Last Updated on November 27, 2025 by Ugurkan Demir

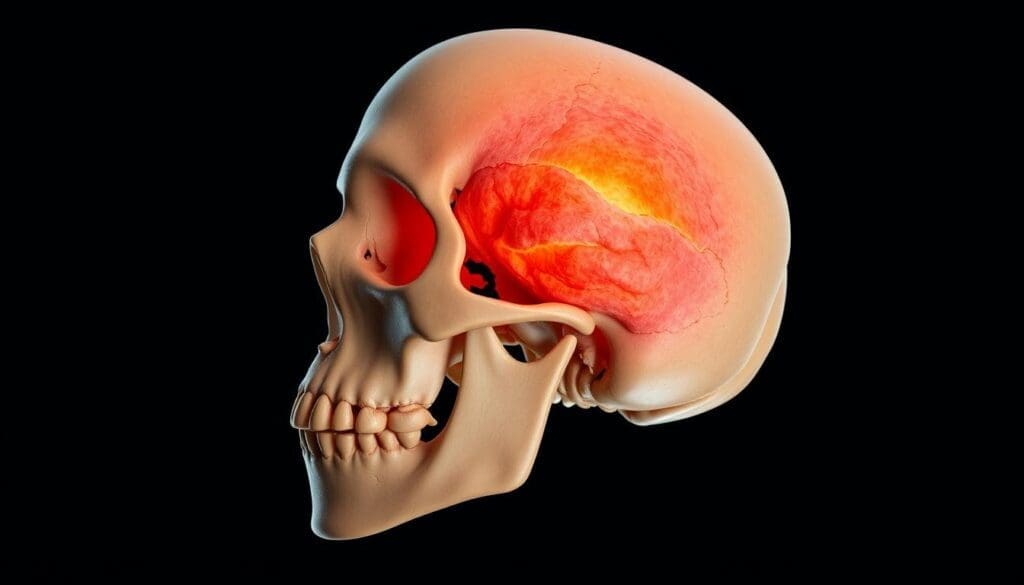
Osteosarcoma of the skull is a rare and aggressive bone cancer. It starts in the bones of the skull. This type of cancer is a small part of all osteosarcoma cases.
Osteosarcoma mainly hits the limbs and mostly affects people under 25. When it’s in the skull, it’s harder to treat because of its close location to important parts of the body.
At Liv Hospital, we offer top-notch care for complex cases like osteosarcoma of the skull. Our team works hard to give patients and their families the support they need.
Osteosarcoma is a complex bone cancer that can happen in any bone, including the skull. It’s a rare and aggressive disease. When it affects the skull, it poses unique challenges due to the skull’s complex anatomy and vital structures.
Osteosarcoma is a malignant bone tumor that makes bone matrix. It’s classified by its location, how it looks under a microscope, and its aggressiveness. The most common type is high-grade conventional intramedullary osteosarcoma.
Other types include chondroblastic osteosarcoma and telangiectatic osteosarcoma. Each has its own features.
Knowing how to classify osteosarcoma helps us predict its outcome and plan treatment. We use the World Health Organization (WHO) classification to guide us.
Osteosarcoma is rare, making up about 3-5% of childhood cancers and less than 1% of adult cancers. It’s even rarer in the skull. The exact number of skull osteosarcoma cases is hard to find because it’s so rare and hard to diagnose.
| Age Group | Incidence Rate |
| 0-19 years | 4.3 per million |
| 20-59 years | 2.1 per million |
| 60+ years | 1.8 per million |
Osteosarcoma is different from other bone cancers because it makes bone matrix and grows aggressively. It affects bone tissue, unlike chondrosarcoma, which affects cartilage. We diagnose it by looking at tissue samples under a microscope.
Knowing these differences is key for accurate diagnosis and treatment. We use imaging, biopsies, and clinical exams to tell osteosarcoma apart from other bone cancers.
The human skull is made of several bones that fuse together. Osteosarcoma, a bone cancer, can affect it. Knowing the skull’s anatomy is key to treating this condition well.
The skull is a complex structure that houses the head’s skeleton. It’s made of many bones that join during growth.
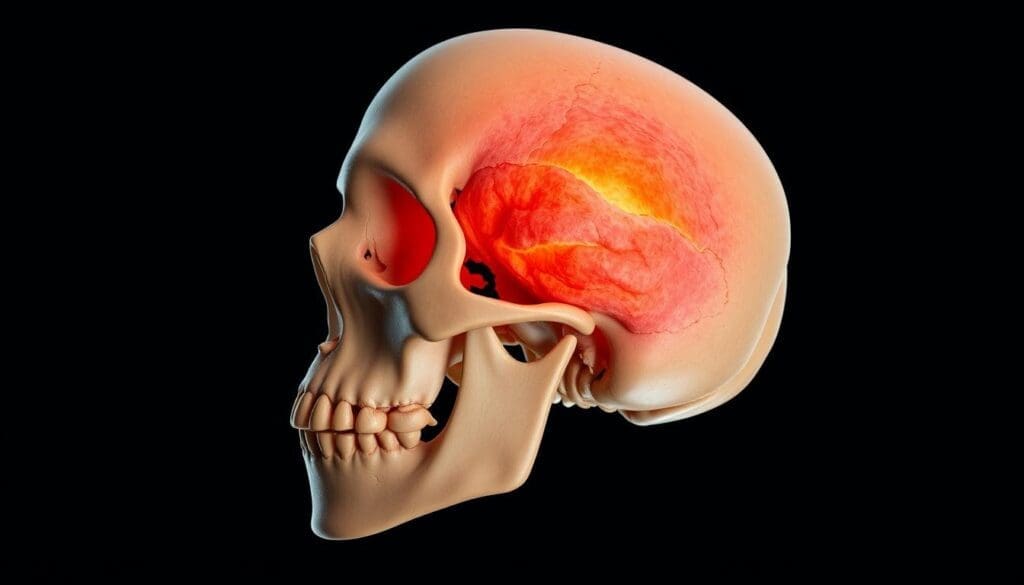
Osteosarcoma can happen in any skull part, including cranial bones. These bones form the brain’s home, the cranial cavity. Osteosarcoma here can cause a lot of harm because of its closeness to important brain parts.
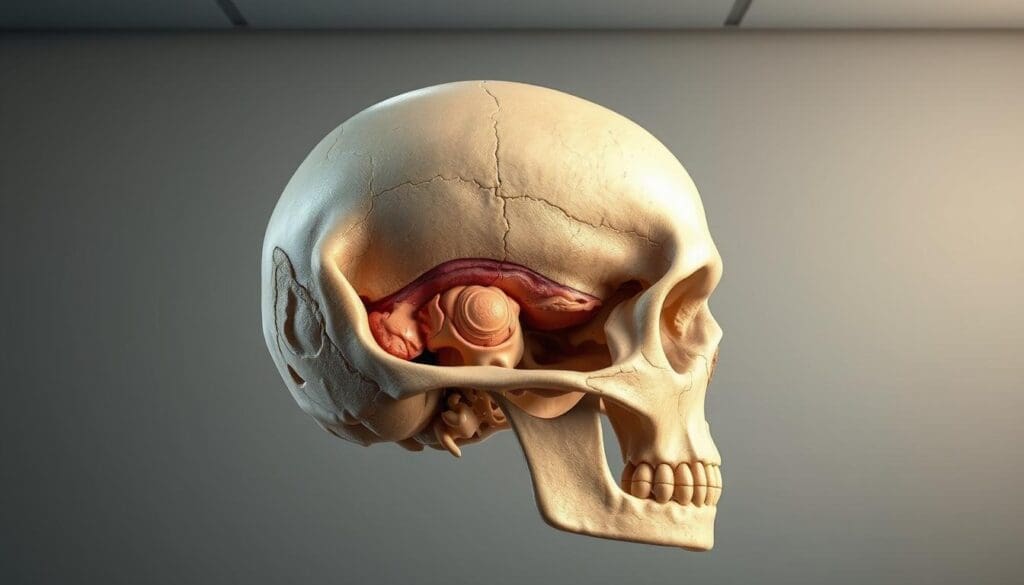
The skull base is another common spot for osteosarcoma. It’s the floor of the cranial cavity, separating the brain from facial structures. Tumors here are hard to treat because they’re near vital blood vessels and nerves.
The skull’s location affects how we treat osteosarcoma. For example, jaw tumors usually have a better outlook than skull base ones. Survival rates differ a lot by location. Jaw tumors have a 5-year survival rate of 75%, while skull base tumors are around 30.5%. Knowing these differences helps us plan better treatments.
Osteosarcoma of the skull is a complex condition with various subtypes. Each subtype has its own characteristics and affects treatment planning. Knowing the subtypes is key to understanding the condition.
Conventional osteosarcoma is the most common type in the skull. It is known for producing osteoid matrix by cancer cells. This type can be further divided based on its appearance under a microscope.
Key Features:
Chondroblastic osteosarcoma mainly produces cartilage. It has a better prognosis than other types, if treated well.
Prognostic Implications: Patients with this type tend to do better, making accurate diagnosis very important.
Paget-associated osteosarcoma occurs in people with Paget’s disease. This type is aggressive and has a poor prognosis.
Clinical Considerations:
The 2020 World Health Organization Classification of Tumors of Bone lists several osteosarcoma subtypes. These include conventional, telangiectatic, and high-grade surface osteosarcoma. Understanding these subtypes is vital for choosing the right treatment and predicting outcomes.
Osteosarcoma in the skull comes from genetics, environment, and medical history. Knowing these factors helps find and treat this aggressive bone cancer early.
Genetics are key in skull osteosarcoma. Li-Fraumeni syndrome and hereditary retinoblastoma raise the risk. People with a family history of bone cancer are also at higher risk.
Some environmental factors can raise the risk of skull osteosarcoma. Radiation and chemicals may play a role, though the exact ways are not fully known.
Getting radiation therapy, even as a child, increases the risk of osteosarcoma. The risk grows with the dose and age at exposure.
Bone disorders like Paget’s disease can raise the risk of osteosarcoma. Catching and managing these conditions early is key to preventing osteosarcoma.
Early detection and treatment with surgery, chemotherapy, and radiotherapy can greatly improve survival rates for skull osteosarcoma patients. Understanding risk factors helps doctors prevent and treat this cancer more effectively.
Knowing the early signs of skull osteosarcoma can save lives. Early detection is key to better outcomes. The symptoms depend on the tumor’s location and size.
The first signs of osteosarcoma in the skull include pain or swelling. These signs can be hard to notice at first. But, if you have ongoing pain or swelling, see a doctor.
As osteosarcoma gets worse, symptoms get more severe. You might see:
The tumor can also press on nerves. This can cause double vision, hearing loss, or trouble swallowing.
The location of the tumor affects symptoms. For example:
| Location | Possible Symptoms |
| Skull Base | Headaches, cranial nerve deficits |
| Cranial Vault | Swelling, pain, visible deformity |
| Facial Bones | Facial asymmetry, pain, trouble chewing |
Early detection and diagnosis are vital for managing skull osteosarcoma. If you have ongoing or severe symptoms, get medical help right away.
Knowing how to diagnose skull osteosarcoma is key for good treatment. Accurate diagnosis helps find the best treatment and improves patient care.
Imaging studies are vital for diagnosing skull osteosarcoma. They show how big and where the tumor is. Common tools include:
Biopsy is a key tool for diagnosing skull osteosarcoma. It takes a tissue sample from the tumor for lab tests. There are two main types:
Doctors choose the best method based on the tumor’s location and the patient’s health.
Staging is critical for understanding the disease’s extent and planning treatment. It looks at the tumor’s size, location, and if it has spread. Accurate staging is important for:
Understanding these steps helps doctors create a treatment plan that fits the patient’s needs.
Skull cancer, like osteosarcoma, needs a special treatment plan. This plan includes surgery, chemotherapy, and sometimes radiation. The right treatment depends on the tumor’s stage, location, and type.
Surgery is key for osteosarcoma of the skull. The goal is to take out the tumor and some healthy tissue around it. Surgical methods change based on the tumor’s location and size.
For tumors in easy-to-reach parts of the skull, open surgery works well. But for tricky or sensitive areas, doctors use advanced techniques. These include navigation systems and imaging during surgery.
Chemotherapy is vital for osteosarcoma, helping to kill cancer cells that might have spread. Chemotherapy for skull osteosarcoma often uses a mix of drugs. These include doxorubicin, cisplatin, and methotrexate, given before and after surgery.
In some cases, radiation therapy is used. This is when the tumor can’t be fully removed or there’s a high chance of it coming back. Advanced radiation methods, like proton therapy, are used. They aim to hit the tumor hard while sparing nearby important areas.
New treatments for osteosarcoma of the skull are being explored. Clinical trials are looking at targeted therapies, immunotherapies, and more. These new methods could lead to better treatments for patients. Joining clinical trials might give patients access to new treatments.
Using different treatments together can greatly improve survival and quality of life for patients. It’s important for patients to talk with their healthcare team. Together, they can find the best treatment plan for each person.
Life expectancy and survival rates for osteosarcoma of the skull depend on many factors. Knowing these factors helps patients make better treatment choices.
The survival rate for osteosarcoma of the skull changes based on several things. These include the stage at diagnosis, where the tumor is, and its type. Localized osteosarcoma has a better chance of survival than metastatic disease.
“The 5-year survival rate for patients with localized osteosarcoma is significantly higher than those with metastatic disease,” as noted in recent medical literature. This shows how important early detection and treatment are.
Survival rates for osteosarcoma of the skull vary by location. Tumors in the jaw have a better chance of survival than those at the skull base. Jaw tumors have a 5-year survival rate of about 75%, while skull base tumors have rates around 30.5%. This shows how location affects treatment outcomes.
The type of osteosarcoma also affects survival rates. Chondroblastic osteosarcoma, for example, has a better prognosis than other types. Knowing the specific type of osteosarcoma is key for choosing the right treatment and predicting outcomes.
Several factors influence the prognosis of osteosarcoma of the skull. These include the stage at diagnosis, the patient’s age, overall health, and the treatment’s success. Early detection and a detailed treatment plan are key to improving survival rates.
As medical professionals, we stress that each patient’s situation is unique. Prognosis can vary a lot. So, it’s vital for patients to work closely with their healthcare team. This way, they can understand their specific prognosis and get a treatment plan that fits them.
The path to getting better after osteosarcoma treatment includes physical, cognitive, and cosmetic rehab. At our place, we know that comprehensive rehabilitation is key. It helps patients get their strength, function, and quality of life back.
Physical rehab is a big part of getting better. It aims to bring back mobility, strength, and function. Our team creates personalized exercise programs for each patient’s needs and goals.
Cognitive rehab is vital for those who lost brain function due to their illness or treatment. We offer cognitive therapy to help patients improve memory, attention, and processing skills.
After surgery, some patients need cosmetic and functional reconstruction. Our experts help plan reconstruction plans that look good and work well.
How long it takes to recover varies a lot. It depends on how much treatment was needed and the patient’s health. We give patients a clear recovery roadmap with milestones and expectations.
We also stress the need for support and care during rehab. We make sure our patients get all the help they need for their physical, emotional, and social well-being.
Getting a diagnosis of skull osteosarcoma starts a tough journey. It requires strength, support, and knowing what to do. Understanding all parts of living with this condition is key.
Dealing with skull osteosarcoma means finding ways to handle its emotional, physical, and mental sides. Good coping methods can really help improve life quality.
Every person’s fight is different. What helps one might not help another. So, it’s important to try out different ways to find what works best.
Having access to good support is key for those with skull osteosarcoma. These resources offer emotional help, practical aid, and important info.
| Resource Type | Description | Benefits |
| Support Groups | Groups of patients, families, and caregivers sharing experiences | Emotional support, community building |
| Counseling Services | Professional counseling for patients and families | Coping strategies, emotional support |
| Online Resources | Websites, forums, and online communities providing information and support | Accessibility, information sharing |
Regular check-ups are vital for watching how skull osteosarcoma progresses. They help catch any signs of it coming back early. A team of healthcare experts usually does this.
Follow-up care plans are made just for each patient. They might include:
It’s important to handle the long-term effects of treatment for skull osteosarcoma. These effects can be different for everyone.
We help patients find ways to deal with these effects. This might include:
Understanding osteosarcoma of the skull is key to better patient care. New treatments have boosted survival rates for this cancer. Early detection and full treatment are vital for a good outcome.
Knowing the signs of skull osteosarcoma helps patients get help fast. Treatment plans that include surgery, chemo, and radiation have shown promise. New treatments and trials offer hope for the future.
A team effort is essential in fighting skull osteosarcoma. Experts from oncology, surgery, and rehab work together. This approach improves life quality for patients. We’re dedicated to top-notch care and support for patients worldwide.
Osteosarcoma of the skull is a rare and aggressive bone cancer. It starts in the skull bones. It’s a type of osteosarcoma, the most common bone tumor.
Several factors can increase your risk. These include genetic predispositions, environmental factors, and bone disorders. Also, radiation exposure is a big risk factor.
Symptoms depend on the tumor’s location and size. Early signs might be pain or swelling. Advanced symptoms can include severe pain, neurological issues, or visible changes.
Diagnosing involves imaging studies and biopsies. Imaging shows the tumor’s size and location. Biopsy confirms the diagnosis.
Treatment combines surgery, chemotherapy, and radiation. The choice depends on the tumor’s stage, location, and type.
Survival rates vary. Tumors in the jaw have a better outlook than those at the skull base. The tumor’s type also affects survival.
Rehabilitation is key. It helps patients regain physical and mental function. They may also need cosmetic and functional reconstruction.
Coping with osteosarcoma requires effective strategies and support. Regular follow-ups are important to catch any recurrence early.
The tumor’s location affects treatment and prognosis. Jaw tumors have a better outlook than those at the skull base.
Yes, there are various subtypes. These include conventional, chondroblastic, and Paget-associated osteosarcoma, based on histological characteristics.
New treatments and clinical trials are emerging. They offer hope for better outcomes. These include new chemotherapy, radiation, and surgical options.
Osteosarcoma of the skull is a rare and aggressive bone cancer. It starts in the bones of the skull. This type of cancer is a small part of all osteosarcoma cases.
Osteosarcoma mainly hits the limbs and mostly affects people under 25. When it’s in the skull, it’s harder to treat because of its close location to important parts of the body.
At Liv Hospital, we offer top-notch care for complex cases like osteosarcoma of the skull. Our team works hard to give patients and their families the support they need.
Osteosarcoma is a complex bone cancer that can happen in any bone, including the skull. It’s a rare and aggressive disease. When it affects the skull, it poses unique challenges due to the skull’s complex anatomy and vital structures.
Osteosarcoma is a malignant bone tumor that makes bone matrix. It’s classified by its location, how it looks under a microscope, and its aggressiveness. The most common type is high-grade conventional intramedullary osteosarcoma.
Other types include chondroblastic osteosarcoma and telangiectatic osteosarcoma. Each has its own features.
Knowing how to classify osteosarcoma helps us predict its outcome and plan treatment. We use the World Health Organization (WHO) classification to guide us.
Osteosarcoma is rare, making up about 3-5% of childhood cancers and less than 1% of adult cancers. It’s even rarer in the skull. The exact number of skull osteosarcoma cases is hard to find because it’s so rare and hard to diagnose.
| Age Group | Incidence Rate |
| 0-19 years | 4.3 per million |
| 20-59 years | 2.1 per million |
| 60+ years | 1.8 per million |
Osteosarcoma is different from other bone cancers because it makes bone matrix and grows aggressively. It affects bone tissue, unlike chondrosarcoma, which affects cartilage. We diagnose it by looking at tissue samples under a microscope.
Knowing these differences is key for accurate diagnosis and treatment. We use imaging, biopsies, and clinical exams to tell osteosarcoma apart from other bone cancers.
The human skull is made of several bones that fuse together. Osteosarcoma, a bone cancer, can affect it. Knowing the skull’s anatomy is key to treating this condition well.
The skull is a complex structure that houses the head’s skeleton. It’s made of many bones that join during growth.
Osteosarcoma can happen in any skull part, including cranial bones. These bones form the brain’s home, the cranial cavity. Osteosarcoma here can cause a lot of harm because of its closeness to important brain parts.
The skull base is another common spot for osteosarcoma. It’s the floor of the cranial cavity, separating the brain from facial structures. Tumors here are hard to treat because they’re near vital blood vessels and nerves.
The skull’s location affects how we treat osteosarcoma. For example, jaw tumors usually have a better outlook than skull base ones. Survival rates differ a lot by location. Jaw tumors have a 5-year survival rate of 75%, while skull base tumors are around 30.5%. Knowing these differences helps us plan better treatments.
Osteosarcoma of the skull is a complex condition with various subtypes. Each subtype has its own characteristics and affects treatment planning. Knowing the subtypes is key to understanding the condition.
Conventional osteosarcoma is the most common type in the skull. It is known for producing osteoid matrix by cancer cells. This type can be further divided based on its appearance under a microscope.
Key Features:
Chondroblastic osteosarcoma mainly produces cartilage. It has a better prognosis than other types, if treated well.
Prognostic Implications: Patients with this type tend to do better, making accurate diagnosis very important.
Paget-associated osteosarcoma occurs in people with Paget’s disease. This type is aggressive and has a poor prognosis.
Clinical Considerations:
The 2020 World Health Organization Classification of Tumors of Bone lists several osteosarcoma subtypes. These include conventional, telangiectatic, and high-grade surface osteosarcoma. Understanding these subtypes is vital for choosing the right treatment and predicting outcomes.
Osteosarcoma in the skull comes from genetics, environment, and medical history. Knowing these factors helps find and treat this aggressive bone cancer early.
Genetics are key in skull osteosarcoma. Li-Fraumeni syndrome and hereditary retinoblastoma raise the risk. People with a family history of bone cancer are also at higher risk.
Some environmental factors can raise the risk of skull osteosarcoma. Radiation and chemicals may play a role, though the exact ways are not fully known.
Getting radiation therapy, even as a child, increases the risk of osteosarcoma. The risk grows with the dose and age at exposure.
Bone disorders like Paget’s disease can raise the risk of osteosarcoma. Catching and managing these conditions early is key to preventing osteosarcoma.
Early detection and treatment with surgery, chemotherapy, and radiotherapy can greatly improve survival rates for skull osteosarcoma patients. Understanding risk factors helps doctors prevent and treat this cancer more effectively.
Knowing the early signs of skull osteosarcoma can save lives. Early detection is key to better outcomes. The symptoms depend on the tumor’s location and size.
The first signs of osteosarcoma in the skull include pain or swelling. These signs can be hard to notice at first. But, if you have ongoing pain or swelling, see a doctor.
As osteosarcoma gets worse, symptoms get more severe. You might see:
The tumor can also press on nerves. This can cause double vision, hearing loss, or trouble swallowing.
The location of the tumor affects symptoms. For example:
| Location | Possible Symptoms |
| Skull Base | Headaches, cranial nerve deficits |
| Cranial Vault | Swelling, pain, visible deformity |
| Facial Bones | Facial asymmetry, pain, trouble chewing |
Early detection and diagnosis are vital for managing skull osteosarcoma. If you have ongoing or severe symptoms, get medical help right away.
Knowing how to diagnose skull osteosarcoma is key for good treatment. Accurate diagnosis helps find the best treatment and improves patient care.
Imaging studies are vital for diagnosing skull osteosarcoma. They show how big and where the tumor is. Common tools include:
Biopsy is a key tool for diagnosing skull osteosarcoma. It takes a tissue sample from the tumor for lab tests. There are two main types:
Doctors choose the best method based on the tumor’s location and the patient’s health.
Staging is critical for understanding the disease’s extent and planning treatment. It looks at the tumor’s size, location, and if it has spread. Accurate staging is important for:
Understanding these steps helps doctors create a treatment plan that fits the patient’s needs.
Skull cancer, like osteosarcoma, needs a special treatment plan. This plan includes surgery, chemotherapy, and sometimes radiation. The right treatment depends on the tumor’s stage, location, and type.
Surgery is key for osteosarcoma of the skull. The goal is to take out the tumor and some healthy tissue around it. Surgical methods change based on the tumor’s location and size.
For tumors in easy-to-reach parts of the skull, open surgery works well. But for tricky or sensitive areas, doctors use advanced techniques. These include navigation systems and imaging during surgery.
Chemotherapy is vital for osteosarcoma, helping to kill cancer cells that might have spread. Chemotherapy for skull osteosarcoma often uses a mix of drugs. These include doxorubicin, cisplatin, and methotrexate, given before and after surgery.
In some cases, radiation therapy is used. This is when the tumor can’t be fully removed or there’s a high chance of it coming back. Advanced radiation methods, like proton therapy, are used. They aim to hit the tumor hard while sparing nearby important areas.
New treatments for osteosarcoma of the skull are being explored. Clinical trials are looking at targeted therapies, immunotherapies, and more. These new methods could lead to better treatments for patients. Joining clinical trials might give patients access to new treatments.
Using different treatments together can greatly improve survival and quality of life for patients. It’s important for patients to talk with their healthcare team. Together, they can find the best treatment plan for each person.
Life expectancy and survival rates for osteosarcoma of the skull depend on many factors. Knowing these factors helps patients make better treatment choices.
The survival rate for osteosarcoma of the skull changes based on several things. These include the stage at diagnosis, where the tumor is, and its type. Localized osteosarcoma has a better chance of survival than metastatic disease.
“The 5-year survival rate for patients with localized osteosarcoma is significantly higher than those with metastatic disease,” as noted in recent medical literature. This shows how important early detection and treatment are.
Survival rates for osteosarcoma of the skull vary by location. Tumors in the jaw have a better chance of survival than those at the skull base. Jaw tumors have a 5-year survival rate of about 75%, while skull base tumors have rates around 30.5%. This shows how location affects treatment outcomes.
The type of osteosarcoma also affects survival rates. Chondroblastic osteosarcoma, for example, has a better prognosis than other types. Knowing the specific type of osteosarcoma is key for choosing the right treatment and predicting outcomes.
Several factors influence the prognosis of osteosarcoma of the skull. These include the stage at diagnosis, the patient’s age, overall health, and the treatment’s success. Early detection and a detailed treatment plan are key to improving survival rates.
As medical professionals, we stress that each patient’s situation is unique. Prognosis can vary a lot. So, it’s vital for patients to work closely with their healthcare team. This way, they can understand their specific prognosis and get a treatment plan that fits them.
The path to getting better after osteosarcoma treatment includes physical, cognitive, and cosmetic rehab. At our place, we know that comprehensive rehabilitation is key. It helps patients get their strength, function, and quality of life back.
Physical rehab is a big part of getting better. It aims to bring back mobility, strength, and function. Our team creates personalized exercise programs for each patient’s needs and goals.
Cognitive rehab is vital for those who lost brain function due to their illness or treatment. We offer cognitive therapy to help patients improve memory, attention, and processing skills.
After surgery, some patients need cosmetic and functional reconstruction. Our experts help plan reconstruction plans that look good and work well.
How long it takes to recover varies a lot. It depends on how much treatment was needed and the patient’s health. We give patients a clear recovery roadmap with milestones and expectations.
We also stress the need for support and care during rehab. We make sure our patients get all the help they need for their physical, emotional, and social well-being.
Getting a diagnosis of skull osteosarcoma starts a tough journey. It requires strength, support, and knowing what to do. Understanding all parts of living with this condition is key.
Dealing with skull osteosarcoma means finding ways to handle its emotional, physical, and mental sides. Good coping methods can really help improve life quality.
Every person’s fight is different. What helps one might not help another. So, it’s important to try out different ways to find what works best.
Having access to good support is key for those with skull osteosarcoma. These resources offer emotional help, practical aid, and important info.
| Resource Type | Description | Benefits |
| Support Groups | Groups of patients, families, and caregivers sharing experiences | Emotional support, community building |
| Counseling Services | Professional counseling for patients and families | Coping strategies, emotional support |
| Online Resources | Websites, forums, and online communities providing information and support | Accessibility, information sharing |
Regular check-ups are vital for watching how skull osteosarcoma progresses. They help catch any signs of it coming back early. A team of healthcare experts usually does this.
Follow-up care plans are made just for each patient. They might include:
It’s important to handle the long-term effects of treatment for skull osteosarcoma. These effects can be different for everyone.
We help patients find ways to deal with these effects. This might include:
Understanding osteosarcoma of the skull is key to better patient care. New treatments have boosted survival rates for this cancer. Early detection and full treatment are vital for a good outcome.
Knowing the signs of skull osteosarcoma helps patients get help fast. Treatment plans that include surgery, chemo, and radiation have shown promise. New treatments and trials offer hope for the future.
A team effort is essential in fighting skull osteosarcoma. Experts from oncology, surgery, and rehab work together. This approach improves life quality for patients. We’re dedicated to top-notch care and support for patients worldwide.
Osteosarcoma of the skull is a rare and aggressive bone cancer. It starts in the skull bones. It’s a type of osteosarcoma, the most common bone tumor.
Several factors can increase your risk. These include genetic predispositions, environmental factors, and bone disorders. Also, radiation exposure is a big risk factor.
Symptoms depend on the tumor’s location and size. Early signs might be pain or swelling. Advanced symptoms can include severe pain, neurological issues, or visible changes.
Diagnosing involves imaging studies and biopsies. Imaging shows the tumor’s size and location. Biopsy confirms the diagnosis.
Treatment combines surgery, chemotherapy, and radiation. The choice depends on the tumor’s stage, location, and type.
Survival rates vary. Tumors in the jaw have a better outlook than those at the skull base. The tumor’s type also affects survival.
Rehabilitation is key. It helps patients regain physical and mental function. They may also need cosmetic and functional reconstruction.
Coping with osteosarcoma requires effective strategies and support. Regular follow-ups are important to catch any recurrence early.
The tumor’s location affects treatment and prognosis. Jaw tumors have a better outlook than those at the skull base.
Yes, there are various subtypes. These include conventional, chondroblastic, and Paget-associated osteosarcoma, based on histological characteristics.
New treatments and clinical trials are emerging. They offer hope for better outcomes. These include new chemotherapy, radiation, and surgical options.
National Center for Biotechnology Information. What Is Osteosarcoma of the Skull and What.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!