems like atrial fibrillation and supraventricular tachycardia.
Flecainide is known for its strong effect in slowing down heart conduction. It’s a good choice for some arrhythmias, but it needs careful use because of possible side effects.
Propafenone also works well against arrhythmias and has some beta-blocking action. This extra effect can help it work better for some patients.
Both flecainide and propafenone are usually safe, but they should be used carefully. This is to avoid any bad side effects.
Class 1 antiarrhythmics can cause changes in the heart’s electrical signals. These changes include alterations in the QRS complex, QT interval, and PR interval. Knowing these changes helps doctors understand how these drugs work and their possible risks.
Class 1 antiarrhythmics often widen the QRS complex. This is more noticeable with Class 1C drugs like flecainide and propafenone. These drugs slow down the heart’s electrical signals.
It’s important to watch the QRS duration when starting or changing these medications. A big widening can mean serious heart problems are coming.
Class 1 antiarrhythmics can also change the QT interval. The effect varies by drug type. Class 1A drugs, like quinidine and procainamide, often make the QT interval longer.
QT interval prolongation can raise the risk of dangerous heart rhythms. So, it’s key to keep an eye on the QT interval, mainly with Class 1A drugs.
The PR interval can also change with Class 1 antiarrhythmics. These drugs can slow down the electrical signal through the AV node. This can help in some heart rhythm problems but can also cause issues.
Doctors need to watch for these changes when treating patients with these drugs. This helps avoid unwanted effects.
In summary, Class 1 antiarrhythmics cause important changes in heart signals. Doctors must understand these changes to use these drugs safely and effectively.
Class 1 antiarrhythmics are good at treating arrhythmias but can sometimes cause them. This makes them a big challenge in medicine. It’s important to think about this when using these drugs.
The reasons behind proarrhythmia from Class 1 antiarrhythmics are complex. These drugs change how the heart works, which can lead to arrhythmias. They slow down how signals move and make the heart take longer to recover, which can start re-entrant circuits.
Key factors contributing to proarrhythmia include:
Some patients are more at risk for proarrhythmic effects from Class 1 antiarrhythmics. Knowing these risk factors is key to safe use.
Risk factors include:
It’s important to watch patients closely on Class 1 antiarrhythmics. Regular ECG checks can spot signs of proarrhythmia, like wider QRS or longer QT intervals.
Good monitoring includes:
By knowing how proarrhythmia works, identifying risks, and using good monitoring, doctors can lower risks. This helps make these drugs more effective and safer for patients.
Class 1 antiarrhythmics are key in treating heart rhythm problems. They follow strict guidelines for use. These drugs have been vital in treating arrhythmias for many years.
These drugs help manage heart rhythm issues like atrial fibrillation and flutter. Flecainide and propafenone are effective in keeping the heart rhythm normal. But, they must be used carefully because of the risk of heart rhythm problems.
Doctors consider several things when using these drugs. This includes the type and length of the arrhythmia, the patient’s health, and how well the patient has responded to treatment before.
Class 1 antiarrhythmics also treat ventricular arrhythmias. Lidocaine is often used for ventricular tachycardia and fibrillation, mainly after a heart attack.
Choosing the right Class 1 antiarrhythmic depends on the heart disease, the type of arrhythmia, and the heart’s function.
Choosing the right patient for Class 1 antiarrhythmics is very important. These drugs are not for everyone, like those with:
Doctors must carefully check the patient’s health and heart rhythm to avoid bad side effects.
In summary, Class 1 antiarrhythmics are vital for treating heart rhythm problems. Their use must be based on a deep understanding of their effects and risks.
When we prescribe Class 1 antiarrhythmics, we must think about drug interactions and special needs. These things can change how well and safely the treatment works.
Class 1 antiarrhythmics can mix with other drugs in different ways. This can affect how the body absorbs, spreads, breaks down, and gets rid of the drugs. For example, some Class 1 antiarrhythmics are broken down by the cytochrome P450 system. This makes them react with other drugs that speed up or slow down this system.
Quinidine, a Class 1a antiarrhythmic, is a strong inhibitor of the cytochrome P450 system. When taken with other drugs that this system breaks down, like some antidepressants or antipsychotics, quinidine can make these drugs build up. This can lead to too much of the drug in the body, causing harm.
People with hepatic or renal impairment need special care with Class 1 antiarrhythmics. Many of these drugs are made in the liver or removed by the kidneys. If these organs don’t work well, the drug can build up, raising the risk of side effects.
Lidocaine, a Class 1b antiarrhythmic, is broken down by the liver. In people with serious liver problems, the lidocaine dose should be lowered to avoid too much of it. Drugs like procainamide and N-acetylprocainamide (its active form) are removed by the kidneys. So, in patients with kidney problems, the dose needs to be adjusted.
The elderly often have many health issues and take several drugs. This increases the chance of drug interactions with Class 1 antiarrhythmics. Also, as people age, their kidneys work less and their body changes, affecting how drugs work.
In pregnant women, using Class 1 antiarrhythmics must be carefully thought about. While some, like lidocaine, are generally safe, others might be risky. For example, quinidine can cause problems with the uterus and has been linked to harm to the fetus in some cases.
We must think carefully about these issues when treating arrhythmias in special groups. We need to balance the need for effective treatment with the possible risks.
We’ve looked into how Class 1 antiarrhythmics work and their types. These medicines are key in treating heart rhythm problems. Their role is changing as cardiology advances.
Today, Class 1 antiarrhythmics are being used in new ways thanks to research. Our understanding of heart rhythms is growing. This means doctors can treat patients better, using less medicine and fewer side effects.
As Class 1 antiarrhythmics evolve, doctors must keep up with the latest in heart medicine. This helps us improve care and move cardiology forward.
Class 1 antiarrhythmics are medicines that help control irregular heartbeats. They do this by blocking sodium channels in the heart. This helps keep the heart rhythm normal.
Class 1 antiarrhythmics are divided into three subclasses: Class 1a, Class 1b, and Class 1c. Each has its own effects on the heart.
Class 1 antiarrhythmics bind to sodium channels in heart cells during depolarization. This blocks sodium ions from entering the cells.
Class 1a antiarrhythmics lengthen the action period. Class 1b shorten it. Class 1c slow down heart conduction.
Quinidine, procainamide, and disopyramide are examples of Class 1a antiarrhythmics.
Lidocaine, mexiletine, and phenytoin are examples of Class 1b antiarrhythmics.
Flecainide and propafenone are examples of Class 1c antiarrhythmics.
Class 1 antiarrhythmics can alter the QRS complex, QT interval, and PR interval on an ECG.
The proarrhythmic paradox is when Class 1 antiarrhythmics can cause arrhythmias in some patients. This is despite their purpose to treat arrhythmias.
Class 1 antiarrhythmics are used to manage various arrhythmias. They are chosen carefully, considering patient needs and safety.
Class 1 antiarrhythmics can interact with other drugs. Their use must be carefully considered in patients with liver or kidney issues, the elderly, or pregnant women.
Patients on Class 1 antiarrhythmics are watched for side effects, including arrhythmia. They are also checked regularly for changes in their ECG and overall health.
National Center for Biotechnology Information. (2025). 7 Key Facts About Class 1 Antiarrhythmics Mechanisms. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482322/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!